The authors aim to evaluate the “point-of-care” transfontanellar ultrasound (TU) as an extension to pediatric physical examination and suggest a TU teaching protocol.
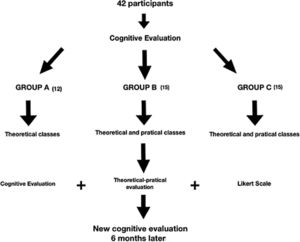
MethodsThe students were randomly divided into two groups, group A (12 participants) and group B (15 participants). The first group only received theoretical training, while the second group received theoretical and practical training. A third group, group C, included 15 pediatricians and interns who also received theoretical and practical training. All the participants underwent multiple-choice testing before and after a four-hour short course on TU. Six months later, another evaluation was performed to analyze the retained knowledge. Furthermore, a questionnaire based on the Likert scale was administered to evaluate satisfaction.
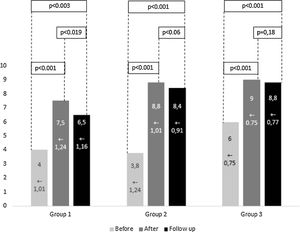
ResultsThe cognitive evaluation (maximum score=10 points) before and after training increased in group A from 4,0±1,04 to 7,5±1,2 (p<0.001) and, 6 months later, to 6,5±1,16 (p<0.003); in group B from 3,8±1,24 to 8,8±1,01 (p<0.001) and, 6 months later, to 8,46±0,91 (p<0.001); and in group C from 6,0±0,75 to 9,0±0,75 (p<0.001) and, 6 months later, to 8,8±0,77 (p<0.001). The average satisfaction estimated by the Likert scale was over 80% for all questions.
ConclusionCognitive assessment before and after classes and training reveals progress in learning, with knowledge retention in 6 months. Theoretical-practical courses are well accepted.
“Point-of-care ultrasound” (POCUS) has indispensable qualities that make it capable of answering specific questions in an interactive way.1,2 POCUS is a bedside technology that allows non-radiologist physicians to integrate physical examination findings with sonographic imaging.3,4
Unlike computed tomography (CT) and magnetic resonance (MR), ultrasound (USG) is less expensive, portable, and provides vascular or blood flow information, in addition to being noninvasive.4 Moreover, USG is a painless procedure that does not require the administration of medicines and is safe since it does not involve ionizing radiation.1,5–7
Proper use of POCUS provides image generation in real-time, which enables a quick diagnosis and provides guidance during procedures.8–12 Finally, the exams can be performed at any time and repeated several times, avoiding unnecessary tests, promoting better clinical decision-making, and decreasing medical errors.12–14
Pediatricians working in intensive care who have technical USG knowledge to recognize the main pathologies and urgent conditions using USG can be essential to patient prognosis.3,15 Furthermore, in recent years, USG has been more commonly used in medical education.16,17 In addition, USG methods are useful in many medical specialties, including pediatrics.18
Therefore, the objectives of the present study are to evaluate the inclusion of TU POCUS as an extension of the physical examination and to present a protocol for teaching medical students and novice users.
MethodsIn the current study, 27 medical students and 15 pediatricians (Fig. 1) without USG training were invited between 2018 and 2019 to perform bedside “point of care” TU on newborns from Terezinha de Jesus Maternity Hospital, Brazil. The pediatricians and interns in this hospital were enrolled if they met the inclusion and exclusion criteria. Inclusion criteria were that all medical students were, at the time of enrollment, in their second year of study and were familiar with neuroanatomy, but not with diagnostic imaging, which could influence the results.
Exclusion criteria were that subjects that had not agreed to participate, that had not performed all the research stages, or that had previously participated in USG training and were excluded from the study.
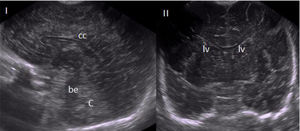
In addition, newborns from the hospital intensive care unit were only enrolled after legal guardians or parents provided written consent. Eight (8) healthy low-risk newborns were included in the study. The procedure was performed in the anterior fontanelle, with the patient in the supine position, and all images were taken in the coronal and sagittal planes. Students were expected to recognize the differences by the sagittal and coronal planes and to determine the corpus callosum, cerebellum, brain stem, and lateral ventricles (Fig. 2).
All those legally responsible were informed that the TU in this study would not replace comprehensive USG and that the method, being noninvasive and with minimal risk for patients, would be performed through the anterior fontanelle. There was no financial reward for parents or legal guardians, and the TU was performed with no obligation for the patients and complemented with additional examinations in case of suspicion for another diagnosis. Pediatricians’ and students’ performance and evaluation were not revealed to maintain confidentiality. The study was approved by the ethics committee.
Study protocolThe study was divided into stages for its realization. The medical students were separated into two groups, the A group (12 students) and the B group (15 students). The first group only received theoretical training, while the second group received theoretical and practical training to identify any additional factors that practical training could provide. The C group, which was formed by 15 pediatricians and interns, also received theoretical and practical training. Finally, all 42 selected participants were randomly distributed into 6 classes. All classes received the same teaching method and practice time, with the exception that group A did not receive practical training.
