Assess the mediating role of breastfeeding self-efficacy in the association between the Kangaroo Neonatal Intermediate Care Unit and exclusive breastfeeding.
MethodCross-sectional study nested in a cohort, carried out in the Neonatal Unit of a Brazilian university hospital between September 2018 and March 2020. The sample consisted of 114 newborns weighing ≤1800 g and their mothers who were divided into those who participated in the first and second stages of the Kangaroo Method and those who only passed through the first stage, categorized as the Conventional group. To assess the self-efficacy of breastfeeding, the Breastfeeding Self Efficacy Scale - Short-Form was used. The Mann-Whitney test was used to compare the breastfeeding self-efficacy score between the groups, and Fisher's exact test to compare rates of exclusive breastfeeding. The adjusted structural equation model was used to check for the mediating effect of breastfeeding self-efficacy. The significance level adopted was 5%.
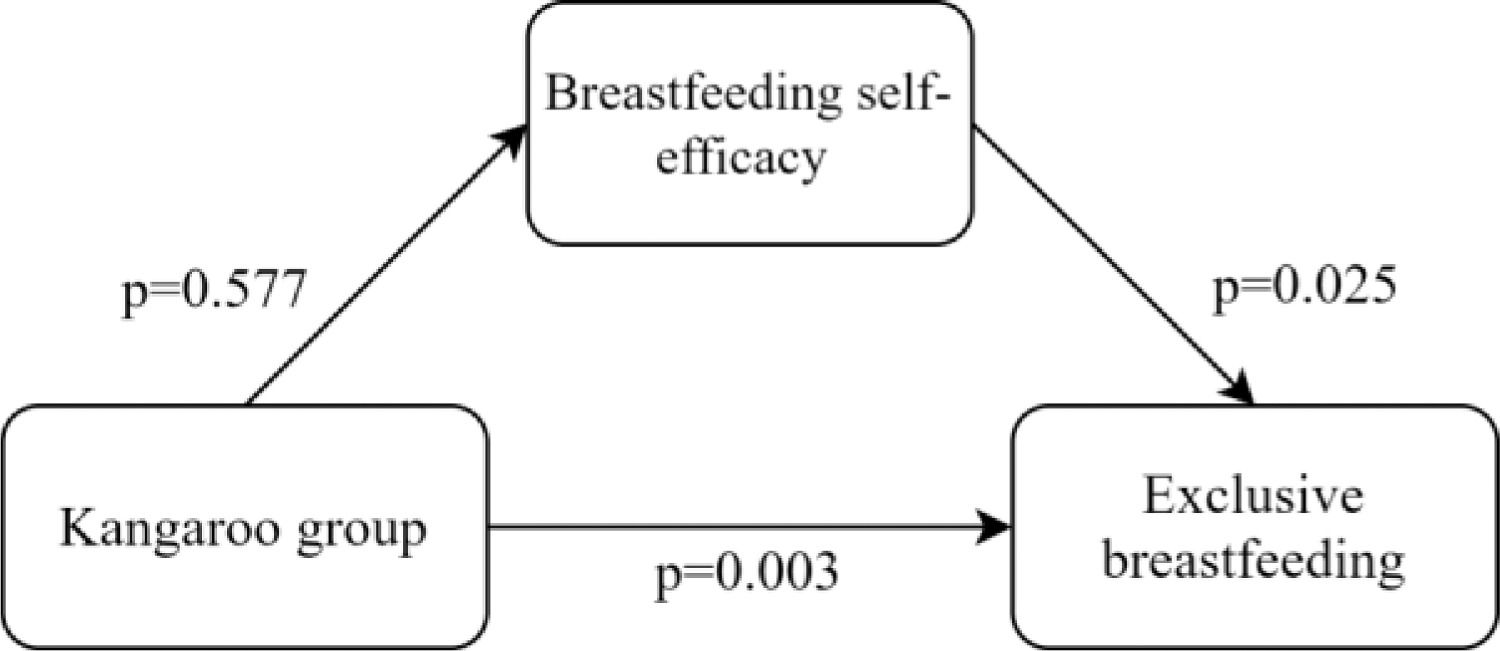
ResultsThe kangaroo group had a higher rate of exclusive breastfeeding at hospital discharge (p = 0.000). There was a positive association between having remained in the kangaroo (p = 0.003) and the breastfeeding self-efficacy score (p = 0.025) with the rate of exclusive breastfeeding at hospital discharge. Breastfeeding self-efficacy did not act as a mediator.
