Urinary tract infection (UTI) is the most common bacterial infection in childhood. UTI may be the sentinel event for underlying renal abnormality. There are still many controversies regarding proper management of UTI. In this review article, the authors discuss recent recommendations for the diagnosis, treatment, prophylaxis, and imaging of UTI in childhood based on evidence, and when this is lacking, based on expert consensus.
SourcesData were obtained after a review of the literature and a search of Pubmed, Embase, Scopus, and Scielo.
Summary of the findingsIn the first year of life, UTIs are more common in boys (3.7%) than in girls (2%). Signs and symptoms of UTI are very nonspecific, especially in neonates and during childhood; in many cases, fever is the only symptom.
ConclusionsClinical history and physical examination may suggest UTI, but confirmation should be made by urine culture, which must be performed before any antimicrobial agent is given. During childhood, the proper collection of urine is essential to avoid false-positive results. Prompt diagnosis and initiation of treatment is important to prevent long-term renal scarring. Febrile infants with UTIs should undergo renal and bladder ultrasonography. Intravenous antibacterial agents are recommended for neonates and young infants. The authors also advise exclusion of obstructive uropathies as soon as possible and later vesicoureteral reflux, if indicated. Prophylaxis should be considered for cases of high susceptibility to UTI and high risk of renal damage.
A infecção do trato urinário (ITU) é a infecção bacteriana mais comum na infância. A ITU pode ser o evento sentinela para alteração renal subjacente. Ainda há muitas controvérsias com relação ao tratamento adequado da ITU. Neste artigo de revisão, discutimos as últimas recomendações para diagnóstico, tratamento, profilaxia e imagiologia da ITU na infância, com base em comprovação e, na sua ausência, com base no consenso de especialistas.
Fonte de dadosOs dados foram coletados após uma revisão da literatura e pesquisa no Pubmed, Embase, Scopus e Scielo.
Resumo dos dadosNo primeiro ano de vida, as ITUs são mais comuns em meninos (3,7%) que em meninas (2%). Os sinais e sintomas da ITU são muito inespecíficos, principalmente em neonatos e durante a infância, sendo a febre o único sintoma em muitos casos.
ConclusõesO histórico clínico e exame físico podem sugerir ITU, porém a confirmação deve ser feita por urocultura. Antes da administração de qualquer agente antimicrobiano, deve ser feita coleta de urina. Durante a infância, a coleta de urina adequada é essencial para evitar resultados falso-positivos. O diagnóstico e início do tratamento imediatos são importantes na prevenção de cicatriz renal de longo prazo. Neonatos febris com ITUs devem ser submetidos a ultrassonografia renal e da bexiga, Agentes antibacterianos intravenosos são recomendados para neonatos e neonatos jovens. Recomendamos também a exclusão de uropatias obstrutivas o mais rápido possível e posterior refluxo vesico-ureteral, caso indicado. A profilaxia deve ser considerada em casos de elevada susceptibilidade a ITU e risco elevado de danos renais.
Urinary tract infection (UTI) is the most common bacterial infection in childhood,1–4 and up to 30% of infants and children experience recurrent infections during the first 6–12 months after initial UTI.5,6 UTIs may be the sentinel event for underlying renal abnormality, although normal anatomy is more common.7 Prompt diagnosis and initiation of treatment is important in preventing long-term renal scarring. However, increasing antibiotic resistance may delay initiation of appropriate therapy.
In young infants, symptoms of UTI differ from those in older children.8,9 The prevalence of UTI is higher in infants than in older children, with a male predominance.7,10,11 Most infections are caused by Escherichia coli, although, in the first year of life, Klebsiella pneumoniae, Enterobacter spp., Enterococcus spp., and Pseudomonas spp. are more frequent than later in life, and there is a higher risk of urosepsis compared with adulthood.7,8,10–12
In 30% of children with congenital anomalies of the kidney and urinary tract (CAKUT), UTI can be the first sign.13 If pediatricians fail to identify patients at risk, the upper urinary tract may be damaged. Up to 85% of infants and children with febrile UTI may have visible alterations on technetium Tc 99-labeled dimercaptosuccinic acid (DMSA) scanning. Of these children, 10–40% have permanent renal scarring,14–16 which may lead to poor renal growth, recurrent pyelonephritis, impaired glomerular function, early hypertension, and, eventually, end-stage renal disease.14,15,17–20
Therefore, identifying children at risk of renal parenchymal damage and follow-up imaging after UTI is a very difficult task. Furthermore, the use of antibiotic prophylaxis also remains controversial. In this review article, the authors discuss recent recommendations for the diagnosis, treatment, prophylaxis, and imaging of UTI in childhood based on evidence, and when this is lacking, based on expert consensus.
