After the Covid-19 pandemics hit Brazil and sanitary measures were adopted to contain its dissemination, pediatric hospital admissions were apparently fewer than usual. The authors aimed to describe the time trends of public hospital admissions of children and adolescents due to respiratory infections (RIs) in São Paulo State, Brazil, before and after the adoption of sanitary measures to contain the dissemination of Covid-19.
MethodsEcological, time-series study on the monthly average number of admissions per day of children and adolescents (< 16 years) admitted to public hospitals of São Paulo due to acute RIs between January 2008 and March 2021. Data from 2008 to 2019 were used to adjust the statistical model, while data from 2020 and 2021 were compared to the values predicted by the model.
ResultsIn 2020 and 2021, the number of hospital admissions was significantly lower than predicted by the time series. However, lethality was three times higher in these years, compared to the previous, and six times higher in patients with Covid-19, compared to those without the disease. Hospitalization costs in 2020 and 2021 were lower than in previous years.
ConclusionsThese findings suggest that the sanitary measures adopted to contain the dissemination of Covid-19 also effectively reduce the transmission of other respiratory viruses. Policymakers and administrators can use this knowledge as a guide to planning preventative interventions that could decrease the number and severity of RIs and related hospital admissions in children and adolescents, decreasing the burden on the public health system.
Respiratory infections (RIs) are a significant cause of morbidity and lethality in children worldwide, especially in those younger than five years,1 comprising about one-third of all pediatric appointments in the United Kingdom in 2018.2 Healthy children, especially those at school ages, experience up to ten episodes of RIs per year.2 The etiologic agents of acute RIs differ according to age and region, possibly because of climatic, geographical, and cultural factors.3 In China, well-defined seasonal patterns have been identified for RIs caused by a respiratory syncytial virus (RSV), influenza, parainfluenza, human metapneumovirus, Moraxella catarrhalis, and Haemophilus spp. Among these, RSV was the most frequent in children aged less than two years.3 It was responsible for 33.8 million episodes of acute RIs in children below five years worldwide, with 3.2 million hospitalizations and almost 60 thousand deaths in 2015.4 The seasonality of RSV infection is well established, spanning from March to July in the Southern hemisphere and from September to December in the Northern hemisphere.4 In Brazil, regional differences have been described, with a peak incidence in April in the Northern, Southeastern, and Mid-Western regions, in May in the Northeastern region, and in June in the southern region.5
However, this scenario was strikingly changed by the SARS-Cov-2 and coronavirus disease (Covid)-19 pandemics,6 which reached Brazil in 2020. From this moment on, several measures were taken in all countries to stop or slow down the virus transmission, such as the use of personal protection equipment (PPE), avoiding contact with respiratory secretions, early identification and isolation of patients with suspected infection, suspension of presential classes in all schools, and social distancing and isolation of apparently healthy people.7 In Brazil, these measures were adopted according to each State's regulations as the number of suspected, and confirmed cases rose. In São Paulo State, social distancing started on March 22nd, 2020.8 In April, when all pediatric emergency departments in São Paulo were expecting a high number of children with RIs, including Covid-19 cases, surprisingly, the number of patients was much lower than expected. This apparent reduction in the number of RIs in children observed in 2020 could have been a consequence of the measures taken to slow down the dissemination of Covid-19, but this relationship was not assessed so far, to the best of our knowledge.
Therefore, this study aimed at testing whether the number of hospital admissions of children and adolescents of up to sixteen years, in public hospitals from São Paulo State, Brazil, due to RIs, decreased in 2020 when compared to previous years and whether this decrease has a temporal relationship with the adoption of measures taken to slow down the dissemination of Covid-19.
MethodsThis was a time-series, ecological study on the monthly average number of hospital admissions per day in public hospitals of São Paulo State, Brazil, between January 2008 and March 2021. The upper limit of 16 years of age was chosen because it includes almost all children and adolescents of school age. Data were obtained from the Brazilian database on hospital admissions in the public health system (SUS) – DATASUS (http://www2.datasus.gov.br/). The database was created in 1991. All data are filled in by the admitting physicians, including main and secondary ICD codes, and are reviewed at discharge by the attending physician and administrative staff. These data are used for epidemiological research in different areas. A simple search for the term DATASUS in Embase (embase.com, November 2021) results in 699 entries. Since DATASUS is a publicly available, anonymized database, this study was waived from analysis and approval by the institutional ethics review board.