ConclusionThe self-efficacy of breastfeeding and the stay of the low birth weight newborn baby in the kangaroo unit acted positively and independently in exclusive breastfeeding, and the self-efficacy of breastfeeding did not act as a mediator in this association.
Premature or low birth weight can delay the establishment of breastfeeding, as well as demand hospital practices that are harmful to its maintenance, one of which is the separation of the woman from her newborn child.1–3 In this sense, psychosocial factors such as the mother's motivation and belief in breastfeeding are determinants for her to overcome the challenges inherent in lactation and breastfeeding.1,2,4
Breastfeeding self-efficacy has been identified as a protective factor against early weaning.5–9 Its concept encompasses women's ability and confidence to successfully breastfeed,5,6 directly related to their skills and knowledge, being subject to modification through health interventions.5–9
A biopsychosocial intervention strategy is the Kangaroo Method, a care model aimed at the qualification and humanization of care for low birth weight newborn babies and their families.10 In Brazil, this practice began in 1992, evolving with rapid expansion, which contributed to the launch, in 2000, of the Standard for Humanized Care for Low Birth Weight Newborn Babies, instituting the “Kangaroo Method” as a national health policy.10,11
Developed in three stages, this method aims to strengthen the family bond, encourage breastfeeding and promote safe hospital discharge with the mother able to develop the care of her child and recognize the alarm signals,10 being an alternative to conventional care.10–15 The first stage begins with the identification of high-risk prenatal care and extends to the reception of the low birth weight newborn babies and their families in the Neonatal Intensive Care Unit (NICU) or Conventional Neonatal Intermediate Care Unit (CNICU).10
The second stage consists of the continuity of care for the low birth weight newborn baby in a hospital unit called Kangaroo Neonatal Intermediate Care Unit (KNICU), which contains a structure capable of receiving the mother-child dyad,10 and stands out for the continuous presence of the mother, where the kangaroo position should be performed for as long as possible.10,11 Finally, the third stage consists of outpatient follow-up with its own schedule and guarantee of care at the original institution until the low birth weight newborn baby reaches 2500 g.10
It is known that the Kangaroo Method as a public health policy has been gaining more space in Brazilian neonatal units due to the various health benefits of the mother-child dyad, with emphasis on the increase in exclusive breastfeeding (EBF) rates.10–13 In the international scenario, skin-to-skin contact stands out specifically.10–15 The self-efficacy of breastfeeding, in turn, has also been shown to be a protective factor against the early discontinuation of EBF.5–9 Therefore, it is necessary to understand the possible mediating role of maternal self-efficacy in breastfeeding in the relationship between the Kangaroo Method and the practice of EBF. Thus, the present study sought to assess the mediating role of breastfeeding self-efficacy in the association between KNICU and EBF.
MethodsStudy designA cross-sectional study nested in a cohort carried out from September 2018 to March 2020 in the Neonatal Unit of a Brazilian university hospital, which has 42 inpatient beds, 20 beds for the NICU, 16 for the CNICU, and six for the KNICU.
ParticipantsThe reference population consisted of all newborns weighing 1800 g or less who were born at the university hospital where the study was conducted. The low birth weight newborn babies were initially admitted to the NICU, and later the determination of their destination unit was routinely carried out according to the criteria established by the Ministry of Health. Eligibility criteria for the second stage of the Kangaroo Method, i.e., stay at the KNICU, are clinical stability of the newborn baby, full enteral nutrition, and a minimum weight of 1250 g. In addition to the mother's wish and availability, family support for her hospital stay, and consensus between the health team and family members.10
The following was considered as inclusion criteria the absence of severe congenital malformation; perinatal asphyxia16; genetic syndrome; symptomatic congenital infection; severe metabolic disease, and twinning. Concerning the mother, it was considered the absence of diagnosis of psychiatric illnesses or serious illnesses; drug addiction; deprivation of liberty; the impossibility of communication; maternal refusal, and any condition that made breastfeeding impossible.
141 low birth weight newborn babies were included, of which 27 were excluded due to neonatal (14) and maternal (2) death, diagnosis of alteration in the Central Nervous System (5) during the period of data collection, maternal refusal after inclusion (4) and loss of data that happened at the beginning of the collection (2).
The sample was calculated from the average of the total number of low-birth-weight newborn babies born at the hospital in the period from 2013 to 2017 (mean = 153), considering a 95% confidence level, a standard deviation of 10.96 and a margin of error of 2.5. Based on these criteria, the minimum final sample was 87 dyads.