Urinary tract infection in pediatrics: general considerationsThe incidence of UTIs depends on age and sex. In the first year of life, UTIs are more common in boys (3.7%) than in girls (2%). This is even more pronounced in febrile infants in the first 2 months of life, with an incidence of 5% in girls and 20.3% in uncircumcised boys, as demonstrated in one prospective study including over 1000 patients using urine specimens obtained by catheterization.10 Later, the incidence changes, and approximately 3% of prepubertal girls and 1% of prepubertal boys are diagnosed with UTI.10,11,13
The first step for the diagnosis of UTI is medical history. Indeed, the patient's history normally allows for the identification of the site, episode, symptoms, and complicating factors.7,9,11,12 This includes questions on primary or secondary infection, febrile or non-febrile UTIs; history of malformations of the urinary tract (e.g., pre- or postnatal ultrasound [US] screening); previous surgeries; drinking and voiding habits; family history; whether there is constipation or presence of lower urinary tract symptoms; and sexual history in adolescents.
Signs and symptoms of UTI are very nonspecific, especially in neonates and during childhood. Fever may be the only symptom of UTI, especially in young children.1,21–23 Newborns with pyelonephritis or urosepsis can present nonspecific signs and symptoms, sometimes without fever.24,25 Septic shock is unusual, even with high fever,26 unless obstruction is present or the patient is otherwise compromised. In older children, lower urinary tract symptoms include dysuria, frequency, urgency, malodorous urine, incontinence, hematuria, and suprapubic pain; for the upper urinary tract, fever and flank pain. A complete pediatric physical examination is always required to exclude any other source of fever. Conversely, if the fever has no apparent cause, UTI should always be discarded.3,4,11 Physical examination should search for signs of constipation, palpable and painful kidney, palpable bladder (stigmata of spina bifida or sacral agenesis spine and feet), genital disorders (phimosis, labial adhesion, urethral meatal stenosis, abnormal urogenital confluence, cloacal malformations, vulvitis, and epididymo-orchitis), and measure temperature.
According to site of predominant alteration, UTI may be classified as cystitis or pyelonephritis. Cystitis is inflammation of the urinary bladder mucosa, with symptoms of lower urinary tract infection.7,8,12 However, in newborns and infants, these symptoms are rarely diagnosed accurately.7 In pyelonephritis, the bacteria have ascended through the upper urinary tract to the kidneys, causing inflammation that could lead to renal damage or deterioration of preexisting scars. In children with dilating vesicoureteral reflux (VUR), there is a strong correlation between febrile UTI recurrence and renal scarring.27 Apart from the risk of developing renal damage, every symptomatic UTI causes discomfort and distress, which is enough to justify the effort to reduce recurrences.28 It should be also mentioned that the introduction of antenatal screening for malformations with ultrasonography has made the detection of urinary tract abnormalities possible before any infections have occurred.29–31
E. coli is the predominant pathogen in childhood UTI, found in 90% of girls and in 80% of boys at the first episode of UTI.2,3,8,12,32 An important factor for the predominance of E. coli is the ability of this pathogen to attach to the urinary tract endothelium. The preputial area is colonized by non-E. coli Gram-negative bacteria in uncircumcised boys, hence the different bacterial spectrum in male UTI. In recurrent infections, the proportion of non-E. coli is higher than Klebsiella spp., enterococci, Enterobacteriaceae, and Proteus spp. If urine culture yields unusual bacteria, follow-up investigations will often disclose CAKUT.8,31,32 Atypical species are also more commonly observed in infections secondary to invasive procedures or indwelling catheters. UTI following antibiotic treatment for other infections is also more frequently caused by non-E. coli species, as repeated antibiotic treatment has the potential to select atypical pathogens.8,31–33
Urinary tract infection in infancy: specific aspectsAs already mentioned, the clinical presentation of UTI is heterogeneous, varying according to age group and location of the infection.34 Other factors may also influence clinical manifestations of UTI, such as nutritional status, presence of abnormalities of the urinary tract, number of previous infections, and the time interval from the last episode. The clinical picture may vary from isolated fever or changes in urinary habits to acute pyelonephritis, which may lead to urosepsis, especially in infants.35