On the first day, before the course, there was a cognitive test lasting 15min, with ten questions (four choices each), to verify previous knowledge about neuroanatomy, USG, knobology, and neonatal pathologies. After the test, there was a theory class lasting 60min with a radiologist with more than 5 years of experience to teach the above knowledge. Later, there was a practical class and training lasting 60min, with a basic orientation about the theory relating to the use of USG devices, basic physics, main buttons and components, techniques to improve image resolution, and required measures for USG in pediatrics, with an emphasis on TU evaluation and “hands-on” practical demonstration in newborns. After this training, the participants were able to study the subject for 3 days. It is important to emphasize that all the groups had USG physical management, knobology, image adjustment, and TU classes, but only the B and C groups had hands-on sessions using an endocavitary probe with the GE Logiq-E device (Logiq-E GE 2014, Contagem, Brazil).
The next morning, there was a second meeting, where the main topics were reviewed with a lecture lasting approximately 15min. Then, the participants received an educational intervention to begin theoretical-practical training lasting 105min.
That afternoon, after the short course had been performed, there was a second cognitive multiple-choice test about USG aiming to evaluate knowledge evolution, using similar but not the same questions as the previous test. Later, on the same day, all participants underwent a theoretical-practical performance evaluation, composed of nine parameters (four alternatives each) in four domains: neuroanatomy (D1), knobology (D2), altered (hemorrhage, calcifications, hydrocephalus) TU images (D3) and normal TU images (D4).
In the cognitive and practical tests for the TU study, 70 points were set as the minimum score, which is the required grade to demonstrate competency in the subjects at our institution. If any of the participants did not achieve the required score, new training would be performed until everyone reached it. Finally, all participants answered a questionnaire based on a Likert scale about their satisfaction with the course. There were four sentences to determine their satisfaction on a scale from one to five.
Six months later, another cognitive evaluation was performed with the same students and pediatricians/interns to verify their knowledge retention.
In summary, the variables presented were: Improvement of the scores of the cognitive assessment; Evolution of the average grades 6 months after the course compared with the second test; Rate of correct answers in the image interpretation; Performance between Groups; Satisfaction evaluation and all that was described as a percentage.
The data were stored and analyzed using Stata 9.1 software (Stata Corp. College Station, United States). The descriptive analysis of the variables was presented using means and standard deviations. The normality of the data was assessed using the Shapiro-Wilk test. To compare the means of the test domains among the groups, the Kruskal-Wallis test was used, followed by the post hoc Bonferroni test. To determine if there was a change in the cognitive test before, after, and in the follow-up, ANOVA with repeated measures was used. The accepted level of significance was 5%.
ResultsA total of 27 students (Group A: mean age 22.58 years, 58.3% female; Group B: mean age 22.2 years, 60.0% female) and 15 pediatricians (Group C: mean age 31.1 years, 66.6% female) participated in the study. There were no differences between sex among the groups. Group C had an older average age than groups A and B, which were composed only of students.
Fig. 3 shows the improvement of the scores of the cognitive assessment from before the course and after its completion for the three groups (p<0.001). Fig. 3 also demonstrates the evolution of the average grades 6 months after the course compared with the second test, highlighting the drop in knowledge retention only in group A (p<0.0019). In all groups, there was significant retention of knowledge in relation to each first test (p<0.05).
The general rate of correct answers in the image interpretation, as shown in Table 1, was 75,9% in group A, 89,8% in group B, and 92,5% in group C (p<0.045). Then, we divided the questions about knowledge domains into D1 (neuroanatomy), D2 (knobology), D3 (altered TU exams), and D4 (normal TU exams).
Percentage of correctness in the evaluation by images and comparison between the different groups according to statistical relevance.
| Domains | Group A | Group B | Group C | GA×GB | GA×GC | GB×GC | Total |
|---|---|---|---|---|---|---|---|
| D1 | 94.4% | 95.5% | 97.7% | p=0.33 | p=0.10 | p=0.13 | p=0.341 |
| D2 | 75.0% | 93.3% | 97.7% | p<0.001 | p<0.001 | p=0.067 | p=0.012 |
| D3 | 66.6% | 90.0% | 96.6% | p=0.003 | p=0.004 | p=0.13 | p=0.007 |
| D4 | 41.6% | 60.0% | 66.6% | p=0.18 | p=0.25 | p=0.71 | p=0.98 |
| Total | 75.9% | 89.8% | 92.5% | p<0.01 | p<0.01 | p=0.355 | p=0.045 |
Table 1 demonstrates that the capacity to dismiss a completely normal exam was the parameter with the lowest success rate, with correct answers of approximately 41.6% in group A, 60% in group B, and 66.6% in group C. Table 1 highlights that the performance between Groups (A×B) and (A×C) was significantly different regarding the domains of knobology (D2), interpretation of pathological images by TU (D3) and in the total count (Total) (p<0.05).