Data collection instruments and procedureThe survey form consisted of maternal sociodemographic data (age, education and marital status); economic data (maternal work and family income); obstetric data (prenatal care, type of delivery, parity, and history of a low birth weight child). Data on the clinical evolution of the low birth weight newborn baby, such as birth weight, gestational age, Score for Neonatal Acute Physiology - Perinatal Extension (SNAPPE II), weight and corrected gestational age at hospital discharge, EBF rate, and length of stay were obtained directly from the electronic and physical records requested by the institutional archive sector.
SNAPPE II consists of a severity and mortality risk score with nine evaluation items, and higher scores correspond to the greater severity and risk of mortality.17 For data collection regarding EBF at hospital discharge, the medical evolution preceding this time point was considered.
Before hospital discharge, mothers answered the Breastfeeding Self Efficacy Scale - Short-Form (BSES-SF), a scale that comprises the mother's perception of her ability to breastfeed. The scale was translated and validated in Brazil with a Cronbach's Alpha of 0.74, indicating that this is a valid instrument to measure the confidence of Brazilian nursing mothers in this context.6 BSES-SF consists of 14 items, organized into two domains, technical and intrapersonal thoughts. Scores ranging from one (strongly disagree) to five (strongly agree) are assigned, with a minimum score of 14 and a maximum of 70 points. It is considered as low self-efficacy of breastfeeding scores from 14 to 32, moderate from 33 to 51, and high from 52 to 70 points.
Statistical analysisData were tabulated in electronic spreadsheets, processed, and analyzed using the Windows R software (version 4.4.1). The significance level adopted was 5% for all analyses. Quantitative data were described as mean, median, and standard deviation, whereas qualitative data were described as absolute and relative frequencies. The comparison of sample characterization variables was performed using Student's t-test and chi-square test.
The Mann-Whitney test was used to compare the breastfeeding self-efficacy score between the KNICU and CNICU groups. To compare the EBF rate between the groups, Fisher's exact test was used. To verify the mediating effect of breastfeeding self-efficacy on the association between KNICU and EBF, the structural equation model adjusted for the variables birth weight, length of hospital stay, maternal education, and history of low birth weight children was used.
Ethical aspectsMothers were approached during the first week of their children's hospitalization and invited to participate in the research, and they were asked to sign the Informed Consent Form. The research was submitted to the Human Research Ethics Committee and approved in March 2018 through Opinion Letter No. 2521,553.
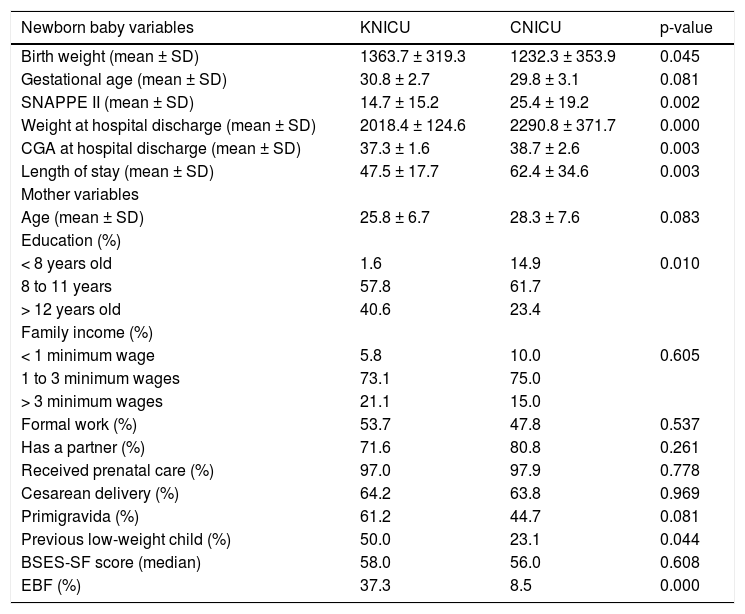
ResultsA total of 114 low birth weight newborn babies were included, 67 of which were hospitalized at KNICU and 47 at CNICU. The clinical characteristics of the low birth weight newborn babies, sociodemographic, economic, and maternal health data, the breastfeeding self-efficacy score, and the EBF rate per group are described in Table 1. It is possible to observe that the low birth weight newborn babies in the CNICU group had lower birth weight (p = 0.045), higher SNAPPE II score (p = 0.002), and longer hospital stay (p = 0.003). The low birth weight newborn babies in the KNICU group had lower weight (p = 0.000) and corrected gestational age (p = 0.003) at hospital discharge. When analyzing the variables related to mothers, the KNICU group had higher education (p = 0.010) and a higher percentage of low birth weight children in a previous pregnancy (p = 0.044). When comparing EBF rates at hospital discharge, a higher EBF percentage (p = 0.000) was observed for the dyads of the KNICU group (Table 1).
