To describe the nutritional assessment of children with cerebral palsy, verifying the correlation of growth curves specific for cerebral palsy with general curves, in addition to assessing the presence of digestive manifestations associated with nutritional problems.
MethodsThis was a cross-sectional study of 187 individuals with cerebral palsy, evaluating anthropometric data in curves commonly used in pediatrics and specific curves for cerebral palsy, in addition to the description of presence of dysphagia, constipation, and respiratory infections.
Results58% of patients were males, with a mean age of 5.6±3.5 years. Anthropometric data of weight below the 10th percentile occurred in 10% of the sample considering the cerebral palsy scale, versus 51% when considering the reference from the Centers for Disease Control and Prevention (p < 0.01; Kappa 0.19). The weight of most individuals with dysphagia, recurrent respiratory infections, and constipation was below the 50th percentile, with respective percentages of 67%, 75%, and 72%.
ConclusionThe references commonly used in pediatrics tend to overestimate malnutrition in individuals with cerebral palsy, and their correlation with specific references for cerebral palsy is low. Digestive manifestations were mainly found in those individuals whose anthropometric measurements were below the 50th percentile.
Descrever a avaliação nutricional de crianças com paralisia cerebral, verificando a concordância de curvas de crescimento específicas para paralisia cerebral com curvas gerais, além de avaliar a presença das manifestações digestórias associadas a agravos nutricionais.
MétodosCorte transversal de 187 indivíduos com paralisia cerebral, avaliando-se dados antopométricos em curvas habitualmente utilizadas em pediatria e em curvas específicas para paralisia cerebral, além da descrição da presença de disfagia, constipação intestinal e infecções respiratórias de repetição.
ResultadosDos indivíduos, 58% eram masculinos; média de idade de 5,6 anos+3,5 anos. Dados antopométricos de peso abaixo do percentil 10 ocorreu em 10% da amostra, considerando a escala para paralisia cerebral, contra 51% na referência do Center of Disease Control (p < 0,01; Kappa 0,19). A maioria dos indivíduos comprometidos com disfagia, infecções respiratórias de repetição e constipação intestinal encontrava-se abaixo do percentil 50, com porcentagens respectivas de 67%, 75% e 72%.
ConclusãoAs referências habitualmente utilizadas em pediatria tendem a superestimar a desnutrição em indivíduos com paralisia cerebral, e sua concordância com referências específicas para paralisia cerebral é baixa. As manifestações digestórias foram encontradas principalmente naqueles indivíduos cujas medidas antropométricas encontram-se abaixo do percentil 50.
Disorders of growth and nutrition are common health problems in children with cerebral palsy (CP).1 Alterations in overall growth, such as obesity and malnutrition, still represent challenges when caring for children with CP, both for pediatricians and specialized teams. These nutritional deficiencies can add losses to motor and cognitive development, socialization, psychological function, use of health services and need for hospitalizations, and overall health in individuals who already have problems in all these areas.2
The investigation of these growth disorders depends on advances in the available nutritional assessment methods to meet the challenges inherent in anthropometry in children with CP.3 In general, health teams use reference measures for populations with no neurological deficits, which are not suitable for children with CP.
Studies to define methods and specific references more appropriate to assess growth in individuals with CP have been performed in recent years, and the improvement in the knowledge and practice of nutrition rehabilitation measures have led to increased survival in CP.4 Specific and descriptive growth charts and other ways of measuring body composition provide information that can help teams through early identification of nutritional and metabolic problems of growth so that effective intervention can be provided.5,6 However, most of these studies were conducted in developed countries; studies evaluating nutritional status in CP in developing countries are scarce, especially in Brazil.
Thus, adequate anthropometry is very important to provide adequate and individualized nutritional counseling, as well as to provide better quality of life for children and adolescents with CP and their families.
Based on these aspects, this study was designed to describe the nutritional assessment of children with CP, verifying the agreement of specific growth curves for CP with general curves, as well as assessing the presence of digestive manifestations associated with nutritional problems.
