To evaluate the association between dose of skin-to-skin contact (SSC) per day and initiation time with the occurrence of deaths in newborns with weight up to 1800g.
MethodMulticentric cohort in five Brazilian neonatal units, including newborns with a birth weight of ≤1800g. The time of SSC was registered in individual file, by the team or family during the hospitalization. Maternal and newborn data were obtained through questionnaires applied to mothers and in medical records. Classification Tree was used for data analysis.
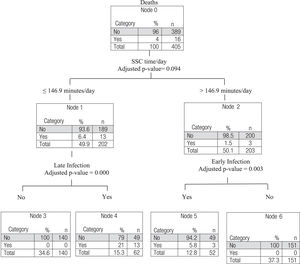
ResultsThe performance of the first SSC after 206h was significantly associated with death (p = 0.02). Although there was no association between SSC/day and death (p = 0.09), the number of deaths among those who performed more than 146.9 minutes/day was lower (3;1.5%) than among those who performed this practice for a shorter time (13;6.4%), a fact considered of great clinical importance. Early and late infections present statistically significant associations with the outcome. The chance of death was equal to zero when there was no early infection in the group with the longest duration of SSC. This probability was also equal to zero in the absence of late sepsis for the group with less than 146.9 minutes/day of SSC.
ConclusionsThe first SSC before 206 hours of life is recommended in order to observe a reduction in the risk of neonatal death. Staying in SSC for more than 146.9 min/day seems to be clinically beneficial for these neonates mostly when it was associated with the absence of infection.
Despite the global reduction in the number of deaths among children during the first month of life, neonatal mortality rates remain high. In 2018, there were about 2.5 million deaths worldwide in this stage of life, representing 47% of deaths among children under five and a global rate of 18 deaths per 1000 live births. In Brazil, estimates are of 8 neonatal deaths per thousand live births, in the same year.1
The complications related to premature birth are the main cause of neonatal deaths.2,3 and in Brazil account for 28% of neonatal deaths, followed by severe infections (26%) and asphyxia (23%). Low birth weight is an important indirect cause of death.4
The reduction in neonatal mortality is linked to greater investments in coverage and improved quality of prenatal, childbirth, and birth services.5 Good newborn care practices have been disseminated in order to improve the quality of neonatal care and reduce negative outcomes. Among these, skin-to-skin contact (SSC) has gained relevance. It consists of placing the newborn in direct contact with the skin of the mother or father's chest, in an upright position, only in diapers, especially in premature and low birth weight newborns.6
Different studies have shown consistent benefits in neonatal outcomes associated with SSC practice such as maintenance of body temperature, stabilization of vital signs, increase in exclusive breastfeeding7-11 reduction of mortality, risk of infection/sepsis, hypothermia, hypoglycemia, and hospital readmissions.8 In addition, there are reports of psychological benefits related to the creation of the mother-baby bond with better availability of the newborn for interactions with its mother.12,13
Although scientific evidence has already demonstrated the association between the practice of SSC and better neonatal results, few studies have taken into account the dose and the time until the first performance of this practice.10,14 It is not clear how long this practice should be in order to reduce the chance of death during hospitalization, as well as the influence of the early introduction to SSC to reduce these rates. Such knowledge could guide more specific recommendations on this practice and contribute to the reduction of neonatal mortality. The objective of this study was to assess the association between the dose of SSC per day and the time until first exposure to this practice, and the occurrence of deaths in newborns weighing up to 1,800 grams.
Materials and methodsA prospective multi-centric cohort study was conducted from 05/2018 to 03/2020 in five Brazilian neonatal units from different regions of the country: two in the Northeast, two in the Southeast and one in the South.
Inclusion criteria included live births, single births, and newborns weighing ≤1800 grams without comorbidities, such as malformations, severe perinatal asphyxia, and genetic syndromes. Non-inclusion and exclusion criteria, as well as losses, are detailed in the sample flowchart (Supplementary Material).
The definition of a cutoff point of ≤1800 grams took into account an observation of a pilot study that showed that NB with higher weights spent less time in the NICU, which could interfere with the observation of the effect of SSC on the outcome under study.
The sample calculation was based on a pilot study and considered a frequency difference of the outcome between exposed and unexposed groups of 8%, using a power of 80% and a confidence interval of 95%. The minimum sample size was estimated at 356 individuals.