Files (.dbc, database container, 159 files) containing all hospital admissions in public hospitals of São Paulo State were downloaded from DATASUS for each month in the selected period. Included “read-me” text files contained instructions for using the database along with the codebook. The database files were converted to comma-separated values (.csv) files with R® software 4.0.5 (The R Project for Statistical Computing, www.r-project.org/), and then imported into a MySQL® (www.mysql.com) database. The following variables were selected for this study: state (UF_ZI), year (ANO_CMPT), month (MÊS_CM), medical specialty (ESPEC), city (MUNIC_R), birth date (NASC), sex (SEXO), total admission cost (VAL_TOT), admission date (DT_INTERN), discharge date (DT_SAIDA), main diagnostic (DIAG_PRINC), age (IDADE), length of hospital stay (DIAS_PERM), death (MORTE), race (RACA), ethnicity (ETNIA), and secondary diagnostics 1–9 (DIAGSEC 1–9). Non-selected variables were dropped from the database.
The variables “main diagnostic” and “secondary diagnostics” contained the International Classification of Diseases, version 10 (ICD-10) codes for each patient. The ICD-10 codes of interest as main diagnostics were: (A) Acute upper and lower respiratory tract infections: J00 (Acute nasopharyngitis [common cold]), J02 (Acute pharyngitis), J03 (Acute tonsillitis), J04 (Acute laryngitis and tracheitis), J06 (Acute upper respiratory infections of multiple and unspecified sites), J10 (Influenza due to other identified influenza virus), J11 (Influenza, virus not identified), J20 (Acute bronchitis), J22 (Unspecified acute lower respiratory infection), J39 (Other diseases of upper respiratory tract), and J40 (Bronchitis, not specified as acute or chronic); (B) Pneumonia: J12 (Viral pneumonia, not elsewhere classified), J13 (Pneumonia due to Streptococcus pneumoniae), J14 (Pneumonia due to Haemophilus influenzae), J16 (Pneumonia due to other infectious organisms, not elsewhere classified), J17 (Pneumonia in diseases classified elsewhere), and J18 (Pneumonia, organism unspecified); (C) Asthma: J45 (Asthma), and J46 (Status asthmaticus); (D) Other respiratory diseases: J44 (Other chronic obstructive pulmonary disease), J98 (Other respiratory disorders), and U04 (Severe acute respiratory syndrome [SARS]); and (E) Infections by coronaviruses: B34.2 (Coronavirus infection, unspecified site), and B97 (Viral agents as the cause of diseases classified to other chapters).
The next step was applying the inclusion criteria, which were: the main diagnostic with any of the ICD-10 codes of interest, and age < 16 years (Fig 1). The final database was then exported to a Microsoft Excel® (Microsoft Corporation, Redmond, CA, EUA) file (.xlsx), which was used for a final, manual database check and importing into the statistical software.
Statistical analysisDescription of all patients and their hospital admissions included in the analysis was made by calculating means [with standard deviations], medians (with interquartile ranges), or absolute and relative frequencies (percentages). Statistical software Stata SE 14.0 (StataCorp LLC, College Station, Texas, USA) was used in this step. The monthly average number of admissions per day was calculated by dividing the number of hospital admissions of children and adolescents <16 years old that contained a diagnostic of acute RIs within the time frame by the number of days in the corresponding month. February was set to 29 days in leap years. A generalized additive model (GAM) was proposed to model the time-series data of the monthly number of hospital admissions per day. GAMs are like generalized linear models, but they consider one or more terms as non-parametric smoothing functions. These models are very flexible in adjusting to time-series data, mostly because they do not have assumptions required by classic models, such as stationarity. Thus, considering that Y is the monthly mean number of hospital admissions per day, the average of the dependent variable Y is given by E(Yi)=µi and, using a link function g(µi), the adjusted model was µi = β0 + s1(trend) + s2(month) + s3(year), where s are the non-parametric smoothing functions, the trend is the series trend, and month and year are the corresponding month and year of the admissions. After the model adjustment, among several different smoothing functions, the authors selected the cyclic cubic regression splines function, as per the Akaike (AIC) criteria. Additionally, after checking the autocorrelation plots (ACF and PACF), an order-2 autoregressive parameter was inserted to remove the correlation between successive admissions. This model was adjusted for the years 2008 to 2019, while predictions were made for 2020 and 2021 to show that the predicted values would be different than the observed. The predicted values with respective 95% confidence intervals (CI) were calculated. Statistical software R®4.0.5 (The R Project for Statistical Computing, www.r-project.org/) was used with mgcv package.9
ResultsA total of 32,581,056 admissions were present in the initial database. After the application of the inclusion criteria, 771,001 hospital admissions were included in the analysis (Fig 1). Demographic and clinical data of the patients, along with their main outcomes, are depicted in Table 1.