MethodsThis was a cross-sectional, descriptive, and retrospective study, with anthropometric data measured on admission of patients with CP treated at a rehabilitation hospital between March of 2001 to March of 2007.
The sampling plan was a simple random sample, without replacement, among children with CP admitted during the study period. Considering that there are qualitative and quantitative variables, the authors chose to establish the sample background according to a quantitative variable. Based on this requirement, the absolute variance of the ratio at a maximum value of 0.25, resulting from p (1-p) for p=0.50, with a confidence level of 95% and approximate error of inference for proportions not exceeding 6.5% were established. Finally, the sample size was adjusted due to the fact that the population is finite, reaching a number of 200 individuals. The charts were arranged in an electronic spreadsheet and each was assigned a unique number. Through a table of random numbers generated by Excel® software, successive draws were performed, with no replacement, from the numbers assigned to the medical records to complete the calculated sample size.
The study included children between 2 and 16 years, diagnosed with CP, of both genders, from the state of Bahia. Exclusion criteria were lack of data on weight in the medical record or other diagnoses associated with genetic syndromes and myelomeningocele. After evaluation, 13 subjects did not meet all the criteria, and the sample consisted of 187 subjects.
Data were collected from medical records, using a protocol that included variables such as gender; age; description of the CP classification; percentiles of weight, height, and body mass index (BMI); and diagnosis of digestive alterations, such as dysphagia and constipation, as well as recurrent respiratory infections (RRI).
Weight was measured on a digital scale calibrated to zero, in kilograms, with the child unclothed, or by calculating the difference between the caregiver's weight with and without the child. Height was measured in centimeters using a stadiometer, with the child in the supine or standing position, in those individuals who had no major skeletal deformities (such as scoliosis, kyphosis, or structured deformities in lower-limb flexion). For those with deformities, height was estimated using the knee height equation, where: Height=(2.69 x knee height)+24.2.7 The formula that uses the measurement of the knee to the heel is the most recommended, as this measurement shows the smallest error relative to the measured height.8
BMI was obtained through weight over the square of height in meters (kg/m2). The anthropometric profile was obtained by entering the anthropometric data in the growth curves for children with CP proposed by Brooks et al.,5 and also in the growth curves recommended by the Centers for Disease Control and Prevention (CDC).9
The same parameters were used in both growth curves: weight/age, height/age, and BMI. “Nutritional deficit” (malnourished) was considered in those whose data were below the 10th percentile; normal weight was considered in those between the 10th and 50th percentile; at risk of overweight between the 50th and the 90th percentile; and overweight in those > the 90th percentile.
CP classification was based on motor impairment predominance: spastic, dyskinetic or extrapyramidal, cerebellar or ataxic, hypotonic, and mixed. Another classification used was the Gross Motor Function Classification System (GMFCS), containing five subgroups according to the severity of motor impairment, progressively varying from the milder level I to the most severe level V. In the present study, subjects were allocated at different levels based on motor acquisition as described by Brooks et al.:5
- I.
Walks without limitations
- II.
Walks with limitations
- III.
Walks using a hand-held mobility device
- IV.
Self-mobility with limitations; may use powered mobility
- V.
Transported in a manual wheelchair
Dysphagia was clinically evaluated using data from specific protocols collected during the interview and observation of intake of different food textures. The clinical data analyzed for the presence of dysphagia were: alteration in cervical auscultation and pulse oximetry, coughing or choking during or after swallowing, deficient oral motor skills, delayed pharyngeal response (to elicit the deglutition reflex), multiple deglutition, increased secretion or stridor in the upper airways during or after deglutition, and modified breathing rhythm.8
RRI was defined by the occurrence of three episodes of otitis media within a period of six months or four episodes in 12 months; recurrent infectious rhinitis, usually defined as more than five episodes per year; recurrent tonsillitis or pharyngitis, with more than three episodes in 12 months; frequent coughing, with fever and upper airway hypersecretion; daily or almost daily coughing for more than three months; more than one case of pneumonia in the last two years; or persistent bronchospasm.10,11
The study was approved by the Ethics and Research Committee of the SARAH Network of Rehabilitation Hospitals.
