To verify the temporal trends of the indicators of overall mortality and hospital morbidity due to diarrheal disease in children younger than 1 year and between 1 and 4 years, according to the region of Brazil, between 2000 and 2010.
MethodThis was an ecological study of temporal series. Data on hospital admission authorization, mean length of stay, and mean value of the authorization were obtained from the Hospital Information System. The number of infant deaths was obtained from the Mortality Information System; information on live births and the general population were obtained from the Information System on Live Births and Demographic Censuses, respectively. These data were available at the website of the informatics department of the Brazilian Unified Health System/Ministry of Health
ResultsMortality due to diarrheal disease in Brazil showed a downwards trend in both age groups. Regarding hospitalization, there was a slight downwards trend in children younger than 1 year and a non-significant upwards trend between 1-4 years, with a shorter hospital stay and lower mean value of hospital stay, regardless of age and region. The North and Northeast had the highest mortality rates and the highest percentage of hospitalizations in children younger than 1 year. The Midwest had the highest mean annual reduction in hospital stay.
ConclusionCurrently, the indicators of overall mortality and hospital morbidity due to diarrhea in Brazilian children are generally lower, but decreasing slowly.
Conhecer as tendências temporais dos indicadores de mortalidade geral e morbidade hospitalar por doença diarreica em crianças menores de um ano e de um a quatro anos, conforme as regiões brasileiras, entre 2000 e 2010.
MétodoEstudo ecológico de séries temporais. Os dados sobre Autorização de Internação Hospitalar, média de permanência e valor médio dessa autorização foram obtidos do Sistema de Informações Hospitalares; o número de óbitos infantis foi adquirido no Sistema de Informações sobre Mortalidade; as informações sobre os nascidos vivos e a população geral foram obtidas do Sistema de Informações sobre Nascidos Vivos e dos Censos Demográficos, respectivamente. Dados disponíveis no endereço eletrônico do Departamento de Informática do Sistema Único de Saúde/Ministério da Saúde.
ResultadosA mortalidade por diarreia no Brasil evidenciou tendência de decréscimo desacelerado em ambas as faixas etárias. Quanto à hospitalização, houve tendência decrescente discreta nos menores de um ano e ascendência insignificante entre 1-4 anos, entretanto, com menor permanência e valor médio de internamento, independentemente da idade e da região. Registraram-se no Norte e Nordeste os maiores coeficientes de mortalidade e maior porcentagem de internação nos menores de um ano. O Centro-Oeste apresentou maior redução média anual do tempo de permanência hospitalar.
ConclusãoAtualmente, os indicadores de mortalidade geral e morbidade hospitalar por diarreia em crianças brasileiras encontram-se, de forma geral, mais baixos, porém lentamente decrescentes.
Diarrheal disease (DD) is considered a public health problem with high morbidity and mortality worldwide.1 The demand for healthcare in the emergency department is high, often resulting in hospitalization and risk of death due to dehydration.
In 2008, infectious diseases were responsible for approximately six million deaths worldwide in children younger than 5 years. DD was responsible for 15% of these deaths (1.336 million), after pneumonia (18%, 1.575 million).2 In Brazil, between 1995 and 2005, there were 1,505,800 hospitalizations and 39,421 deaths of children younger than 1 year of age due to diarrhea and its complications.3
In some countries, oral rehydration therapy (ORT) was able yield a reduction of approximately 75% in infant deaths and of 61% in hospitalizations due to diarrhea between 1980 and 2008.4,5 However, there has been some stabilization in the rates of morbidity and mortality caused by this disease.6,7
The worldwide rates of morbidity and mortality from diarrhea, although lower, are not acceptable, considering that the disease can be prevented through relatively simple public health measures. Recent advances in the prevention and treatment of diarrheal disease, such as the formulation of improved oral rehydration solution, zinc supplementation, rotavirus vaccines, and vitamin A supplementation, are some of the measures proposed by the World Health Organization and the United Nations Children's Fund (WHO/UNICEF) to reduce these epidemiological indicators and revitalize DD control.1 However, evidence suggests a slow global progress since 2000 regarding the implementation of the new recommendations for the treatment and prevention of diarrhea.1
Given the above considerations and regional differences in Brazil, this study aimed to understand the temporal trends of indicators of overall mortality and hospital morbidity due to diarrheal disease in children younger than 1 year and between 1 and 4 years, according to the regions of Brazil, between 2000 and 2010.
MethodsThis was an ecological study of temporal series performed based on hospital morbidity data from the Brazilian Unified Health System (Sistema Único de Saúde - SUS), such as hospital admission authorization (HAA), mean length of hospital stay, and mean HAA value obtained from the Hospital Information System (Sistema de Informações Hospitalares – SIH/SUS); the number of infant deaths was obtained from the Mortality Information System (Sistema de Informações sobre Mortalidade – SIM); information on live births and the general population were obtained from the Live Birth Information System (Sistema de Informações sobre Nascidos Vivos – SINASC) and demographic censuses from the Brazilian Institute of Geography and Statistics (Instituto Brasileiro de Geografia e Estatística – IBGE), respectively. This evaluation included collection of pre-existing data, obtained from the SUS database, available on the website of the SUS Informatics Department (DATASUS) 8 The code used for data selection was A09 (diarrhea and gastroenteritis of presumed infectious origin), according to the tenth International Classification of Diseases (ICD-10).9
The coefficient of mortality, hospitalization rate, mean hospital stay, mean hospitalization values, and percentage of hospitalization of children younger than 1 year and between 1 and 4 years were described, as these age groups are the most vulnerable to this disease.