In newborns, UTI may manifests as sepsis, predominantly with nonspecific signs and symptoms, including insufficient weight gain, anorexia, vomiting, poor sucking, irritability, lethargy, convulsions, and hypothermia. It may also present with less acute symptoms, such as food refusal, occasional vomiting, pallor, and jaundice.36 The American Academy of Pediatrics recommends that infants with elevated direct bilirubin levels should be screened for UTIs. However, those with elevated unconjugated bilirubin levels should not be excluded, especially if other concerning clinical features are present.37 As with most infections, in this age group, there is high probability of bacteremia, suggesting hematogenous bacterial spread. There is a high rate of mortality (around 10%), and many of these deaths are due to the spread of infection to another sites, leading to meningitis, for instance.38
In infants, fever is the main symptom, and often the only sign of infection. Rarely, there are signs or symptoms related to the urinary tract, such as urinary frequency, dysuria, foul-smelling urine, and back pain. However, high temperature associated with nonspecific manifestations, such as appetite loss, vomiting, abdominal pain, dehydration, and poor weight gain are commonly found in infants with UTI.34–36
The physical examination should be complete, covering nutritional aspects, growth, and psychomotor development. Careful palpation of abdominal flanks may reveal increased renal volume (a symptom of severe hydronephrosis or cystic kidneys, for example). The persistence of palpable bladder after micturition suggests obstructive process or lower urinary tract dysfunction. In infants, the lumbar percussion may rarely show strong painful reaction (positive Giordano).34–36 Particularly in this age group, the observation of the urine stream, during the physical examination, is helpful. A weak or dripping stream arises the possibility of low urinary tract obstruction, such as posterior urethral valves in boys.39
A thorough examination of the external genitalia is mandatory in neonates and infants. It is essential to evaluate anatomical conformation, specifically the appearance and location of the urethral meatus and narrowing of the foreskin, which prevent the exposure of the urethral meatus in boys. It is important to rule out the presence of vulvovaginitis or balanoposthitis that can lead to a false-positive laboratory diagnosis of UTI. Constant and/or uncontrollable loss of urine, especially when observed during the physical examination, suggests ectopic ureter. A careful examination of spine column is also indispensable, searching for abnormalities on spinal curvature/symmetry and evidence of spina bifida occulta or pilonidal sinus hidden by creases or dimples.11
The diagnosis of UTI in infants is based on clinical and laboratorial findings, including detailed clinical history and physical examination. In the anamnesis, in addition to specific symptoms of UTI, it is important to inquire about bowel habits (constipation and fecal leaks), characteristics of the urinary stream, and general symptoms associated (fever, vomiting, diarrhea, stunted weight gain). History of the pregnancy should also be investigated, including prenatal sonographic findings, such as fetal hydronephrosis and other clues for CAKUT, neural tube disorders, and amniotic fluid volume. The family history should include questions about CAKUT in relatives, such as VUR, obstructions of the urinary tract, and cystic renal diseases.
UTI in childhood: practical approachDiagnosisDiagnosis and management of UTI is one of the most—if not the most—controversial areas of pediatrics. One factor contributing to the current situation is the unexpected difficulty in diagnosing UTI in infants. Substantial over- and under-diagnosing can result from practical difficulties in at least three areas, including problems with urine sample collection, issues in interpreting bacterial counts correctly, and misdiagnosis between infantile asymptomatic bacteriuria and true symptomatic febrile UTI.40
Clinical history and physical examination may suggest the diagnosis of UTI, but confirmation should be made by urine culture, which will show the proliferation of microorganisms in the urinary tract.41 Therefore, before any antimicrobial agent is given, urine culture must be performed.11 During infancy, the proper collection of urine is essential to avoid false-positive results; it should be done after cleaning the genital area with water and soap without antiseptic agents.40 In newborns, infants, and non-toilet-trained children, there are four main methods for obtaining urine, with varying contamination rates and invasiveness.11 A plastic bag attached to the cleaned genitalia is the technique most often used in daily practice.42 Although a culture-negative urine bag sample is reliable, this technique has high rate of false-positive cultures due to contamination by periurethral flora.43 McGillivray et al. 44 compared the validity of the urinalysis on clean-voided bag versus catheter urine specimens using the catheter culture as the gold standard in a cross-sectional study of 303 non toilet-trained children under age 3 years at risk of UTI who presented to a children's hospital emergency department. Bag dipstick was more sensitive than catheter dipstick for the entire study sample: 0.85 versus 0.71, respectively. Conversely, specificity was consistently lower for the bag specimens than for the catheter specimens: 0.62 versus 0.97, respectively.