The data were stored in an ACCESS® database and the statistical analysis was subsequently performed using the Statistical Package for Social Sciences (SPSS®), release 17.0. EXCEL® was used in the selection of the sample elements. Descriptive analyses were used predominantly with measurements of frequency, central trend, and dispersion, in addition to graphical representations. The chi-squared test and the Kruskal-Wallis H test were used for comparisons of categorical variables. The Kolmogorov-Smirnov test was used to evaluate the distribution of variables in relation to normal. The reliability of agreement between the different methods used (World Health Organization [WHO]/CDC curves versus CP curves) was assessed by the weighted kappa coefficient, using the absolute error and their respective 95% confidence intervals as the weighting system and significance tests. The level of significance was set at 5%.
ResultsThe sample consisted of 187 individuals. Regarding gender distribution, 58% were males, and the mean age at admission was 5.6 years±3.5 years.
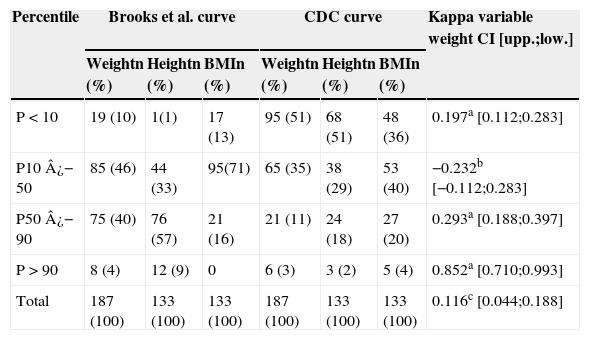
The observed weight was below the 50th percentile in most individuals with CP, both in the CP curve (56%), and in the CDC curve (86%), with statistically significant difference. Data distribution of weight, height, and BMI are shown in Tables 1 and 2, according to the reference curves specific for CP and those commonly used in pediatrics, with a Kappa index obtained by comparing the weight of the two references used. Considering the CP scale by Brooks et al., “malnutrition” (P<10) occurred in 10% of the sample. In the CDC reference, 51% of subjects were classified as below P10. The findings suggestive of overweight were similar in both evaluations, with a Kappa index of 0.0852 (Table 1).
Anthropometric data in percentiles according to the references by Brooks et al. for individuals with cerebral palsy (CP) and the Centers for Disease Control and Prevention (CDC) reference commonly used in pediatrics.
| Percentile | Brooks et al. curve | CDC curve | Kappa variable weight CI [upp.;low.] | ||||
|---|---|---|---|---|---|---|---|
| Weightn (%) | Heightn (%) | BMIn (%) | Weightn (%) | Heightn (%) | BMIn (%) | ||
| P < 10 | 19 (10) | 1(1) | 17 (13) | 95 (51) | 68 (51) | 48 (36) | 0.197a [0.112;0.283] |
| P10 ¿− 50 | 85 (46) | 44 (33) | 95(71) | 65 (35) | 38 (29) | 53 (40) | −0.232b [−0.112;0.283] |
| P50 ¿− 90 | 75 (40) | 76 (57) | 21 (16) | 21 (11) | 24 (18) | 27 (20) | 0.293a [0.188;0.397] |
| P > 90 | 8 (4) | 12 (9) | 0 | 6 (3) | 3 (2) | 5 (4) | 0.852a [0.710;0.993] |
| Total | 187 (100) | 133 (100) | 133 (100) | 187 (100) | 133 (100) | 133 (100) | 0.116c [0.044;0.188] |
BMI, body mass index; CI, confidence interval; CP, cerebral palsy; low, lower limit; upp, upper limit.
Statistical significance of the weighted kappa values shown as: a p-value <0.001, b not interpretable and does not apply to test, and c p-value <0.002.
