This study examined the mediation role of psychological morbidity, defined in this study as depression/anxiety, in the relationship between excessive daytime sleepiness and sleep quality, and between sleep habits and health behaviors, in adolescents.
MethodsA total of 272 students, between 12 and 18 years old, underwent a psychological protocol assessing excessive daytime sleepiness, sleep quality, sleep habits, health behavior, and psychological morbidity.
ResultsPsychological morbidity was not associated with the relationship between excessive daytime sleepiness and sleep quality, but was associated, with statistical significance, in the relationship between sleep habits and health behaviors. These results emphasize the role of psychological morbidity in adolescent health behaviors.
ConclusionAnalyzing the symptoms of depression and anxiety in pediatric patients may help in a more accurate diagnosis, especially in relation to sleep problems and health behaviors.
Este estudo analisa o papel mediador da morbidade psicológica, definida neste estudo como depressão e ansiedade, na relação entre a sonolência diurna excessiva e qualidade do sono, e entre hábitos de sono e comportamentos de saúde, em adolescentes.
Método272 Estudantes, entre 12 e 18 anos, foram entrevistados através de um protocolo de avaliação que acessou dados acerca da sonolência diurna excessiva, qualidade do sono, hábitos de sono, comportamentos de saúde e morbidade psicológica.
ResultadosOs resultados mostraram que a morbidade psicológica não estava associada, com significância estatística, na relação entre a sonolência diurna excessiva e qualidade do sono, mas estava associada, com significância estatística, na relação entre hábitos de sono e comportamentos de saúde. Esse resultado reforça a importância da morbidade psicológica nos comportamentos de saúde dos adolescentes.
ConclusãoInvestigar sintomas de depressão e ansiedade nas consultas pediátricas, pode auxiliar o profissional num diagnóstico mais preciso, principalmente em relação a problemas de sono e comportamentos de saúde.
Adolescence is marked by several biopsychosocial changes. Adolescence is also a period where sleep undergoes several structural changes, which may cause problems in sleep quality, and consequently, a negative impact in several areas of an adolescent's life, including mental health.1 It is known that sleep is essential for the proper functioning and maintenance of life,2 and recently it was concluded that a major function of sleep is to allow neurons to perform cell maintenance.3 Despite this complex function, adolescents are sleeping less than what was expected.4 This reduction in quality and time of sleep may be due to several factors, including poor sleep habits and poor health behaviors, which can lead to negative consequences, such as excessive daytime sleepiness.
The lack of healthy sleep habits has been commonly observed in studies with adolescents. One of the factors that is closely linked with the decline of healthy sleep habits is the use of electronics, which have a large negative impact on adolescent's sleep quality5 since they are one of the main distractions that compete with sleep. However, the problem may worsen when beyond the use of electronics, adolescents make use of psychoactive substances, such as caffeine drinks to stay awake longer, which have an impact on sleep quality and on daytime sleepiness.6 This type of behavior may become a vicious cycle, i.e., the adolescent needs to wake up early to go to school, will show daytime sleepiness (reduced sleep time), and thus needs caffeinated beverages to help to stay awake during class.
The literature shows a connection between excessive daytime sleepiness and sleep deprivation.7 Moreover, a systematic review found a strict relationship between sleep problems and health risk behaviors, such as consumption of psychoactive substances and unprotected sex.8 Furthermore, sleep problems were connected with emotional and behavior problems among adolescents.8 Previous studies have found that adolescents with less hours of sleep showed higher levels of depressive symptoms and higher prevalence of anxiety disorders.9 Literature has also found high rates of comorbidity among adolescents that have sleep problems and depression, i.e., adolescents who suffer from sleep disorders also show depressive disorders concomitantly.5
A recent study found that when young students had a few hours of sleep during the week, there was considerably more self-reports of complaints regarding anxiety and tension.10 A meta-analysis found that 20% of adolescents suffers from depression and sleep problems.11 Literature has found a relationship between psychological morbidity (depression and anxiety solely or combined) and adolescents’ sleep disturbances. Psychological morbidity is the distress caused by the lack of physical and psychological well-being, which has an impact on the individual's health. In the present paper, the term psychological morbidity includes the combination of depression and anxiety.12
According to the Stress-Coping Model from Maes et al.13 illness related events, disease treatment, and demographic characteristics are linked with emotional and cognitive responses as well as coping, predicting psychological, physical, and social consequences of illness. Coping is also influenced by the individual's internal and external resources. Based on the Stress-Coping Model, in this study, emotional response was analyzed as psychological morbidity, the health related event considered was excessive daytime sleepiness, and the psychological consequences included both sleep quality and health behaviors. Sleep habits were considered an internal resource that, through coping, could also influence health behaviors. With these goals in mind, the focus of this research was to analyze the plausible mediation role of psychological morbidity in the relationship between excessive daytime sleepiness and sleep quality, as well as the mediation role of psychological morbidity in the relationship between sleep habits and health behaviors.