Demographic and socioeconomic data of mothers and fathers were obtained through questionnaires designed by the researchers. Data on the evolution of the newborn were collected from medical records and with the direct investigation. The SSC time was recorded on cards attached to the bed by the health team at the beginning of the admission of the newborn. Then, parents received specific training to perform the registration, under the supervision of health professionals. This card notes the beginning and end of each contact, the period of the day in which it occurred, and the frequency and time individually performed by the father and/or mother. These records were consolidated daily by research assistants during the newborn's hospitalization period, ensuring the quality of the collection.
The following variables of the mother were included: age; schooling; marital status; adequate prenatal care15; use of antenatal corticoid; occurrence of Specific Hypertensive Pregnancy Syndrome; infection; use of alcohol during pregnancy and type of delivery. Variables of newborn included gestational age at birth (calculated by the date of the last menstruation or by the ultrasound of the first trimester or by the New Ballard clinical examination); weight at birth; weight adequacy for gestational age (categorized in AGA, SGA, or LGA)16; Score for Neonatal Acute Physiology - Perinatal Extension II (SNAPPEII), evaluated prospectively within the first 12h of admission after stabilization17; start time of the first SSC in days (started after the clinical stabilization of the newborn, as recommended by the WHO)18; total time of SSC in minutes; Apgar in the fifth minute; the presence of early infection (< 48 hours of life); late infection (≥48 hours of life)19; length of stay in days; time of use of pulmonary mechanical ventilation (PMV) and time of use of total parenteral nutrition (TPN).
The collected data were tabulated in a Google Form tool and then exported to a Microsoft Office Excel spreadsheet, version 2016. Quantitative data were represented by the mean and standard deviation or medians and interquartile ranges, depending on the normality distribution criteria. Categorical variables were presented in frequencies and percentages.
For statistical analysis of the association between SSC time and neonatal death, the Classification Tree method was used. This method elaborated an efficient explanatory model through the relationships between the variables, in which the classes were established automatically, based on the available data and the logistic expression of the relationships.
SSC time, the main variable of interest in this study was prioritized in the analysis, that is, the program was asked to insert this variable in the model as the first attribute of the Classification Tree. Then, it was observed which variables would be significantly associated with the investigated outcome. This type of tree differs from the one that would be generated without the requirement of including a certain variable, where only statistically significant subdivisions would be represented.
The Classification Tree started with the main neonatal death outcome, which was divided into others, representing new categories that explained the behavior from this variable. Each subdivision had its level of significance measured in relation to the previous variable. When a node was no longer divided the set of variables and their subdivisions were identified, which explained the evolutionary and associative context of neonatal death.20
The cut-off points that determine the subdivisions of the nodes were established by the statistical program and based on significant values. In addition, it related the independent variables with the others, establishing the associations of greater logistic sense.
To establish a statistical association, significance levels were set at 5% and 95% confidence intervals (95%CI) were adopted. Stata® 14.0 and SPSS® 21 statistical packages were used.
The multi-centric study was approved by the Ethics in Research Committee (ruling number 2.570.959/CAAE n° 83803817.0.1001.5086).
ResultsAmong those eligible for this study, three infants didn't undergo SSC due to the seriousness of the clinical condition with evolution to death after the first week of life and one case in which the mother opted for conventional care. Four hundred and five (405) newborns participated in this study with an average gestational age of 31.3 ± 2.7 weeks and 1369.7 ± 297.3 grams. The median time to perform the first SSC was 5 days and the median time of use was 147.02 minutes/day. Other characteristics of the infants are shown in Table 1. Maternal characteristics are described in Table 2.
Characterization of newborns weighing up to 1800g (n = 405) hospitalized in neonatal units.
| Variable | |
|---|---|
| Male Sexa | 208 (51,4%) |
| Weight (grams)b | 1.369,7 ± 297,3 |
| Gestational age (weeks)b | 31,3 ± 2,7 |
| Small for gestational agea | 139 (34,3%) |
| Adequade for gestational agea | 257 (63,5%) |
| Apgar 5th minuteb | 8,5 ± 0,93 |
| SNAPPE IIc | 5 (0-15) |
| Early Infectiona | 105 (25,9%) |
| Late Infectiona | 118 (29,1%) |
| Hospitalization period (days)c | 34 (25-52) |
| Death ratea | 16 (4,0%) |
| 1st Skin to skin contact (SSC in days)c | 5 (4-8) |
| Total skin to skin contact per day (minutes)c | 147.02 (106,73-263,05) |
SNAPE II, Score for Neonatal Acute Physiology - Perinatal Extension II.