Calculation proceduresThe infant mortality rate for diarrhea was defined as the total number of deaths due to diarrhea in children younger than 1 year x 1,000 by the number of live births (LB). The mortality rate of children aged between 1 and 4 years due to diarrhea was defined as the total number of deaths due to diarrhea in children in this age group x 100,000 by the number of children aged between 1 and 4 years.
The rate of hospitalization due to diarrhea in children younger than 1 year was defined as the number of hospitalizations due to diarrhea in children younger than 1 year x 1,000 by the number of live births and the rate of hospitalization of children aged between 1 and 4 years as the number of hospitalizations due to diarrhea children at this age group x 100,000 by the number of children aged between 1 and 4 years.
The proportion of hospitalizations due to diarrhea in children younger than 1 year was defined as the number of hospitalizations due to diarrhea in children younger than 1 year x 100 by the total number of hospitalizations in children younger than 1 year and the proportion of hospitalization of children aged between 1 and 4 years was defined as the number of hospitalizations due to diarrhea in children in this age group x 100 by the total number of hospitalizations of children aged between 1 and 4 years. Hospital stay and mean hospitalization value due to diarrhea were obtained directly from DATASUS.
For the analysis of the temporal series, dynamic regression models were used (regression with ARIMA errors),10 as they allow for the incorporation and adjustment of the effect of a historical series autocorrelation, reducing such bias when estimating trends. For the total of the 50 series studied, those that were non-stationary were differentiated. Then, structural parameters of auto-regression and moving averages were estimated (autocorrelation (AR), differentiation (d), moving average (MA)), with an ARIMA notation (AR, d, MA), as well as the slopes of the regressions (β) representing the changes in average trends of the series, per year.
To diagnose the best model, the Akaike's information criterion10 that provided the least value was obtained for each series, together with the residual analysis, observation of autocorrelation and partial autocorrelation graphs (descriptively through the Ljung-Box test), evaluation of parameter overestimation, and comparison of the original data with those predicted by the models. As the entire target population was studied, inferential statistics were not calculated. The statistical package R, release 2.15.1, was used for the analysis of data in this temporal series.11
The Committee of Ethics in Research of the Complexo Hospitalar Universitário Professor Edgard Santos (COM-HUPES) approved this study under protocol No. 001/01/2012 as an addendum to a previously approved project by the same committee under protocol No. 121/2003.
ResultsAccording to official data from the Brazilian Ministry of Health, during the study period there were 22,933 deaths among children younger than 5 years due to ICD A09 (80.3% in children younger 1 year) and 1,209,622 hospitalizations (62.6% in children between 1 and 4 years); the Northeast accounted for 57% and 46%, respectively.
Coefficients of mortality due to diarrhea – ICD 409There was a reduction in the number of deaths in children younger than 1 year from approximately 77% in 2000 (2,738) to 2010 (632) versus 57% (541/235) among children aged 1 to 4 years. Between the extremes of the temporal series, reductions in the infant mortality rate from 0.96/1,000 to 0.39/1,000 in the North, from 1.62/1,000 to 0.38/1,000 in the Northeast, from 0.71/1,000 to 0.23/1,000 in the Midwest, from 0.43/1,000 to 0.1/1,000 in the Southeast, and from 0.5/1,000 to 0.08/1,000 in the South were observed. Regarding the coefficient of mortality of children aged between 1 to 4 years, there was a reduction from 6.81/100,000 to 5.04/100,000 in the North, from 6.05/100,000 to 2.52/100,000 in the Northeast, from 5.76/100,000 to 3.17/100,000 in the Midwest, from 1.99/100.000 to 1.13/100,000 in the Southeast, and from 2.86/100,000 to 0.85/100,000 in the South.