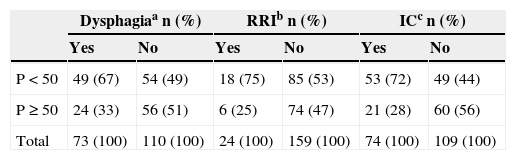
Digestive alterations and RRI distributed in different weight percentiles in 183 subjects with CP.
| Dysphagiaa n (%) | RRIb n (%) | ICc n (%) | ||||
|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | |
| P < 50 | 49 (67) | 54 (49) | 18 (75) | 85 (53) | 53 (72) | 49 (44) |
| P ≥ 50 | 24 (33) | 56 (51) | 6 (25) | 74 (47) | 21 (28) | 60 (56) |
| Total | 73 (100) | 110 (100) | 24 (100) | 159 (100) | 74 (100) | 109 (100) |
IC, intestinal constipation; RRI, recurrent respiratory infection.
Chi-squared test: a p-value=0.016; b p-value=0.047; c p-value <0.001.
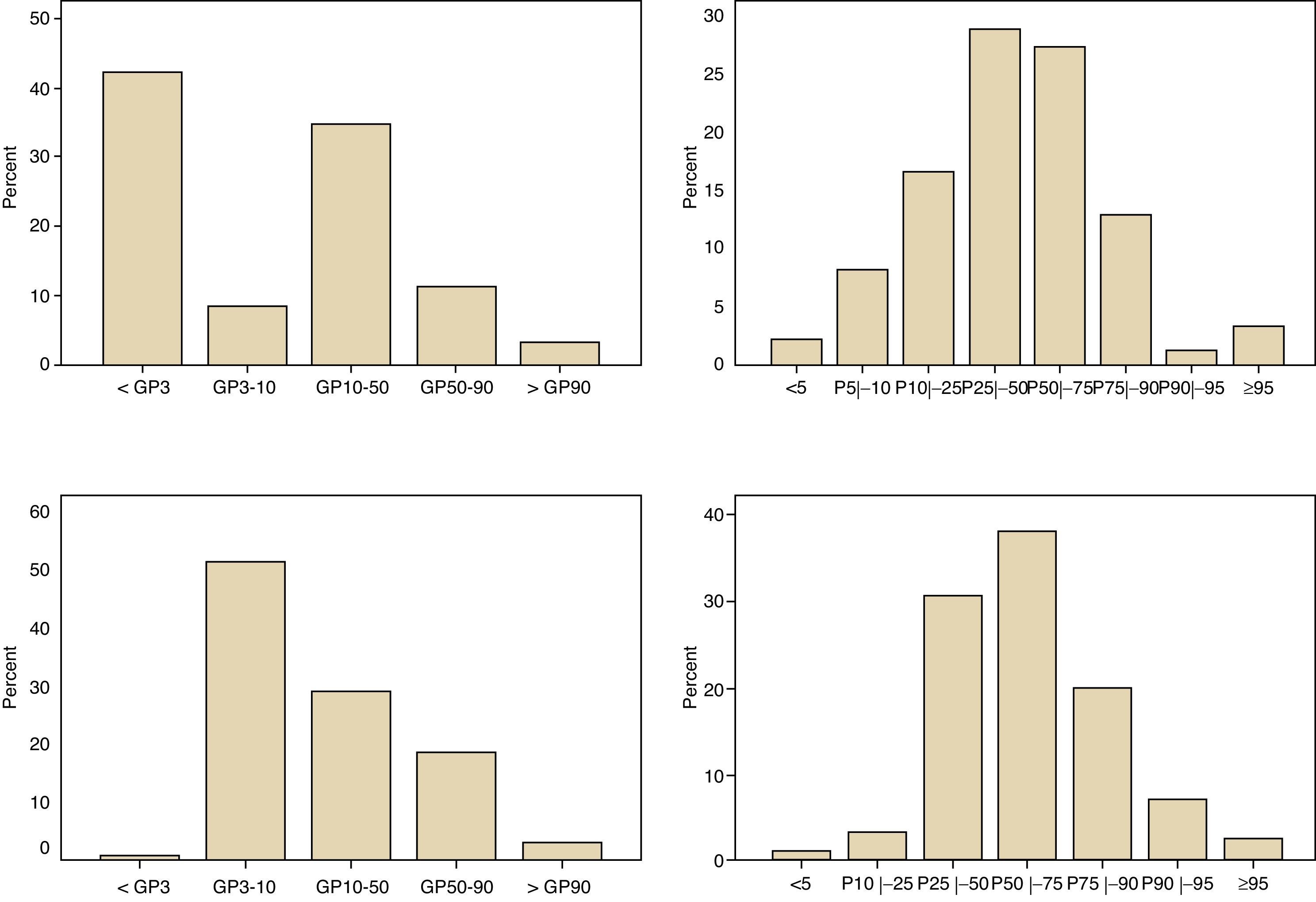
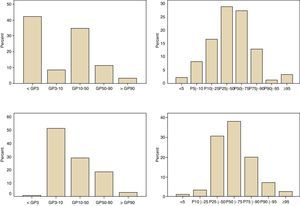
Moreover, regarding the agreement between the two references used, the Kolmogorov-Smirnov normality test showed that the distribution was non-normal for both references. The respective histograms are shown in Fig. 1. The assessment of the agreement between the two references using the Wilcoxon test was statistically significant.