Demographic, socioeconomic and gestational characteristics of mothers of newborns weighing up to 1800g (n = 405) admitted to neonatal units.
ES, elementary school; HS, high school; SHPS, specific hypertensive pregnancy syndrome.
According to the Classification Tree algorithm, the cutoff point of exposure to SSC capable of reducing the probability of death from 6.4% to 1.5% was 146.9 minutes/day, although this difference was not statistically significant (p=0.09). Starting from the variable “SSC time” in the Tree, there were statistically significant associations with early and late infection. If the newborn didn't present early infection, the chance of neonatal death was equal to zero when SSC was > 146.9 minutes/day. In the case of those who spent less time in the SSC (≤ 146.9 min/day), the chance of death was 6.4%, and among those who didn't have a late infection, this chance was equal to zero (Figure 1).
Figure 2 shows the classification tree for the occurrence of death in relation to the time elapsed until the first SSC. This tree shows the first subdivision with a cutoff point of 206 hours, approximately 8.5 days. The difference between the groups with more or less time for the first SSC was significant (p-value = 0.013). The chance of death varied from 2.5% among those who started SSC earlier to 9.9% among those who started later. In the group that initiated the first SSC before 206 hours, the time of pulmonary mechanical ventilation (PMV) was determinant for the death outcome (p < 0.001). The chance of death was 12.1% in the group with the longest PMV utilization time and zero among those who used this technology for less than 2 days.
DiscussionThe number of neonatal deaths among newborns who underwent more than 146.9 min/day was smaller SSC than among infants who did so less time (13:6.4%), although this association wasn't statistically significant. Among children who had had a longer SSC/day and had no diagnosis of early infection the chances of progressing to death were zero, while among those who had shorter periods and developed a late infection, the probability was 21% for this outcome (Figure 1). On the other hand, there was a strong association between earlier first SSC (≤ 206 hours) and a lower chance of death. Longer time to start of the first SSC represented a nearly four times greater chance of death. The explanation of death included the variable PMV. Performing more than two days of mechanical ventilation showed a statistically significant association with death among infants that started SSC earlier (Figure 2).
Neonatal deaths are responsible for 45% of the mortality in children under the age of 5 years worldwide, and 18% of these deaths may occur due to complications of prematurity.21 SSC is an effective strategy to reduce these rates.8-22 In the present study, the authors didn't evaluate the association between doing and not doing SSC, but doing it for more or less time. For this analysis, the authors used the cutoff point of 146.9 min/day minutes, determined by the classification tree algorithm. At first, no statistical association with this variable alone was observed. However, the authors found a reduction in the absolute number of deaths from 13 to 3 among those who had a mean time longer than 146.9 minutes/day of SSC. The authors of the present study consider this fact to be of great clinical relevance since it represents the chance to avoid 10 deaths in this population.
Although “SSC time” wasn't a statistically significant variable associated with death, it was observed that in the subdivisions, after nodes 1 and 2, the variables “late infection” appeared as relevant explanatory components, for those who practiced less than 146.9 min/day of SSC, and “early infection” for those with an average above 146.9 min/day.
The analysis detected these two variables as being of great importance in explaining the death outcome. Following the subdivision of node 1, the absence of a diagnosis of late infection among these children presented a chance of death equal to zero in relation to those with this diagnosis. Similarly, among those who did more SSC time, the non-occurrence of early infection implied a chance of death equal to zero comparing to those with this kind of infection.
There is a correlation between the classification tree and clinical logic. The literature shows that late and early neonatal infections are important risk factors for neonatal death.23,24 In this study, late infections were strongly associated with death among those who had less than 146.9 minutes of SSC on average per day, and the presence of early-onset infection, of maternal origin, were associated as an explanation for deaths among those who had a mean SSC higher than 146.9 min/day.