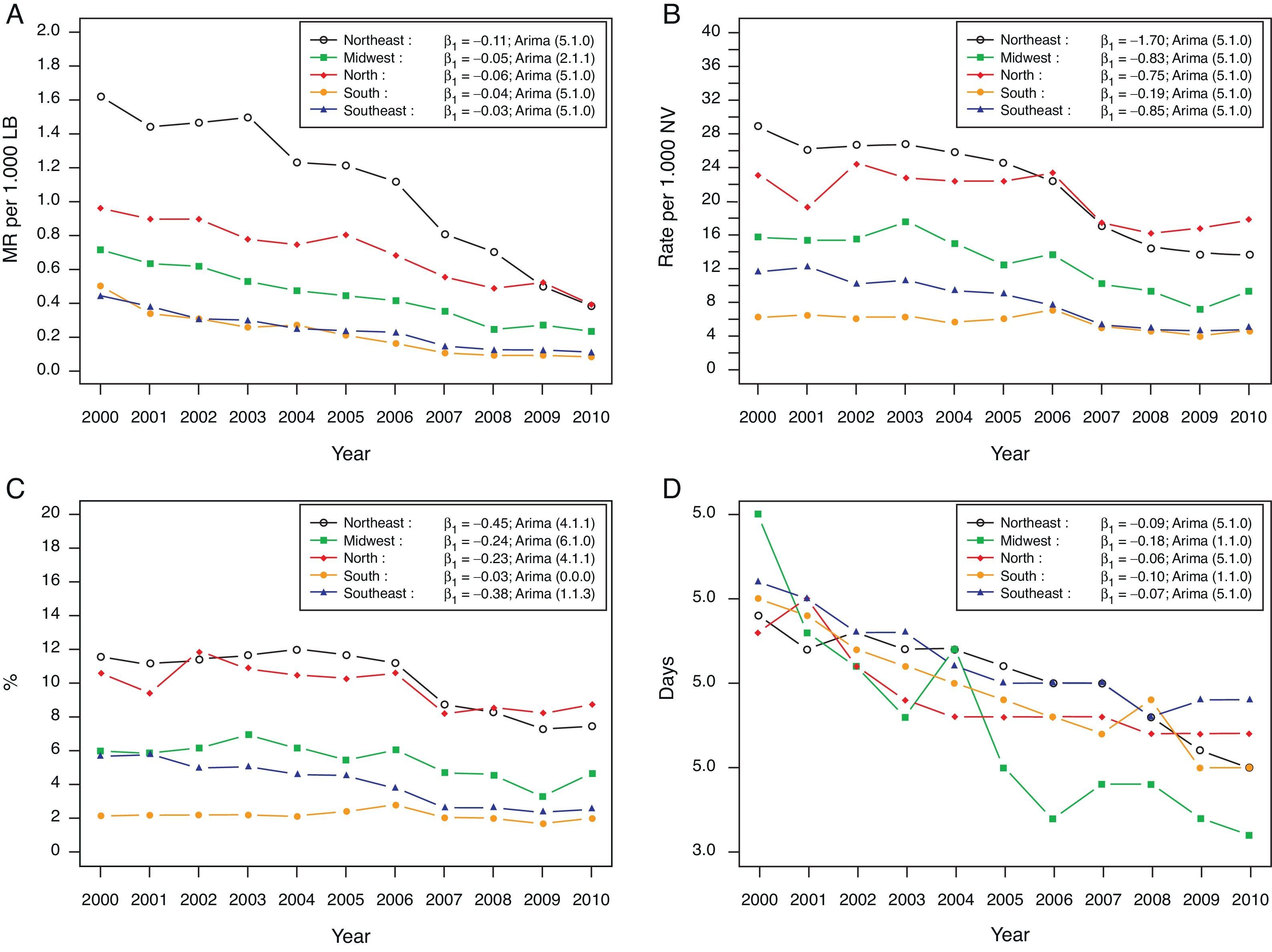
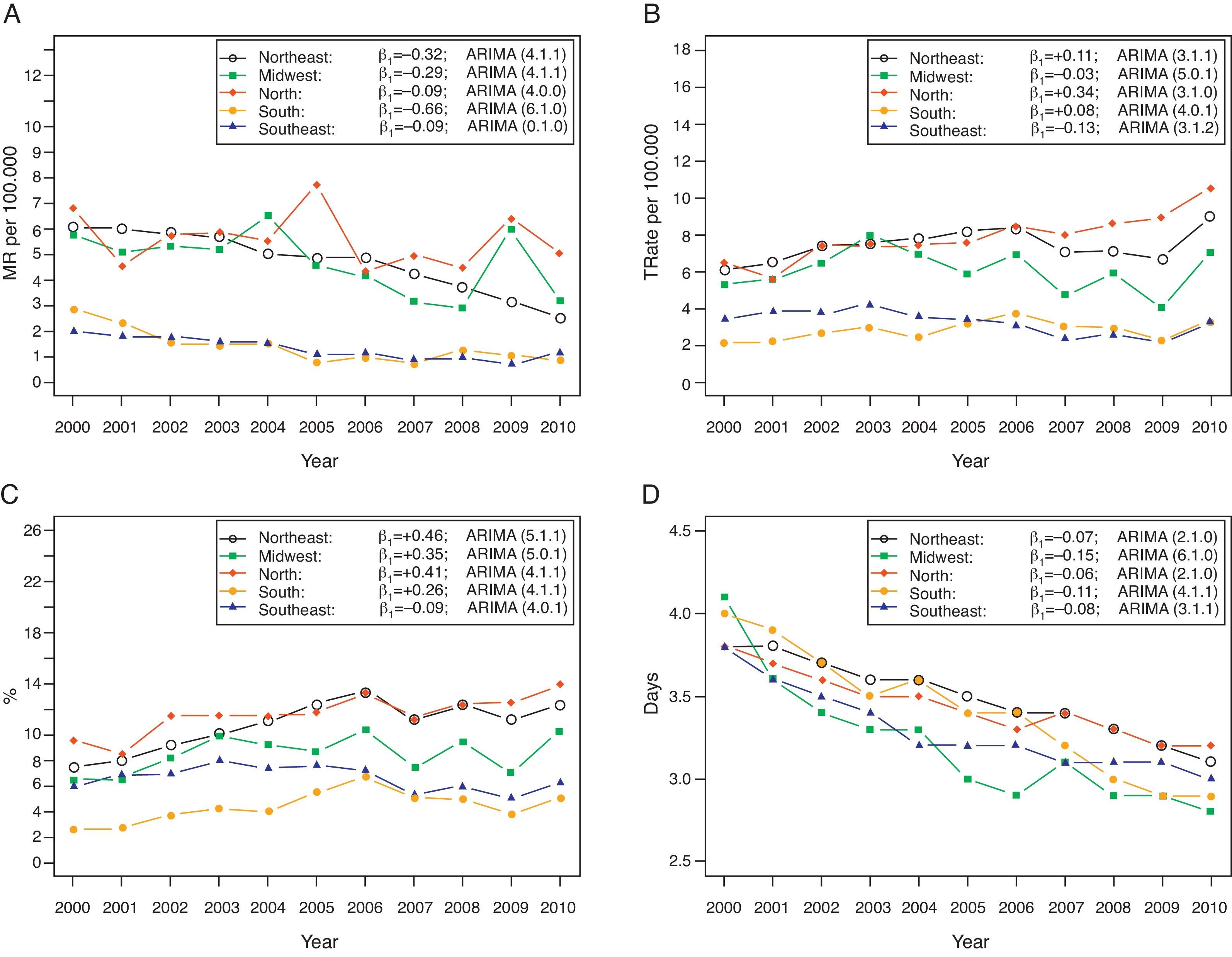
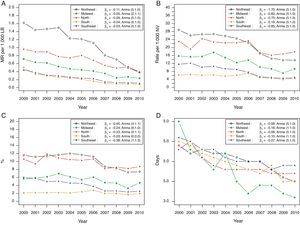
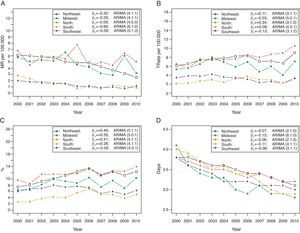
Figs. 1A and 2A show the downward trend in coefficients of mortality by age group and by region during the study period. For the age range younger than 1 year, all regions showed a slow decrease over time, ranging on average from 0.03 to 0.11 deaths/year/1,000 LB (3 to 11 deaths/year/100,000 LB). Although the Northeast (β1=-0.11) had the largest annual decrease, it was also the region, throughout almost the entire period, with the highest rates of infant mortality from diarrhea (ranging from 1.62 to 0.38 deaths/1,000 LB), followed by the North (β1=-0.06). Among older children, the mean annual reduction in the coefficient of mortality ranged from 0.09 to 0.66 deaths/100,000 (Tables 1 and 2). The North (5.6 deaths/100,000), Northeast (4.7 deaths/100,000), and Midwest (4.7 deaths/100,000) had, on average, higher values of mortality coefficients when compared to the South (1.4 deaths/100,000) and Southeast (1.3 deaths/100,000) during the ten-year study period.