For clean-catch urine collection, the infant is placed in the lap of a parent or nurse holding a sterile foil bowl underneath the infant's genitalia. There is a good correlation between results of urine culture obtained by this method and by suprapubic bladder aspiration.45 However, a study with 120 infants and children observed a 25% contamination rate with samples from clear-voided urine compared to samples from suprapubic aspiration.46
Suprapubic bladder aspiration (SPA) is the most sensitive method for obtaining an uncontaminated urine sample. When urine is collected by suprapubic aspiration, a method that bypasses the urethra, any colony count is considered to represent significant bacteriuria. All other methods of urine collection (mid-stream clean catch, catheterization, and bag collections) require passage of urine through the urethra. SPA has been considered the gold standard for obtaining urine that is uncontaminated by perineal flora. Variable success rates for obtaining urine have been reported (23–90%),37 increasing when ultrasonography guidance is used.47 The technique has limited risks, but technical expertise and experience are required, and many parents and physicians perceive the procedure as unacceptably invasive. However, there may be no acceptable alternative to SPA for boys with severe phimosis, girls with tight labial adhesions, presence of external genital infection, or presence of genital complex abnormalities.
Bladder catheterization may be an alternative to SPA, although the rates of contamination are higher. Urine obtained through catheterization for culture has a sensitivity of 95% and a specificity of 99% when compared with that obtained through SPA.48
In order to choose a particular method, it is important to consider the clinical condition of the patient, the experience of healthcare team, and the resources of the pediatric or urgency center facilities.
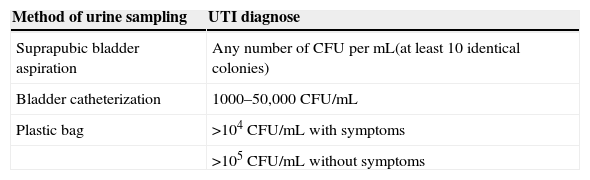
The definitive diagnosis of UTI in infants is a continuous challenge for physicians, and a judicious interpretation of tests results is mandatory. In urine analysis, dipstick tests for nitrite, leukocyte esterase, protein, glucose, and blood is very useful.49 A dipstick test that is positive for leukocyte esterase and nitrite is highly sensitive for the diagnose of UTI. A test that is negative for leukocyte esterase and nitrite is highly specific for discarding UTI.49 In urine culture, the classical definition of >105CFU/ml of voided urine is still used to define significant UTI. It is well established that different cut-off levels are used for bag cultures, SPAs, and cultures from catheterized samples (see Table 1, adapted from Stein et al.).11 The recent American Academy of Pediatrics (AAP) Guidelines on UTI suggest that the diagnosis should be based on the presence of both pyuria and at least 50,000CFU/mL in an SPA sample. Mixed cultures indicate contamination.37
Criteria for diagnosing urinary tract infection (UTI) in children.
| Method of urine sampling | UTI diagnose |
|---|---|
| Suprapubic bladder aspiration | Any number of CFU per mL(at least 10 identical colonies) |
| Bladder catheterization | 1000–50,000 CFU/mL |
| Plastic bag | >104CFU/mL with symptoms |
| >105CFU/mL without symptoms |
CFU, colony-forming units.