MethodsParticipantsTwo public schools in the north of Portugal agreed to participate in this research. The sample was composed of adolescents aged 12–18 years of both genders. The inclusion criteria included age 12 to 18 years old, completed authorization by the parents, and being present in the application day, in the class. There were no exclusion criteria.
MeasuresPittsburgh Sleep Quality Index (PSQI).14 This instrument assesses sleep quality during the previous month and includes 19 items. The PSQI is composed of seven components that evaluate daytime dysfunction, sleep medication, sleep disturbances, sleep efficiency, sleep duration, sleep latency, and sleep quality. Higher scores indicate worse sleep quality. In this study, only the total scale was used, and Cronbach's alpha was 0.60.
Sleep Habits Questionnaire (SHQ).15 This 12-item questionnaire assesses the impact of behaviors that may influence sleep in adolescents (e.g.: how many times a week do you play video-games after bedtime, how many times a week do you read, study, or do homework after bedtime). Cronbach's alpha, in this sample, for the total scale was 0.70.
Modified Excessive Sleepiness Scale (MESSA).16 The instrument assesses the propensity of adolescents to fall asleep in different situations, and is composed of 13 items. A higher score indicates the presence of excessive daytime sleepiness. In this study, Cronbach's alpha for the total scale was 0.78.
Hospital Anxiety and Depression Scales (HADS).17 This instrument assesses the levels of depression and anxiety. It has 14 items that provide a psychological morbidity global scale with two subscales (anxiety and depression). The cutoff score for clinical depression and anxiety is 8, according to the authors. The sum of the two subscales provides a score of psychological morbidity. In this study, only the total scale was used. Cronbach's alpha, in this sample, was 0.76.
Health Behaviors Questionnaire (HBQ).18 This 24-item instrument assesses health behaviors such as exercising, healthy diet, oral hygiene, and regular medical checkups. A higher score indicates healthier behaviors. In this study, Cronbach's alpha for the total scale was 0.70.
ProcedureThe study was approved by the General Education Committee. Data was collected in two public high schools in the North of Portugal. Within each school, class directors who agreed to participate offered one of their class periods for students’ participation. Parents signed an informed consent regarding their adolescent's voluntary participation. The self-administered questionnaires were completed during the class period, by one of the researchers.
Data analysisThe calculation of sample size was based on Tabachnick and Fidell formula.19 The measurements were performed using the bootstrapping method.20 Bootstrapping is a non-parametric statistical method, where it is possible to achieve more accurate confidence intervals than conventional methods. Parameter estimates were based on 3000 bootstrap samples. The bias corrected and accelerated 95% confidence intervals were then examined, and if the confidence intervals did not contain zero, the indirect effect was considered significant at p<.05.
ResultsThe sample was composed of 272 high school adolescents, between 12 and 18 years old (mean=15.48, SD=1.61), 58% female, 90% white. Of the total sample, 31% consumed one to two cups of coffee/day and 23% consumed energy drinks. In addition, 79% of the adolescents had married parents and 35% reported having a family member with sleep problems. Adolescents reported that 73% of their fathers drank alcohol, as well as 51% of their mothers. In addition, 31% of fathers and 15% of mothers smoked.