(A) Child mortality coefficient per 1,000 LB due to diarrhea, according to the regions of Brazil, 2000-2010. (B) Child hospitalization rate per 1,000 LB due to diarrhea, according to the regions of Brazil, 2000-2010. (C) Percentage of children hospitalized due to diarrhea, according to the regions of Brazil, 2000-2010. (D) Mean hospital stay in days due to diarrhea, according to the regions of Brazil, 2000-2010. MR, mortality rate; LB, live births; β1, slope coefficient.
(A) Overall mortality rate per 100,000 children aged 1 to 4 years due to diarrhea, according to the regions of Brazil, 2000-2010. (B) Rate of hospitalization per 100,000 children aged 1 to 4 years due to diarrhea, according to the regions of Brazil, 2000-2010. (C) Percentage of hospitalization in children 1 to 4 years due to diarrhea, according to the regions of Brazil, 2000-2010. (D) Mean days of hospitalization in children aged 1 to 4 years due to diarrhea, according to the regions of Brazil, 2000-2010. MR, mortality rate; β1, slope coefficient.
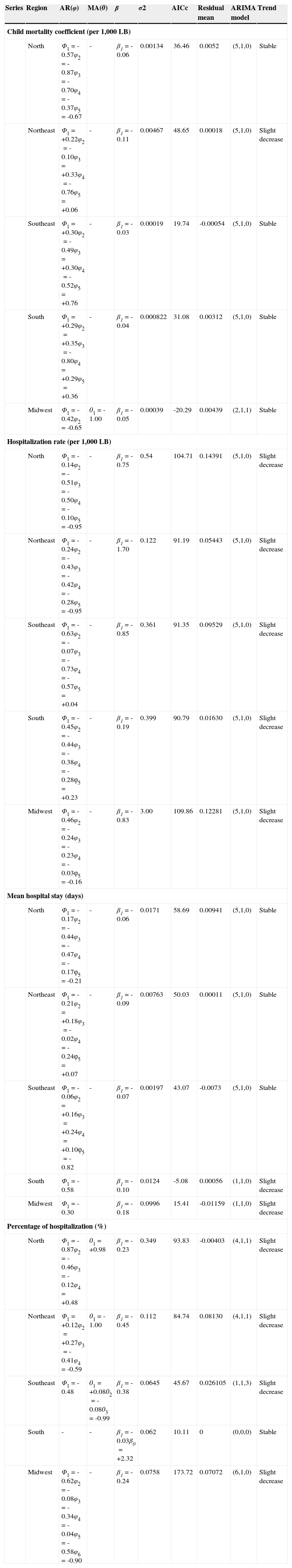
Estimated coefficients per year for temporal series of diarrhea in children younger than 1 year according to the region.