In infants, C-reactive protein and blood cell counts should be obtained for monitoring ill patients with febrile UTI. In addition, in a severely ill child, renal function and blood cultures should also be taken. For infants with febrile UTI, US imaging of the urinary tract can be very useful during the acute phase, for instance, to promptly identify an obstructive uropathy. Early US examination is also indicated in children with suspected urosepsis, palpable abdominal masses, hematuria, and for patients without response to the standard management.11,37
TreatmentIn febrile children with signs of UTI (clinical signs, positive dipstick, and/or positive microscopy), antibiotic treatment should be initiated as soon as possible to eradicate the infection, prevent bacteremia, improve clinical outcome, diminish the likelihood of renal involvement during the acute phase of infection, and reduce the risk of renal scarring. As previously stated, before any antibiotic therapy is started, a urine specimen should be obtained for urinalysis and urine culture.50
Proper treatment includes the relief of symptoms, eradication of the infectious agent, and identification of patients at high risk of developing lesions in the renal parenchyma. For relief of symptoms, analgesic and antipyretic drugs should be prescribed at usual doses. In neonates and young infants, physicians should be watchful for early detection of signs or symptoms of urosepsis, septic shock, or hypovolemic status. For patients with low oral intake or with dehydration, rehydration must be readily provided, if necessary, via parenteral route.11,43
Empiric therapy for neonates and young infants with UTI and sepsis are similar because of common etiology. Therefore, as a result of the high incidence of urosepsis and severe pyelonephritis in newborns and infants <3 months of age, parenteral antibiotic therapy is always recommended. Otherwise, when choosing between oral and parenteral therapy, some factors should be considered: patient age, severity of illness, refusal of oral intake, vomiting, noncompliance with oral medication, and potential complicated febrile UTI (for instance, severe urinary tract dilatation).7,11,37,51 A multicenter randomized controlled trial by Montini et al.52 demonstrated that oral therapy was as effective as intravenous therapy followed by oral therapy for managing the first UTI episode.
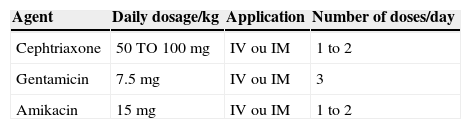
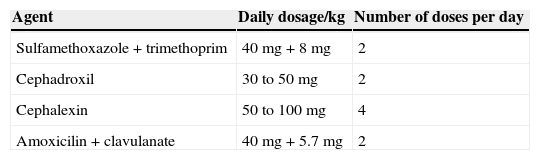
Traditionally, intravenous antibiotics are started once appropriate cultures are obtained. A combined treatment with ampicillin and an aminoglycoside or a third-generation cephalosporin usually achieves excellent therapeutic results.53 The choice of agent is also based on local antimicrobial sensitivity patterns and can be later adjusted, according to sensitivity testing of the isolated pathogen. Tables 2 and 3 present a scheme of frequently used parenteral and oral agents, respectively, for the treatment of UTI in infants. Most infections are caused by E. coli, although during the first year of life, K. pneumoniae, Enterobacter spp., Enterococcus spp., and Pseudomonas spp. are more frequent than later in life. In infants with urinary tract abnormalities, there is also a higher prevalence of “atypical” bacteria.36
Improvement of the general clinical condition and the reduction of fever within 48–72h are indicative of good response to treatment with antibiotics. Conversely, in patients with prolonged fever and failing recovery, treatment-resistant uropathogens and the presence of congenital uropathy or acute urinary obstruction should be considered; an US examination is highly advisable. Temporary urinary diversion may be required in infants with obstructive uropathy or with severely dilated urinary tract, in case of non-response to antibiotic therapy and/or worsening on clinical status.11
Very few studies have evaluated the duration of treatment and the transition from parenteral to oral therapy in infants. In the premature infant, the bioavailability of most antibiotics is not known; therefore, intravenous therapy is typically preferred. Documentation of negative blood and cerebral spinal fluid cultures in both premature and young infants is advisable.7 In older infants, Benador et al. 54 observed that the risk of renal scarring was not different between infants that received three days of parental therapy followed by seven days of oral therapy when compared with 10 days of oral therapy. Thus, in older and more mature infants, three to four days of parental therapy followed by transition to oral medications to complete a 7- to 14-day course of treatment can be used. If outpatient management and oral therapy are chosen, close surveillance and medical supervision are critical in the initial phase of therapy; treatment should be adjusted when necessary.