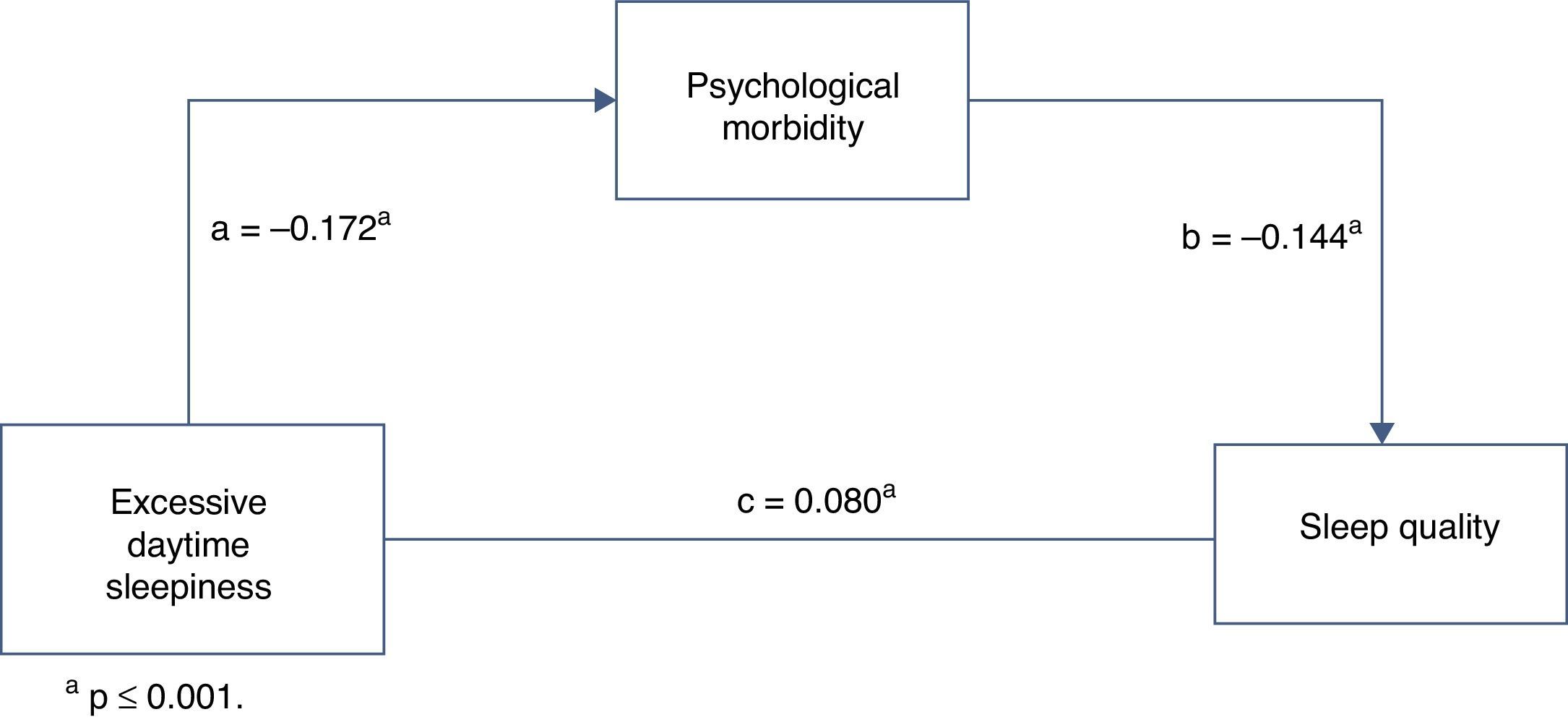
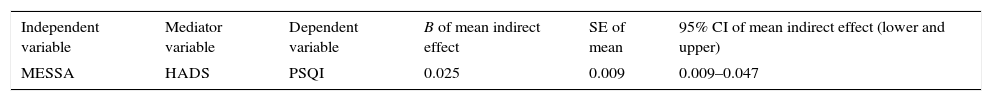
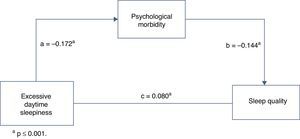
Psychological morbidity as a mediator in the relationship between excessive daytime sleepiness and sleep qualityThe indirect effect of excessive daytime sleepiness on sleep quality was not mediated by psychological morbidity (95% CI=0.009–0.047, p=ns) (Table 1, Fig. 1).