| Series | Region | AR(φ) | MA(0) | β | σ2 | AICc | Residual mean | ARIMA model | Trend |
|---|---|---|---|---|---|---|---|---|---|
| Child mortality coefficient (per 1,000 LB) | |||||||||
| North | Φ1=-0.57φ2=-0.87φ3=-0.70φ4=-0.37φ5=-0.67 | - | β1=-0.06 | 0.00134 | 36.46 | 0.0052 | (5,1,0) | Stable | |
| Northeast | Φ1=+0.22φ2=-0.10φ3=+0.33φ4=-0.76φ5=+0.06 | - | β1=-0.11 | 0.00467 | 48.65 | 0.00018 | (5,1,0) | Slight decrease | |
| Southeast | Φ1=+0.30φ2=-0.49φ3=+0.30φ4=-0.52φ5=+0.76 | - | β1=-0.03 | 0.00019 | 19.74 | -0.00054 | (5,1,0) | Stable | |
| South | Φ1=+0.29φ2=+0.35φ3=-0.80φ4=+0.29φ5=+0.36 | - | β1=-0.04 | 0.000822 | 31.08 | 0.00312 | (5,1,0) | Stable | |
| Midwest | Φ1=-0.42φ2=-0.65 | 01=-1.00 | β1=-0.05 | 0.00039 | -20.29 | 0.00439 | (2,1,1) | Stable | |
| Hospitalization rate (per 1,000 LB) | |||||||||
| North | Φ1=-0.14φ2=-0.51φ3=-0.50φ4=-0.10φ5=-0.95 | - | β1=-0.75 | 0.54 | 104.71 | 0.14391 | (5,1,0) | Slight decrease | |
| Northeast | Φ1=-0.24φ2=-0.43φ3=-0.42φ4=-0.28φ5=-0.95 | - | β1=-1.70 | 0.122 | 91.19 | 0.05443 | (5,1,0) | Slight decrease | |
| Southeast | Φ1=-0.63φ2=-0.07φ3=-0.73φ4=-0.57φ5=+0.04 | - | β1=-0.85 | 0.361 | 91.35 | 0.09529 | (5,1,0) | Slight decrease | |
| South | Φ1=-0.45φ2=-0.44φ3=-0.38φ4=-0.28φ5=+0.23 | - | β1=-0.19 | 0.399 | 90.79 | 0.01630 | (5,1,0) | Slight decrease | |
| Midwest | Φ1=-0.46φ2=-0.24φ3=-0.23φ4=-0.03φ5=-0.16 | - | β1=-0.83 | 3.00 | 109.86 | 0.12281 | (5,1,0) | Slight decrease | |
| Mean hospital stay (days) | |||||||||
| North | Φ1=-0.17φ2=-0.44φ3=-0.47φ4=-0.17φ5=-0.21 | - | β1=-0.06 | 0.0171 | 58.69 | 0.00941 | (5,1,0) | Stable | |
| Northeast | Φ1=-0.21φ2=+0.18φ3=-0.02φ4=-0.24φ5=+0.07 | - | β1=-0.09 | 0.00763 | 50.03 | 0.00011 | (5,1,0) | Stable | |
| Southeast | Φ1=-0.06φ2=+0.16φ3=+0.24φ4=+0.10φ5=-0.82 | - | β1=-0.07 | 0.00197 | 43.07 | -0.0073 | (5,1,0) | Stable | |
| South | Φ1=-0.58 | β1=-0.10 | 0.0124 | -5.08 | 0.00056 | (1,1,0) | Slight decrease | ||
| Midwest | Φ1=-0.30 | β1=-0.18 | 0.0996 | 15.41 | -0.01159 | (1,1,0) | Slight decrease | ||
| Percentage of hospitalization (%) | |||||||||
| North | Φ1=-0.87φ2=-0.46φ3=-0.12φ4=+0.48 | 01=+0.98 | β1=-0.23 | 0.349 | 93.83 | -0.00403 | (4,1,1) | Slight decrease | |
| Northeast | Φ1=+0.12φ2=+0.27φ3=-0.41φ4=-0.59 | 01=-1.00 | β1=-0.45 | 0.112 | 84.74 | 0.08130 | (4,1,1) | Slight decrease | |
| Southeast | Φ1=-0.48 | 01=+0.0802=-0.0803=-0.99 | β1=-0.38 | 0.0645 | 45.67 | 0.026105 | (1,1,3) | Slight decrease | |
| South | - | - | β1=-0.03β0=+2.32 | 0.062 | 10.11 | 0 | (0,0,0) | Stable | |
| Midwest | Φ1=-0.62φ2=-0.08φ3=-0.34φ4=-0.04φ5=-0.58φ6=-0.90 | - | β1=-0.24 | 0.0758 | 173.72 | 0.07072 | (6,1,0) | Slight decrease | |
AR(φ), Autoregressive term; ARIMA, autoregressive integrated moving average; cAIC, corrected Akaike information criterion; MA(0), moving average term; β, model coefficient; β0, intercept; β1, slope coefficient; σ2, variance average.