Nodes 3 and 4 of classification three indicate that all deaths occurred among late-infection newborns, which is possibly the cause of these deaths. Thus, it is plausible to think that a shorter time of exposure to SSC was probably a risk factor for late sepsis death in the Neonatal Unit, and conversely, that a longer time of SSC could play a protective role in relation to late sepsis in these newborns. This reasoning was corroborated by Lamy-Filho et al.25 in 2015 in a randomized clinical trial, where it was demonstrated that preterm neonates submitted to SSC for seven days, two hours a day, had more than twice the chance of decolonizing from their multi-drug resistant flora than the control group, which didn't experience this practice. Other studies also point to a reduction of late infection among newborns exposed to SSC.8,14,22,26
The presence of early neonatal sepsis was associated with a risk for deaths among those who had practiced longer SSC. However, these children, having presented early in life a sequence of problems, probably didn't undergo SSC in the first 72 hours. Thus, the authors cannot evaluate a possible protective effect of SSC in this group of children in relation to death, even though they had practiced longer SSC.
The exposure time after which the authors can observe the effect of SSC in relation to death, considering the presence of early or late sepsis, seems to be around an average cutoff point of 146.9 minutes of exposure per day. This raises the possibility that the effect of the use of this practice, in relation to neonatal death is found when the average SSC per day is close to two and a half hours.
Although the literature has demonstrated the beneficial effects of SSC, there is a large variation in the time of use of SSC in several published works, which point from continuous use (above 20h per day)22,26 to shorter time, such as two hours a day.12,25,27 Although it isn't possible to make a formal recommendation, the present study's results point to the cut-off point of 146.9 minutes of SSC dose, from which the best results could be achieved during hospitalization, especially among newborns who were not diagnosed with late-onset sepsis. In addition, this work shows that the nosocomial infections in neonates that didn't achieve this amount of time of SSC are of great importance.
In the present study, it was found that newborns that experienced these first SSC later (> 206 hours) had a chance of dying almost four times higher than those that started earlier (Figure 2). These data show that the earlier the newborn is submitted to SSC, the greater are the benefits of this practice. It is possible that the severity of admission results in greater chances of death, and, at the same time, promotes a delay in the onset of SSC. However, this fact does not seem to be the main determinant for the late introduction of SSC, since newborns with worse severity, that is, those who died in the first week of life, were excluded from the study.
An important recommendation for the present study's results is to avoid a late start of SSC. The analysis of the classification tree showed that an SSC initiation after 206 hours (around 8 days) points to a nearly 4 times higher risk of neonatal death than the earlier practice. A multicenter trial reinforced the importance of early SSC by demonstrating a 25% reduction in the chance of neonatal death among infants with a birth weight between 1000 and 1799g who started SSC before clinical stabilization.26 In contrast, the present study maintained the current recommendation to carry out this contact only after clinical stability of newborns,18 and also included those weighing less than 1000 grams and/or with respiratory problems using ventilation support. However, it is observed that both studies point to early exposure as a preponderant factor for the occurrence of death, either before or after clinical stability is reached.
The present study's results also show that, even among newborns submitted to early SSC, those who used mechanical ventilation for more than 2 days had a much greater chance of death, probably because they were part of a group of neonates with more severe diseases.
The main limitation of this study was that some of the records the authors used were documented by the parents, which could introduce some measurement bias. However, all the records were checked and supervised by the team every day, which minimized this possibility. Although the choice of participating institutions wasn't randomized, the authors believe they accurately exemplified the reality of the practice of SSC in Brazil. Another possible limitation was that the neonatal units in this study were not evaluated as an independent variable, which may have influenced mortality analysis.
The multi-centric character of this study has contributed to a better comprehension of the reality of SSC practice in Brazil. Other strengths of this study were also its prospective cohort design and the use of the “Classification Tree” analysis, which allowed observing cut-points of the time of use SSC related to the outcome in question and creating explanatory models for the occurrence of deaths in the population studied.
This study methodology resulted in a greater understanding of the relationship between the amount of SSC and neonatal death by examining the role of each element involved in the outcome. It was also possible to determine how early the first SSC must be in order to observe its protective effects. Early SSC can be an effective strategy to contribute to the reduction of neonatal mortality.
Other robust studies on the regularity and frequency of SSC practice during neonatal admission related to these and other outcomes are still needed.
FundingThis research has received funding from the Foundation for Research and Technological Development of Maranhão (FAPEMA), the National Council for Scientific and Technological Development (CNPq) and the Coordination for the Improvement of Higher Level Personnel (CAPES) - Finance Code 001.
The authors of the present study thank the health professionals of the participating Units and the parents for their availability.
Study conducted at Universidade Federal do Maranhão, Departamento de Saúde Pública, São Luís, MA, Brazil.