Preventing UTI recurrence: prophylaxisApproximately 20% of children who have had one UTI experience a symptomatic recurrence.55 Preventing UTI recurrence would avoid further episodes of illness, discomfort, and family stress.26 There are many studies on prophylaxis with contradictory results and divergent conclusions, but only a few of them are properly randomized and controlled. Evidence regarding the efficacy of prophylactic therapy to prevent recurrences after the first episode of UTI is lacking for the infant population.56,57
A long-term follow-up of 71 infants with UTI showed a recurrence rate of 28%. Most of the episodes of recurrence (65%) occurred in the first six months after the initial UTI, and 75% occurred in patients without any renal abnormalities.25 A recent study compared infants with VUR and recurrent UTI (mean age: 3.2 months) and without recurrent UTI (mean age: 4.8 months). The authors demonstrated that, during the first year of life, the earlier the first UTI occurs, the higher the chance of recurrence. Higher grades of reflux, bilateral VUR, and the first infection not caused by E. coli significantly increased the risk of recurrent UTIs.58
Although some prospective randomized studies have questioned the efficacy of antibacterial prophylaxis, recent well-designed trials have shown that some subgroup of patients clearly benefits from prophylaxis.27 For instance, the Swedish reflux study clearly demonstrated that chemoprophylaxis is effective in preventing new renal scars in infant girls with moderate/severe reflux.59,60 Craig et al. have shown, in a large placebo-controlled trial in Australia, that long-term, low-dose trimethoprim–sulfamethoxazole was associated with a decreased number of UTI episodes in predisposed children.55 During the study, 36 of 288 patients (13%) developed UTI in the group receiving trimethoprim–sulfamethoxazole (antibiotic group), versus 55 of 288 patients (19%) in the placebo group (hazard ratio in the antibiotic group, 0.61; 95% confidence interval, 0.40–0.93). In fact, the treatment effect appeared to be consistent across subgroups, including for younger children. The recently published Randomized Intervention for Children with Vesicoureteral Reflux (RIVUR) trial with 607 children (280 with a reflux I or II and 322 with a reflux III or IV) showed that antimicrobial prophylaxis with trimethoprim/sulfamethoxazole reduced the risk of recurrence by 50%.61
Good quality evidence for prophylaxis in very young children is limited, because there are not specific randomized controlled trials for this age group. Nevertheless, there is a clear benefit of prophylaxis for some subgroups and long-term low dose antibacterial administration should be considered in cases of high susceptibility to UTI and high risk of acquired renal damage. In this context, the prophylaxis should be considered in the following clinical situations: (1) presence of prenatal sonographic findings suggestive of uropathies; (2) until the imaging investigation of the urinary tract has been completed; (3) in the presence of severely dilated urinary tract; (4) in the presence of obstructive uropathy until surgical correction; and (4) in the presence of VUR grades III to V. The aim of prophylaxis in these situations is to prevent recurrent UTI and/or renal damage.
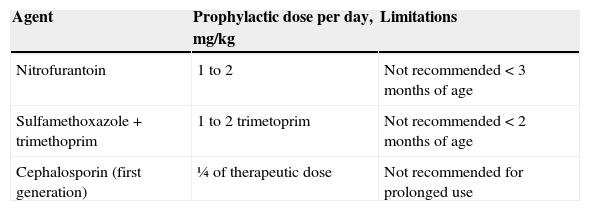
Continuous prophylaxis with low-dose antibiotics given for a variable period time has been the cornerstone of this approach.27 The usual choices for prophylaxis include trimethoprim-sulfamethoxazole and nitrofurantoin (Table 4). The use of cephalosporins for chemoprophylaxis should be considered during the first two months of age, due to possible side effects of both trimethoprim-sulfamethoxazole and nitrofurantoin in neonates and infants aged less than 3 months. In spite of the current controversy regarding the efficacy of prophylaxis, this approach is advisable for selected subgroups of patients. In these cases, prophylaxis can protect from recurrent UTI and possible long-term sequelae.
Options of antibacterial prophylaxis for urinary tract infection recurrences.