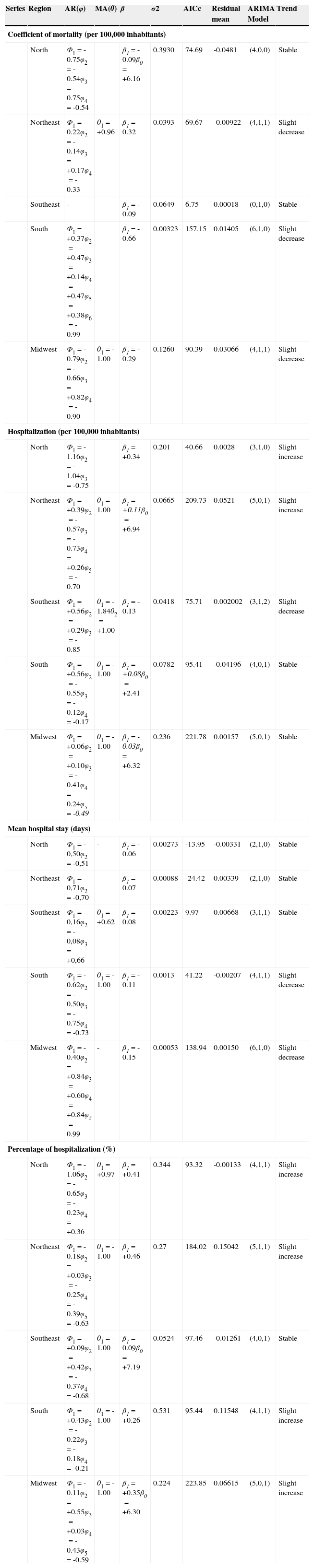
Estimated coefficients per year for temporal series of diarrhea in children aged 1 to 4 years depending on the region.
| Series | Region | AR(φ) | MA(0) | β | σ2 | AICc | Residual mean | ARIMA Model | Trend |
|---|---|---|---|---|---|---|---|---|---|
| Coefficient of mortality (per 100,000 inhabitants) | |||||||||
| North | Φ1=-0.75φ2=-0.54φ3=-0.75φ4=-0.54 | β1=-0.09β0=+6.16 | 0.3930 | 74.69 | -0.0481 | (4,0,0) | Stable | ||
| Northeast | Φ1=-0.22φ2=-0.14φ3=+0.17φ4=-0.33 | 01=+0.96 | β1=-0.32 | 0.0393 | 69.67 | -0.00922 | (4,1,1) | Slight decrease | |
| Southeast | - | β1=-0.09 | 0.0649 | 6.75 | 0.00018 | (0,1,0) | Stable | ||
| South | Φ1=+0.37φ2=+0.47φ3=+0.14φ4=+0.47φ5=+0.38φ6=-0.99 | β1=-0.66 | 0.00323 | 157.15 | 0.01405 | (6,1,0) | Slight decrease | ||
| Midwest | Φ1=-0.79φ2=-0.66φ3=+0.82φ4=-0.90 | 01=-1.00 | β1=-0.29 | 0.1260 | 90.39 | 0.03066 | (4,1,1) | Slight decrease | |
| Hospitalization (per 100,000 inhabitants) | |||||||||
| North | Φ1=-1.16φ2=-1.04φ3=-0.75 | β1=+0.34 | 0.201 | 40.66 | 0.0028 | (3,1,0) | Slight increase | ||
| Northeast | Φ1=+0.39φ2=-0.57φ3=-0.73φ4=+0.26φ5=-0.70 | 01=-1.00 | β1=+0.11β0=+6.94 | 0.0665 | 209.73 | 0.0521 | (5,0,1) | Slight increase | |
| Southeast | Φ1=+0.56φ2=+0.29φ3=-0.85 | 01=-1.8402=+1.00 | β1=-0.13 | 0.0418 | 75.71 | 0.002002 | (3,1,2) | Slight decrease | |
| South | Φ1=+0.56φ2=-0.55φ3=-0.12φ4=-0.17 | 01=-1.00 | β1=+0.08β0=+2.41 | 0.0782 | 95.41 | -0.04196 | (4,0,1) | Stable | |
| Midwest | Φ1=+0.06φ2=+0.10φ3=-0.41φ4=-0.24φ5=-0.49 | 01=-1.00 | β1=-0.03β0=+6.32 | 0.236 | 221.78 | 0.00157 | (5,0,1) | Stable | |
| Mean hospital stay (days) | |||||||||
| North | Φ1=-0,50φ2=-0,51 | - | β1=-0.06 | 0.00273 | -13.95 | -0.00331 | (2,1,0) | Stable | |
| Northeast | Φ1=-0,71φ2=-0,70 | - | β1=-0.07 | 0.00088 | -24.42 | 0.00339 | (2,1,0) | Stable | |
| Southeast | Φ1=-0,16φ2=-0,08φ3=+0,66 | 01=+0.62 | β1=-0.08 | 0.00223 | 9.97 | 0.00668 | (3,1,1) | Stable | |
| South | Φ1=-0.62φ2=-0.50φ3=-0.75φ4=-0.73 | 01=-1.00 | β1=-0.11 | 0.0013 | 41.22 | -0.00207 | (4,1,1) | Slight decrease | |
| Midwest | Φ1=-0.40φ2=+0.84φ3=+0.60φ4=+0.84φ5=-0.99 | - | β1=-0.15 | 0.00053 | 138.94 | 0.00150 | (6,1,0) | Slight decrease | |
| Percentage of hospitalization (%) | |||||||||
| North | Φ1=-1.06φ2=-0.65φ3=-0.23φ4=+0.36 | 01=+0.97 | β1=+0.41 | 0.344 | 93.32 | -0.00133 | (4,1,1) | Slight increase | |
| Northeast | Φ1=-0.18φ2=+0.03φ3=-0.25φ4=-0.39φ5=-0.63 | 01=-1.00 | β1=+0.46 | 0.27 | 184.02 | 0.15042 | (5,1,1) | Slight increase | |
| Southeast | Φ1=+0.09φ2=+0.42φ3=-0.37φ4=-0.68 | 01=-1.00 | β1=-0.09β0=+7.19 | 0.0524 | 97.46 | -0.01261 | (4,0,1) | Stable | |
| South | Φ1=+0.43φ2=-0.22φ3=-0.18φ4=-0.21 | 01=-1.00 | β1=+0.26 | 0.531 | 95.44 | 0.11548 | (4,1,1) | Slight increase | |
| Midwest | Φ1=-0.11φ2=+0.55φ3=+0.03φ4=-0.43φ5=-0.59 | 01=-1.00 | β1=+0.35β0=+6.30 | 0.224 | 223.85 | 0.06615 | (5,0,1) | Slight increase | |
AR(φ), Autoregressive term; ARIMA, autoregressive integrated moving average; cAIC, corrected Akaike information criterion; MA(0), moving average term; β, model coefficient; β0, intercept; β1, slope coefficient; σ2, variance.