Histograms of weight (a) and height (b) percentiles in 187 individuals with cerebral palsy (CP) in this study; to the left, according to the nutritional classification of the Centers for Disease Control and Prevention (CDC) and to the right, according to the specific nutritional classification for individuals with CP of Brooks et al.5.
Data on dysphagia, RRI, and intestinal constipation (IC) were present in 183 subjects. For all these variables, it was observed that most individuals affected with dysphagia, RRI, and IC were below the 50th percentile, with respective percentages of 67%, 75%, and 72% (Table 2). In the studied sample, 4 subjects were fed via gastrostomy, and 183 orally.
Of the total, 144 children were classified as spastic CP, 34 as dyskinetic, 3 as ataxic, one as hypotonic, and 6 as mixed. In the analysis of frequency of weight percentiles in relation to the different topographies of spastic classification of CP, it was observed that 13% of individuals with tetraplegia were below the 10th percentile, and 49% were between 10th and 50th percentiles, with p = 0.157 (Kruskal-Wallis).
DiscussionThis study showed that the references commonly used in pediatrics tend to overestimate malnutrition in individuals with CP. Another important point was that the results corroborate those in the literature regarding the low correlation between the distribution of anthropometric data in specific percentiles for PC and for general references of nutrition assessment. Data obtained through the Kappa index showed poor agreement in the anthropometric assessment of the group below the 10th percentile and between the 50th and 90th percentiles. Although a negative Kappa index was found in the group between the 10th and 50th percentiles, any Kappa value < 0 indicates that the agreement found was less than that expected by chance, therefore suggesting disagreement.
In the group of overweight individuals, the Kappa index showed agreement, but the result may have been influenced by the low frequency of subjects with anthropometric data in that range. These differences should alert interdisciplinary teams accompanying the children with CP to the importance of using appropriate tools in order to obtain a more reliable anthropometric profile and more realistic nutritional goals in nutritional rehabilitation.
As the individual with CP has a peculiar growth pattern, studies aiming to find more appropriate forms of nutritional assessment are of great value, especially in developing countries such as Brazil.12 The pediatrician, who must systematically perform the nutritional assessment in all consultations, may have difficulties in evaluating individuals with CP.