The satisfaction evaluation by the Likert scale demonstrates that all questionnaire sentences had a global positive rate higher than 80%. Items: 1. The course meets expectations: 88.0%; 2. Practical theoretical training enables brain structures to be identified by TU: 97.5%; 3. TU should be included in medical education: 83.3%; 4. The participant has added knowledge and believes to be better able to evaluate a newborn’s brain: 80.9%. The second sentence about the capacity of structure identification in USG had the highest global positive rate (97.5%).
We developed a TU USG training protocol. TU indication criteria remain visible on the ICU general bulletin board. Every six months, transfontanellar USG classes are provided for pediatricians/interns. Once a week, all of the interns could watch a USG performed by a radiologist and should participate in case report discussions. Finally, the hospital-acquired the USG device and made it fully available to those who perform permanent training in POCUS (pediatric and adult ICU, anesthesiologists, and surgeons).
DiscussionThe main study findings were as follows: according to cognitive evaluation before and after classes, there was learning evolution, with knowledge retention for 6 months; practical training results in a higher number of correct answers and can influence knowledge retention; the capacity to dismiss a normal TU (Fig. 2) was the most difficult parameter for the participants; questions related to the technique of using the USG device were easily addressed and quickly learned by the participants; according to the satisfaction questionnaire, theoretical-practical short-courses are well received by the participants, with even higher results when there is a practical component; and the proposed teaching protocol was well received and can be an interesting way to improve hospital compliance.
In a study performed in 2011, 95% of emergency service departments in the United States of America (USA) that included “fellow” training programs performed some kind of service with “point-of-care” techniques, and 88% of specialized training programs provided specific training for this purpose.19 This study corroborates other research in the literature, such as the studies by Nunes et al. with intern physicians and Heinzow et al. with students, that demonstrates how USG short training has significantly improved cognitive evaluations before and after practical training.20
There is enormous variability in the protocols between several USG studies in medical education, and the necessary number of exams performed by professionals to reach a level of competence for safe and confident performance has not been established, although it is well known that practice examinations are effective in the evaluation of the participants’ knowledge.21,22
Many USG studies have involved medical students and physicians, and there has been an extensive utilization of practical simulations, including on real patients in emergency situations.22,23 Therefore, it was reasonable to predict that practical training would produce better results than only theoretical training, as our study has confirmed. Finally, as we observed in our study, determining that an exam is normal is, in fact, a complex and challenging task, even for those with experience in diagnosis, and only continuous training will produce a significant increase in technical knowledge and diagnostic confidence.24
There is not an established consensus about the duration of the course, which can be explained by the high variability in training that aims between the medical specialties, or about the need to obtain certification by medical societies. However, short courses have already demonstrated efficacy, as in the study by Thomas et al., which achieved excellent results after a single 8-h trauma course through didactic classes and practical training performed by surgeons.25
There is increasing interest in USG training among medical students and interns.26,27 Recent research about POCUS training and implementation between scholarship programs in the USA has suggested limited scope but high levels of interest.28,29 Therefore, our study corroborates the literature by demonstrating the high interest and acceptance for those courses, with positive satisfaction rates higher than 80% for all the questionnaire statements.
Our study had some practical limitations. First, it should be discussed that the number of participants is not large, although previous POCUS studies have a similar number of participants, and all of our hospital pediatricians and interns were selected (according to the inclusion and exclusion criteria) with equivalence in the number of students in the other groups. Second, the follow-up at six months may not be long enough to analyze knowledge retention; however, we obtained results with statistical relevance even with few participants and in a short evaluation time. Third, there is difficulty in the qualitative assessment of the ability of new apprentices to perform the USG, and only continuing education and continuous assessment can attest to the quality of POCUS courses. This is a pioneering study in developing the training and proficiency regimes necessary for the implementation of the POCUS protocol in an ICU with an emphasis on TU, as has been necessary for pediatric practice and emphasized in the literature.29,30
The point-of-care modality is already a reality in many hospital services around the world for most medical specialties. In pediatrics, the method has enormous importance since it is inherently safe, with no radiation emission and no drug administration. Finally, knowledge dissemination is necessary for the education of academics and physicians, and short courses have been considered effective regarding this dissemination, although it is necessary to emphasize permanent education and cooperation between different medical specialties. We reinforce that POCUS improves the pediatric physical examination, verified in this study through the TU and that it can be taught in short courses with serial monitoring of studies by a radiologist, which is fundamental whenever the pediatrician or clinician finds its limit on USG.
The protocol below is suggested according to the experience of the present study and bibliographic review:
- -
First day: cognitive test before the course and, after that, theory class and practical class lasting 60min each.
- -
Three days of personal study.
- -
Fifth day: review, cognitive test, and another theoretical-practical performance evaluation.
- -
Monitor the performance and perform TU exams at least once a week.
- -
Every six months: another cognitive test.
Finally, we suggest if any author wants to replicate the study that adds a fourth group with physicians that already know the method and perform TU. This would allow new comparisons between subgroups with different degrees of knowledge.
Conflicts of interestThe authors declare no conflicts of interest.