In 2000, the absolute number of HAAs paid in Brazil with ICD A09, for children younger than 1 year was 55,161, with a reduction of 52% of this value in 2010 (26,347) and 14% increase (59,533 to 67,858) in children aged between 1 and 4 years. The rate of hospitalization for diarrhea in children younger than 1 year was nearly stable (slight mean annual decrease) in all regions throughout the series (Fig. 1B), with the highest reduction rate observed in the Northeast (β1=-1.70 – reduction of 1.7 hospitalizations per thousand LB each year) (Table 1).
Among older children, a stabilization trend was observed, with a non-significant increase (Fig. 2B), except in the Southeast, which presented a slight decrease in hospitalization rates (β1=-0.13) (Table 2). The same pattern was observed regarding the percentage of estimated annual hospitalizations in both age groups in the last decade (Tables 1 and 2); however, it could be observed that the North and Northeast had more hospitalized children due to diarrhea, especially among children younger than 1 year (Figs. 1C and 2C). On average, the rate of hospitalizations among children younger than 1 year in the Northeast was 10.2% (standard deviation [SD]=1.9%); in the North, 9.8% (SD=1.2%); in the Southeast, 4% (SD=1.3%); in the Midwest, 5.4% (SD=1.0%); and in the South, 2.2% (SD=0.3%). For older children, on average, the rate of hospitalization in the Northeast was 10.7% (SD=1.9%); in the North, 11.6% (SD=1.5%); in the Southeast, 6.5% (SD=1.0%); in the Midwest, 8.5% (SD=1.5%); and in the South, 5.3% (SD=1.2%).
The mean length of hospital stay during the study period was 4 days in those younger than 1 year and 3.4 days in children aged between 1 and 4 years, with a reduction of approximately 20% (0.85 days) between 2000 and 2010 in both age groups.
Figs. 1D and 2D demonstrates that the mean length of stay is decreasing and homogeneous in all regions, except for the Midwest, which presented a heterogeneous pattern, especially in children younger than 1 year; however, the Midwest presented the highest estimated annual decrease, although negligible, in the mean length of stay (days) in both age groups (β1=-0.18/β1=-0.15) (Tables 1 and 2).
The mean value paid by HAA in 2000/2010 was R$ 405.36 (US$ 221.14)/R$ 368.43 (US$ 209.72) and R$ 360.12 (US$ 196.46)/R$ 347.62 (US$ 197.88), for children younger than 1 year and between 1 and 4 years, respectively. This represents a reduction of 9.1% and 3.5%, respectively, for a mean stay of 4 days. The value of HAA in 2000 was adjusted for inflation, based on the year 2010.
DiscussionMortalitySince the 1980s, the overall infant mortality trend and that caused by diarrhea are described as downwards, both in Brazil3,12,13 and worldwide.2,6 However, it has been reported that progress in the decease of global mortality has not been accelerated, when compared with three decades ago;7 the same was observed in Brazil in the previous decade.13 In parallel, a slow progress has been observed in the implementation of the new global recommendations for diarrhea control.1 Contaminated water, inadequate sanitation, and poor hygiene still account for 88% of world deaths due to diarrhea.1
This slow progress in the management of diarrheal disease may be a factor contributing to the stabilization of infant mortality, since this disease is the second infectious cause of this indicator worldwide.1,2
It is fair to say that the current rates of mortality attributable to this disease in Brazil, albeit low, are still unacceptable. This is a disease transmitted via fecal-oral route; it is self-limited, preventable, of simple management at home with ORS, and does not require technology or relatively high costs for its prevention.