Demographic and clinical characteristics and main outcomes of children and adolescents (< 16 years) admitted to public hospitals because of respiratory infections in São Paulo State, Brazil, between January 2008 and March 2021.
Source: DATASUS (http://www2.datasus.gov.br). Legend: A) ICD: J00, J02, J03, J04, J06, J10, J11, J20, J22, J39, and J40; B) ICD: J12, J13, J14, J16, J17, and J18; C) ICD: J45 and J46; D) ICD: J44, J98, and U04; E) ICD: B34 and B97. Data are expressed as median (interquartile range) or counts (percentages).
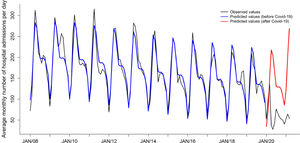
The observed monthly average numbers of hospital admissions per day in each year are plotted in Figure 2 (black line). Of note, there was a clear seasonal pattern with peak numbers occurring in April and May and a clear, progressive decrease over the years. The blue line corresponds to the values adjusted by the statistical model, and the red line corresponds to the predicted values after January 2020, when the observed values were significantly lower than the predicted by the model (below the 95%CI lower limits, presented in Table 2).
Observed and predicted (with 95% confidence intervals) monthly average number of public hospital admissions per day of children and adolescents (< 16 years) due to respiratory infections in São Paulo State, Brazil, between January 2008 and March 2021.
LL, lower limit; UL, upper limit.
Values are expressed in admissions per day.
Lethality in this time series ranged from 0.40 to 0.55% between 2008 and 2019 whereas, in 2020, it was 1.09% and, in January through March 2021, it was 1.34%, almost a three-fold increase. Between January 2020 and March 2021, the lethality of patients with a diagnostic of Covid-19 was 4.66%, more than six times higher than in those without Covid-19 (0.74%).
The amount of money paid by SUS for hospital admissions of children and adolescents < 16 years because of RIs ranged from 10.9 to 33.5 million dollars per year between 2008 and 2019. In 2020, this amount was only 4.9 million dollars (Supplementary Figure 1). On the other side, the mean reimbursement paid by SUS for these hospitalizations decreased from 2008 to 2015 but has been relatively stable from 2015 to 2021 (Supplementary Figure 2).
DiscussionThis study showed that after measures to contain Covid-19 dissemination were adopted, in 2020, there was a significant decrease in the number of public hospital admissions due to RIs in children and adolescents < 16 years in São Paulo State, Brazil, when compared to a historical time series. The hospitalization costs paid by SUS were much lower as well. Besides, lethality in these patients increased three times in 2020, and patients with Covid-19 had six-fold higher lethality. These results support the hypothesis that sanitary measures to control Covid-19 were effective in decreasing the transmission not only of Covid-19 but also of other respiratory agents in children and adolescents and, consequently, the number of hospitalizations caused by RIs in this age group.
One must take into consideration the fact that the number of hospitalizations was already decreasing over the years. This can be explained by improvements in the education of patients and the general population, increasing adherence to hand hygiene (with soap or alcohol-gel), better sanitary conditions of the population, but also by the universal vaccination against Influenza and Pneumococci (10-valent) initiated in Brazil in 2009 and 2010, respectively.10,11 After these vaccines were incorporated into the national vaccination program, hospitalization rates in children decreased.10,11 In developed countries, such as the United States, McAllister et al. (2018) demonstrated that, after the release of the 13-valent pneumococcal vaccine, in 2010, there was a reduction in hospitalization rates due to pneumonia from 14 to 4 per 1,000 children below two years of age.12,13 In Santa Catarina State, Brazil, another study assessed the impact of the adoption of the 10-valent pneumococcal vaccine on the hospitalization rates due to pneumonia and found a 23.3% decrease in the number of hospitalizations in children below one year of age and an 8.4% decrease in children of one to four years.14 Another possible explanation for the lower-than-expected number of pediatric hospitalizations due to RIs in 2020, even in the months of peak incidence of RIs in children, includes lower transmission rates of other respiratory viruses.15 This phenomenon can be attributed to crossed immunity between respiratory viruses, but it is more likely caused by improved personal and hand hygiene practices, use of face masks, and social distancing and isolation.16 However, the individual contribution of each sanitary measure for this effect is yet to be determined.17
In 2019, an extreme severe weather event occurred in Western Washington State, USA, leading to school closure, revealing that intensive and brief measures of social distancing and isolation can significantly decrease the incidence of RIs if implemented close to the epidemic peak.18 This was also observed during the Covid-19 pandemics, in which punctual, brief interruptions in normal activities (“lockdowns”) effectively reduced the number of cases and deaths by Covid-19.19 In this direction, the authors speculate that the present study'sfindings, along with the knowledge accumulated over the last year of Covid-19 pandemics, can be used to propose changes in school vacation and holidays so that they precede or coincide with the months of peak incidence of RIs in Brazil. The authors believe that such changes could significantly reduce the burden of RIs in children and adolescents, in terms of morbidity and mortality, and on the public health system, in terms of overload and costs. For example, the usual two-week school holiday in July, in Brazil, could be anticipated to April, the month with the highest numbers of hospital admissions, including by RSV, in São Paulo State.5