Nutritional alterations are frequently observed in children with CP and are of multifactorial etiology, secondary to factors related to the neurological damage, decreased nutritional intake, and adequate nutritional support, as well as morphological and functional digestive alterations, mainly those related to motility disorders, osteoarticular alterations, particularities of growth, and hormonal alterations.13,14
In the present study, digestive manifestations were found more frequently in subjects with anthropometric data below the 50th percentile, and it was observed that 50% of individuals were below the 10th percentile, considering the general references of CDC. These data are in agreement with the literature, which describes malnutrition in 40% to 90% of individuals with the same type of analysis.4,15–17 It is noteworthy that the use of the CDC reference as the usual reference for healthy children was also used by Brooks et al. in their study.5 Moreover, although the WHO has constructed new anthropometric charts for healthy children in 2006, their usefulness in relation to the CDC curves is still questionable.18
The specific curves for CP classified fewer individuals with nutritional deficit than those from the CDC, for weight, height, and BMI. These findings corroborate data from recent studies that have shown that body composition of children with CP is different from that of healthy children for weight, height, and BMI, and that current methods of body assessment tend to underestimate the nutritional diagnosis.7,19,20
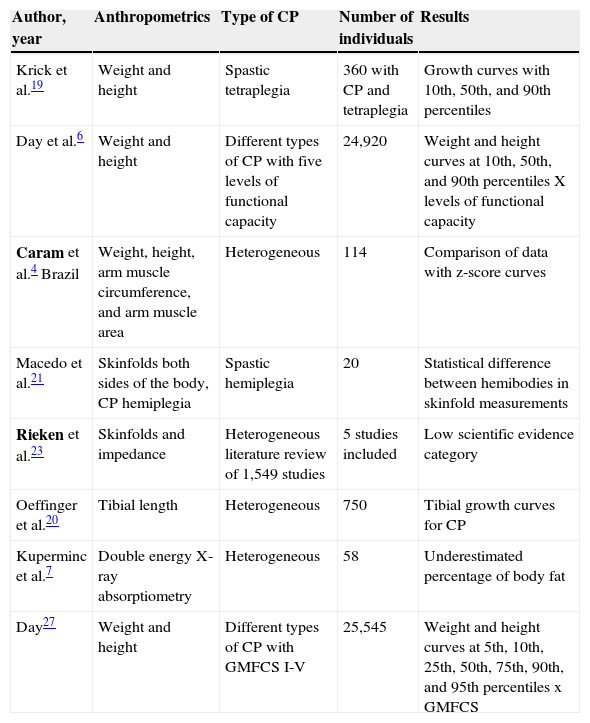
Recent studies have been performed in order to develop a more appropriate nutritional assessment for individuals with CP, such as by measuring height and weight through arm circumference and skinfold thickness, measurement of body segments and other more sophisticated techniques, such as impedance and X-ray emission/absorption (Table 3).4–6,19–23 In 1996, Krick et al. evaluated anthropometric data of 360 children with spastic quadriplegic CP between 2 and 12 years and developed specific growth curves for this profile, which they compared with reference curves from the CDC.19 The researchers found that children with quadriplegic CP had weight and height below normal when compared with healthy children. Most individuals with anthropometric data at the 50th percentile for height/age and weight/age of the reference curves for CP were classified as “below the 10th percentile” using the CDC reference. The results were similar for the height/weight parameter.19
Nutritional assessment studies with different methodologies.
| Author, year | Anthropometrics | Type of CP | Number of individuals | Results |
|---|---|---|---|---|
| Krick et al.19 | Weight and height | Spastic tetraplegia | 360 with CP and tetraplegia | Growth curves with 10th, 50th, and 90th percentiles |
| Day et al.6 | Weight and height | Different types of CP with five levels of functional capacity | 24,920 | Weight and height curves at 10th, 50th, and 90th percentiles X levels of functional capacity |
| Caram et al.4 Brazil | Weight, height, arm muscle circumference, and arm muscle area | Heterogeneous | 114 | Comparison of data with z-score curves |
| Macedo et al.21 | Skinfolds both sides of the body, CP hemiplegia | Spastic hemiplegia | 20 | Statistical difference between hemibodies in skinfold measurements |
| Rieken et al.23 | Skinfolds and impedance | Heterogeneous literature review of 1,549 studies | 5 studies included | Low scientific evidence category |
| Oeffinger et al.20 | Tibial length | Heterogeneous | 750 | Tibial growth curves for CP |
| Kuperminc et al.7 | Double energy X-ray absorptiometry | Heterogeneous | 58 | Underestimated percentage of body fat |
| Day27 | Weight and height | Different types of CP with GMFCS I-V | 25,545 | Weight and height curves at 5th, 10th, 25th, 50th, 75th, 90th, and 95th percentiles x GMFCS |
CP, cerebral palsy; GMFCS, Gross Motor Function Classification System.