In some parts of Brazil, diarrhea is still a major public health problem.3 The regional heterogeneity in mortality rates from diarrhea described here reflects the socioeconomic and cultural inequality, as well as the difficulty of access to health care and sanitation.The Northeast and Midwest showed higher rates of reduction in these coefficients when compared to the South and Southeast. Although these regions showed higher levels of these indicators in 2000, which could explain the higher rates of reduction, it is possible that this downward trend is a reflection of national public health strategies, such as the Family Health program, training programs for professionals on diarrheal disease monitoring, rotavirus vaccine campaigns, breastfeeding encouragement programs, and vitamin A supplementation. These strategies were implemented in important sectors, especially after the 1990s, with promising results on the impact of overall mortality, as well as mortality due to diarrheal disease, in children younger than 5 years.3,14–17
It is possible that the recent investments aimed at reducing inequalities have been an important factor on infant mortality due to diarrhea in some regions;3 however, this assumption should be taken with caution due to the limitation of academic studies on infant mortality in regions such as the North and the Midwest.13
Such prevention strategies were considered models for export;16 however, regarding the treatment of diarrhea, Brazil does not explicitly adopt the recommendation of low-osmolarity ORS (66 countries) and zinc supplementation (46 countries). This occurs, perhaps, due to the difficulty to acquire and/or handle the products, mainly by the financial investment involved in this process.1 According to the National Survey on Demography and Health/2006, Brazil used the “homemade hydration solution” more frequently than other forms of ORS (government-provided solution and commercially available solutions) to revert cases of morbid diarrhea.18
Hospital morbidityLower numbers of deaths from diarrhea have been recorded, but without a proportional decrease in morbidity attributable to this disease,6,18 which imposes a heavy burden on the public health system.19 The present study showed a slow annual reduction in rates of hospitalization for diarrhea in children younger than 1 year and a slight increase in children between 1 and 4 years, demonstrating that hospitalizations remained generally stable, despite a modest increase in some regions of the country (North/Northeast).
National literature mentions a reduction of approximately 40% to 60% in the rate of hospitalization in children younger than 1 year,3,20 with different evolutions between the Brazilian regions and stabilization between the ages of 1 and 4 years,20 but at different time periods. In the U.S., diarrhea was considered a major cause of hospitalization of children younger than 5 years in 2000, with an expected reduction after rotavirus vaccination measures.21 This fact was recorded in Brazil,15 mainly in children younger than 1 year, although in the present study a small reduction in hospitalization rates was observed, perhaps explained by the low and variable rotavirus vaccine coverage achieved since 2006 in Brazil.8 Even though the Brazilian Ministry of Health established a goal of coverage of 90%,22 the maximum coverage achieved was 84.4% in 2009, and the mean was only 58.7% in the country between 2006 and 2010.
In spite of the mentioned reduction, gastroenteritis and its complications are the leading cause of hospitalization of children younger than 5 years due to conditions treated in primary care between 1999 and 2006, with higher rates of hospitalization in the North, Northeast, and Midwest.20 The trend in this series was similar: the North and Northeast accounted for the greatest number of hospitalizations, especially in children younger than 1 year, throughout the study period. This is possibly due to socioeconomic and cultural differences historically found in these regions, in addition to the increased demand for public hospitals in these regions.18
The recommendation of hospitalization during an episode of diarrhea is restricted to complicated cases with severe dehydration due to hypovolemic shock and high risk of death, in addition to small infants, malnourished patients, those with elevated fecal loss, and those whose caregiver is unable to successfully manage the disease at home.23 Furthermore, the low level of education in certain regions of Brazil account for most of the hospitalizations.18Despite the success of preventive strategies to control diarrheal disease in Brazil, the deficit of primary care in some regions affects the redirection of care in cases of diarrhea to emergencies,19,24 with presumed risk of hospitalization secondary to multifactorial causes, favoring the mismanagement of the case (intravenous rehydration, unnecessary use of drugs, excessive tests), increasing the time and cost of hospitalization.4,19,25–27
In this study, the mean hospital length of stay during ten years was reduced by only 20% (0.85 days), with a mean of 4 days among children younger than 1 year and 3.4 days in those aged 1 to 4 years. The Midwest and South had the highest rates of annual decrease, a fact that needs further investigation to better understand such behavior.
Associated with a modest reduction in hospital length of stay, there was a small reduction in mean hospitalization value (adjusted for inflation during the period), and it was assumed that investments targeted to reduce the length of hospitalization may represent a reduction in the health system burden attributed to diarrheal disease.
In Brazil, in 2010, approximately R$ 9.8 million were spent on hospital admissions of children younger than 1 year with diarrhea, and R$ 23.5 million for those aged between 1 and 4 years;8 these resources could have been invested in new therapeutic recommendations for the management of this pathology. It is worth mentioning that the HAA system of hospitalization control is based on a table of costs per procedure, not necessarily associated with the actual costs of the hospitalization;28 therefore, these values may be underestimated.
Research priorities are being defined to reduce the overall morbimortality of childhood diarrhea by 2015; the main areas are targeted for public health and epidemiological policies in order to understand the barriers to the implementation and to optimize the available programs and interventions.29
It appears that strategies aimed at reducing the number of hospitalizations and length of hospital stay, with consequent reduction in cost and risk to the patient, are appropriate in the management of diarrheal disease in Brazil.
ConclusionThe levels of mortality rates in children from diarrhea were found to be lower and slowly decreasing over the study period. Hospitalization rates remained stable, and there was a slight decrease in hospital length of stay and hospital costs during disease management. There were regional differences for all indicators, except for the mean hospital stay.
Clear and socially regulated public policies aiming primarily at reducing social differences; enabling collective sanitary measures; structuring health services; training human resources; and encouraging and financing research in local health diagnosis, information solutions, prevention, and treatment must be strategically coordinated so they can effectively extend the scope and resolution of what has been achieved when addressing this specific but crucial health situation.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Mendes PS, Ribeiro Jr. HC, Mendes CM. Temporal trends of overall mortality and hospital morbidity due to diarrheal disease in Brazilian children younger than 5 years from 2000 to 2010. J Pediatr (Rio J). 2013;89:315–25.