Mortality by Covid-19 in children is low when compared to adults: Covid-19 was responsible for only 0.48% of all deaths in children and adolescents < 19 years in seven countries, resulting in a mortality rate of 0.17 per 100,000 until February 2021.20 However, in the present study, although the overall number of pediatric hospital admissions was lower in 2020, lethality was three-fold higher. The authors initially speculated that this increase in lethality could be, at least in part, attributed to the overload in the public health system with adult cases of Covid-19, which resulted in healthcare providers and equipment being transferred to units caring for severely ill adults with Covid-19, leaving pediatric units with fewer professionals and resources. Another explanation could be a late presentation of patients to the emergency departments because of concern of contamination by Covid-19 or late referral to tertiary-care centers because of shortage of beds. However, the authors also showed that lethality in pediatric patients diagnosed with Covid-19 was six times higher than in those without this ICD-10 code. This finding suggests that Covid-19 is responsible for some part of the increased lethality in 2020 and 2021. Moreover, the few admission recorded for Covid-19 were probably in the more severe end of the disease spectrum. In 2021, Oliveira et al described similar results.21 The present study, however, was not planned to answer these questions.
The question of the hospitalization costs is more complicated. Along the years, the total amount paid by SUS to public hospitals decreased (Supplementary Fig. 1) not only because there were few admissions (Fig 2), but also because the reimbursement for each hospital admission decreased from 2008 to 2015 (Supplementary Fig. 2). This does not mean that the patients became less complex with time, but that the hospitals are chronically underfunded by SUS, which pays prefixed values (by the Government) for this. Thus, the decrease in hospitalization costs seen from 2008 to 2015 (Supplementary Fig. 1) can be attributed, at least in part, to the decrease in the reimbursement per hospital admission, but not from 2015 on. Of note, the dramatic fall in the number of hospital admissions seen in 2021 was not accompanied by a proportional decrease in hospital costs, which may be explained by the higher complexity of patients admitted in 2021.
Altogether, the present study's findings bring the discussion about how the authors can foster the adoption of preventative measures that significantly impact the morbidity of children and adolescents, as well as fewer ICU admissions and fewer deaths from RIs in these patients.
One strength of the present study is the use of a solid, comprehensive public database, with information on all hospital admissions in public hospitals in São Paulo State. This same fact brings the major limitation of this study, which is the use of a secondary data source, subject to information bias and underreporting mostly. Since data are entered by physicians and reviewed by administrative staff, there is a risk of some hospitals manipulating data to maximize billing to the health system. Nevertheless, given the enormous volume of data, these problems end up diluted. Another strength was the analysis of a time series with GAMs, allowing to describe trends, accommodate seasonal variations, and predict future values in the series. These models are flexible regarding the assumptions of classic models for time-series, besides easier insertion of independent variables and better adjustment to the different shapes that time-series data can assume. Therefore, the model's fit to the actual data was very good. Another limitation of the present study is that the authors did not analyze data from private hospitals. Therefore, the authors’ conclusions cannot be completely generalized to the private health system. On the other hand, the mean age of the patients included in this study is similar to those described in other publications on the global impact of RIs in children, as well as the predominance of boys, making the study's findings fairly generalizable.14,22,23
In conclusion, the sanitary measures adopted in Brazil in 2020 to slow down the transmission of Covid-19 resulted in a significant decrease in the number of public hospital admissions due to RIs in children and adolescents < 16 years in São Paulo State when compared to previous years. This knowledge can be used in the future to implement practices, such as changes in school vacancy and holidays, long-term incorporation of hand hygiene, social distancing, and other measures that can decrease the transmission of other respiratory agents, reducing the burden of RIs on this age group and the public health system.