In 2007, Day and colleagues conducted a study of anthropometric data on weight, height, and BMI of 24,920 individuals with CP between the ages of 2 to 20 years.6 They developed new growth curves specific for children with CP, also using individuals from the United States. These curves comprehended different types of CP with four levels of motor acquisition, and a specific curve for gastrostomized individuals. The results also showed that individuals with CP had different weight and height than normal subjects, except for the group with better motor performance (patients with independent gait), where growth was similar to that of healthy children at a young age.6
In 2011, Brooks et al. performed a new study to determine the nutritional status of 25,545 individuals according to the GMFCS classification of motor performance, when new curves were designed. These curves were used in the present study as a benchmark for CP, as they were the result of a recent study involving a more representative sample, due to both its size and the heterogeneity of the CP. Once again, it was reported that the worse the motor impairment, the higher the difference between curves; the results of the present study corroborate this assertion.5
Similar to other studies, the largest anthropometric discrepancies were found in the most compromised groups. In these, malnutrition is more typical due to the severe difficulties caused by the neurological impairment associated with poor nutritional intake, higher frequency of digestive alterations, increased losses and higher energy expenditure, in addition to the lack of training and the difficulties faced by caregivers when feeding these children.24
In subjects with more severe neurological impairment, brain injuries are more extensive, interfering with the neural control of deglutition, esophageal transit, gastrointestinal transit, and defecation. Neurogenic dysphagia, gastroesophageal reflux disease, constipation, and RRI are secondary to neural control alterations of the digestive tract, added to the peculiarities involved in the care of children with CP, such as other associated alterations, type of food, caregiver experience, among others.2,25,26 Digestive alterations determine higher nutritional impairment and anthropometric deficits in curves, creating greater risk of hospitalizations, school absences, impaired neuropsychomotor development,and mortality.27
It is noteworthy that malnutrition during childhood can impair brain development, cell division of neurons, myelination, and synaptogenesis.28 The impact of these factors on an already compromised brain may be even higher, exacerbating the developmental delay and possibilities of neuroplasticity, as well as cognitive and motor skills.
There are several obstacles that limit satisfactory food intake in children with CP.13 Among them can be mentioned neurological immaturity, the interference of mood and training of caregivers, as well as the characteristics of individuals with CP (difficulties of positioning; movement disorder and deformities; epilepsy; dental abnormalities; cognitive and language delay, which hinders communication regarding hunger and food preferences; and pasty foods, making the meal monotonous and risking loss of nutrients in preparation, among others).13,29 All these factors are interconnected in a vicious circle of neurological impairment, digestive manifestations, malnutrition, and global health threat.
The retrospective study has some limitations, which do not invalidate the results. Height was measured using the same tools, by the team that receives the same training for the care of individuals with CP, which reduces the risk of interobserver discrepancies. Weight assessment was performed on the same calibrated scale, which is independent from the observer. Therefore, the main results were based on the analysis of weight.
The interdisciplinary team must be involved and train caregivers in feeding the children, regarding proper food consistency and posture during meals, and content and balance of nutrients. They must also help identify individuals who require pharmacological treatment for gastroesophageal reflux disease and constipation, and those who have indication for gastrostomy with concomitant antireflux surgery, in order to improve the nutritional status, overall health, and quality of life of individuals with CP and their families.
Based on the results of this study, it can be observed that anthropometry and growth of children with CP differ from that of healthy children. Thus is emphasized the importance of the use of nutritional assessment methods by the professional team treating with children with CP, both general pediatricians and members of specialized teams, in order to properly predict the nutritional status in this specific population. Consequently, more realistic goals in nutritional rehabilitation can be achieved.
More studies are needed to assess the nutritional status in this population in other areas of Brazil, in order to compare them among themselves, and with the new nutritional assessment techniques that are feasible for the general pediatrician and the specialist, which can demonstrate the external validity of results.
FundingSARAH Network of Rehabilitation Hospitals, Brazil.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Araújo LA, Silva LR. Anthropometric assessment of patients with cerebral palsy: which curves are more appropriate? J Pediatr (Rio J). 2013;89:307–14.