Bootstrap analyses of the statistical and magnitude significance of indirect effect.
| Independent variable | Mediator variable | Dependent variable | B of mean indirect effect | SE of mean | 95% CI of mean indirect effect (lower and upper) |
|---|---|---|---|---|---|
| MESSA | HADS | PSQI | 0.025 | 0.009 | 0.009–0.047 |
MESSA, Modified Excessive Sleepiness Scale; HADS, Hospital Anxiety and Depression Scale; PSQI, Pittsburgh Sleep Quality Index.
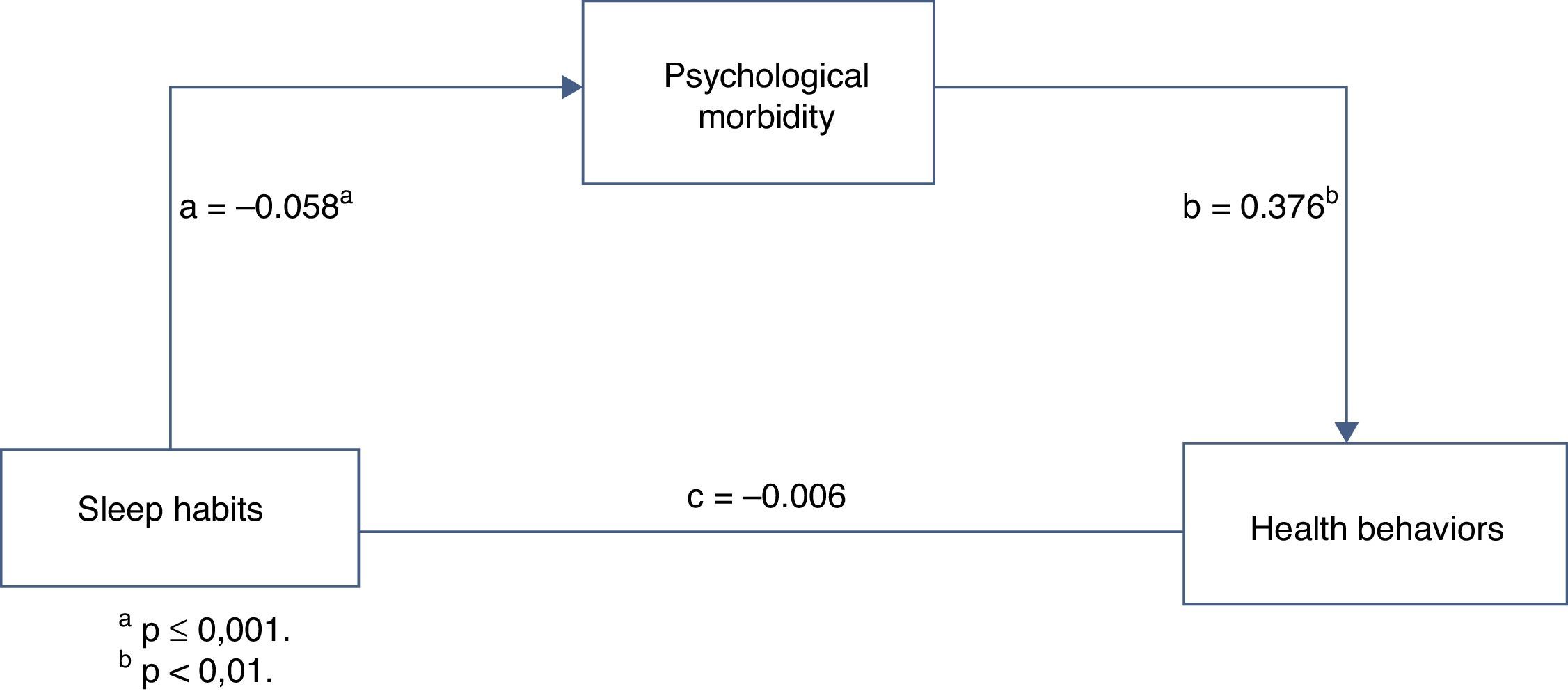
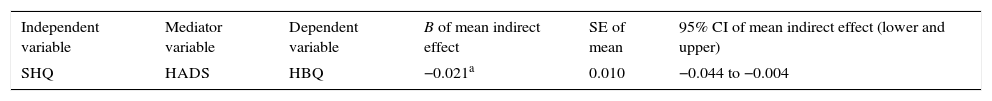
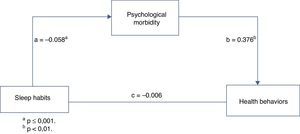
Psychological morbidity was a significant mediator in the relationship between sleep habits and health behaviors (95% CI=−0.044 to −0.004, p=.02) (Table 2, Fig. 2).