| Agent | Prophylactic dose per day, mg/kg | Limitations |
|---|---|---|
| Nitrofurantoin | 1 to 2 | Not recommended<3 months of age |
| Sulfamethoxazole+trimethoprim | 1 to 2 trimetoprim | Not recommended<2 months of age |
| Cephalosporin (first generation) | ¼ of therapeutic dose | Not recommended for prolonged use |
Widespread use of prenatal US clearly has reduced the prevalence of previously unsuspected CAKUT in infants.37,62 However, the impact of prenatal screening on the prevalence of renal abnormalities in infants with UTIs has not been well studied yet. It is important to highlight that the quality of prenatal sonograms is extremely heterogeneous and a report of “normal” fetal sonographic examination cannot rule out the possibility of structural abnormalities.37,62
Two recent guidelines on urinary tract infections in children, by the AAP and the European Association of Urology (EAU), stated consensually that febrile infants with UTIs should undergo renal and bladder US (RBUS).27 The aim of RBUS is to detect anatomic abnormalities that require further evaluation, such as additional imaging or urologic procedure. RBUS also provides an evaluation of the renal parenchyma and an assessment of kidneys size.63 These features help establishing a tailored approach to monitor these patients. Nevertheless, some caution must be taken in the interpretation of ultrasonography findings. The method has intrinsic limitations and it is highly observer-dependent. For instance, RBUS has low sensitivity in detecting VUR and cannot exclude the presence of even high levels of this uropathy, although it may show indirect signs of their presence.64–66 Conversely, renal US is a very useful screening test for obstructive uropathies and other structural abnormalities, is relatively inexpensive, non-invasive, and usually readily available. As stated earlier, the timing of RBUS depends on the clinical status and on the course of treatment. RBUS is recommended early when there is suspect of complicated febrile UTI (e.g., renal abscesses, pyonephrosis, and structural abnormalities) or in patients without clinical improvement. It must be pointed out, however, that an acute renal parenchyma infection may cause transitory alterations, such as urinary tract dilatation and changes in the echogenicity of renal parenchyma.37
The AAP guideline recommends that voiding cystourethrogram (VCUG) should not be performed routinely after the first febrile UTI. VCUG is indicated if RBUS reveals hydronephrosis, scarring, or other findings that suggest either high-grade VUR or obstructive uropathy.37 Conversely, the EAU guideline recommends that, for infants under 1 year, VUR should be excluded by VCUG and/or DMSA scan. In addition, this guideline suggests a similar approach for girls above 1 year of age, but not for boys above this age. For boys older than 1 year, this guideline recommends only RBUS. VCUG should be performed after the UTI has been treated.11 Indeed, two possible imaging strategies have been recommended for the diagnosis of VUR: the bottom-up method (VCUG and, if positive, a DMSA scan) or the top-down method (DMSA scan and, if positive, VCUG).67,68
Therefore, currently there is no consensus regarding the best imaging approach after the first episode of febrile UTI. In this context, Williams et al. suggest a simpler and direct approach: (1) renal tract sonography in all children, and (2) voiding cystography and/or DMSA for children with abnormal renal tract sonography.50
Concluding remarksThe proper management of UTI is one of the most controversial areas in pediatrics. Nowadays, the classification of a UTI is made according to the site, episode, symptoms, and complicating factors. For acute treatment, the site and severity are of the most important factors. Treatment of patients with febrile UTIs should be initiated after urine analysis and culture to confirm the diagnosis. SPA and catheterization presents the lowest contamination rate for urine sampling, while plastic bag remains the most commonly used method in daily practice. UTI can be excluded if the dipstick is negative for both leukocyte esterase and nitrite, or if the microscopic analysis is negative for both pyuria and bacteriuria. In neonates and young infants, intravenous antibiotics are usually recommended for the treatment of febrile UTI. The improvement of general clinical condition and the reduction of fever are indicative of good response to treatment with antibiotics. Prophylaxis has been shown to be beneficial when prenatal sonographic findings are suggestive of uropathies, until the imaging investigation has been completed, in the presence of severely dilated urinary tract, of obstructive uropathy (until surgical correction), and of vesicoureteral reflux grades III to V. In these situations, prophylaxis aims to prevent recurrent UTI and/or renal damage. There is still no consensus regarding the best imaging approach after the first episode of febrile UTI. Early ultrasonography of the kidney and bladder are necessary in young patients with febrile UTI to exclude underlying uropathy. Longitudinal prospective studies are still needed to establish tailored protocols for the approach of UTI in childhood.
FundingThis study was partially supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq, Brazil) and Fundação de Amparo à Pesquisa do Estado de Minas Gerais (FAPEMIG, Brazil). Dr. AC Simões e Silva and Dr. EA Oliveira received a research grant from CNPq.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Simões e Silva AC, Oliveira EA. Update on the approach of urinary tract infection in childhood. J Pediatr (Rio J). 2015;91:S2–10.