Bootstrap analyses of the statistical and magnitude significance of indirect effect.
| Independent variable | Mediator variable | Dependent variable | B of mean indirect effect | SE of mean | 95% CI of mean indirect effect (lower and upper) |
|---|---|---|---|---|---|
| SHQ | HADS | HBQ | −0.021a | 0.010 | −0.044 to −0.004 |
SHQ, Sleep Habits Questionnaire; HADS, Hospital Anxiety and Depression Scale; HBQ, Health Behavior Questionnaire.
The first aim of the present study was to analyze whether psychological morbidity (depression and anxiety) was a mediator in the relationship between excessive daytime sleepiness and sleep quality in adolescents. The indirect effect of excessive daytime sleepiness on sleep quality was not mediated by psychological morbidity. This result was surprising, because as previously described, sleep is related to psychological morbidity in adolescents and mood disorders.21 Studies have found a bidirectional relationship between psychological morbidity, mental health, and sleep quality.22,23 Another study comparing depressed adolescents with control groups, using EEG, reported inconsistent conclusions in terms of sleep patterns.24 The authors concluded that negative rumination and distress at bedtime, in adolescents, further accentuated the interaction between psychological morbidity and insomnia. Anxiety disorders tend to follow the same patterns as depression regarding sleep problems. In fact, adolescents with anxiety disorders complain about nighttime awakening and difficulty in falling asleep.24 However, according to some longitudinal studies, sleep problems predict psychological morbidity, but the converse is not true.11 The present results are in accordance with those studies, showing no causal effect between psychological morbidity and sleep quality.
Psychological morbidity was a mediator in the relationship between sleep habits and health behaviors. Past studies found a strong relationship between psychological morbidity and internet addiction,25 and between watching media (television, computer games, internet) and sleep patterns.26 Furthermore, behaviors such as alcohol consumption were also associated with sleep problems (e.g. insomnia),27 and consumption of caffeine has been associated with the use of electronics, showing an impact on the sleep quality of the adolescent.6 Sleep disorders imply a risk not only for mental health, but also for physical morbidity.28 Furthermore, psychological morbidity (depression/anxiety), drug consumption, and behavioral problems are difficulties often reported by adolescents with disturbed sleep.29 Therefore, it comes as no surprise that psychological morbidity plays a mediator role in the relationship between sleep habits and health behaviors. Sleep restriction may have multiple risk factors; the cumulative burden of these factors may affect the chronicity and the frequency of sleep problems more intensively.30
This study has several limitations that need to be acknowledged. The sample was only from the North of the country, which limits the generalization of the findings. Cronbach's alpha of the PSQI was satisfactory, but low. Furthermore, the sample included only high school adolescents. Future longitudinal studies should pursue how psychological morbidity plays a role in the adolescent's lifestyle, and in the development of sleep disturbances.
The current study highlights the importance of psychological morbidity, sleep habits, and health behaviors in adolescents. According to the results, psychological morbidity has an important mediator role between sleep and adolescent's health behaviors. The awareness of health professionals in detecting symptoms of depression and anxiety should be taken in consideration in pediatric visits, particularly when sleep problems and health risk behaviors are involved.
FundingThe present research was supported by Erasmus Mundus 15.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Pucci SHM, Pereira MG. The mediator role of psychological morbidity on sleep and health behaviors in adolescents. J Pediatr (Rio J). 2016;92:53–7.