Characterization of low birth weight newborn babies, sociodemographic, economic, and maternal health data, breastfeeding self-efficacy score and exclusive breastfeeding rate by group.
KNICU, Kangaroo Neonatal Intermediate Care Unit; CNICU, Conventional Neonatal Intermediate Care Unit; SNAPPE II, Score for Neonatal Acute Physiology - Perinatal Extension; CGA, Corrected gestational age; BSES-SF, Breastfeeding Self Efficacy Scale – Short Form; EBF, Exclusive breastfeeding. Analysis: ' 'Student's t-test. Chi-square test. Mann Whitney Test. Fisher's exact test.
The results of the possible mediating role of breastfeeding self-efficacy in the association between KNICU and EBF at the time of hospital discharge are shown in Figure 1. Through the structural equation model, a positive association was observed between having remained at the KNICU and the EBF rate (p = 0.003) at hospital discharge; and between the breastfeeding self-efficacy score and the EBF rate (p = 0.025). However, breastfeeding self-efficacy did not act as a mediator between the stay at the KNICU and EBF (p = 0.577).
DiscussionIn the context of prematurity and the Kangaroo Method, the authors observed that both KNICU and breastfeeding self-efficacy had a positive association with EBF at hospital discharge, but there was no mediating effect of self-efficacy in the association between KNICU and EBF. Thus, newborn babies who remained at the KNICU during hospitalization were more likely to be discharged from the hospital in EBF. In addition, mothers with high self-efficacy scores for breastfeeding, regardless of the hospitalization unit, also had greater chances of exclusively breastfeeding their children at the time of their hospital discharge.
Breastfeeding self-efficacy has been identified as a protective factor against early weaning,5–9 establishment and maintenance of EBF in the short and long term.18 The theory of breastfeeding self-efficacy infers that the act of breastfeeding is directly influenced by the women's personal experience, observation of other women's experiences, verbal persuasion of close and influential people, and emotional responses.5,6 In this sense, being confident in relation to her condition as a nursing mother is a positive aspect.6
The perception of self-efficacy can determine how the individual thinks, feels and behaves in a given situation, indicating the time and effort that will be used to achieve the desired result.5,6 In addition, since it is a construct related to health promotion behaviors, it is subject to change through interventions.5–9 Behavior in relation to breastfeeding in the immediate postpartum period, for example, is predictive of behavior four to eight weeks later.7
The establishment and continuity of EBF for mother and low birth weight newborn baby dyads are permeated by difficulties and challenges,19–22 but there are factors that can favor its maintenance, such as the daily stay of the mother with her child, a possibility offered by the KNICU. The continuous presence of the mother and skin-to-skin contact can promote benefits such as reduced neonatal mortality,23 clinical stability, weight gain, and early hospital discharge,11 in addition, this longer time with the child favors breastfeeding.11–13
It was possible to observe in the results of the present study that the permanence of the low birth weight newborn baby in the KNICU favored EBF, regardless of the mothers feeling confident to breastfeed. It is known that the Kangaroo Method is a support and incentive policy for breastfeeding, and EBF is one of its components. This care model aims at the qualification and humanization of neonatal care, bringing together biopsychosocial intervention strategies favorable to the active participation of the family from admission to the Neonatal Unit until hospital discharge.10 The implementation of the KNICU and skin-to-skin contact have been identified as a means of favoring the increase in EBF rates at the time of hospital discharge and in the outpatient follow-up.11–13
It is necessary to emphasize that family-centered care,24 the support of healthcare professionals,20,25 the confidence and commitment of women to breastfeeding 20–22 programs and policies with the objective of protecting, promoting, and supporting breastfeeding 2,10 have also been identified as important for increasing EBF rates regardless of the inpatient unit. Additionally, the welcoming and free access of parents to the neonatal unit and the work of the team also ensured that the family is a modulator of the newborn baby's well-being.10,25 Thus, these care practices should be encouraged even if the hospital institution does not have beds for KNICU.
The authors highlight as positive points of this study the evaluation of a public health policy and the analysis of mediation to understand direct and indirect relationships among the inpatient unit, maternal self-efficacy, and EBF. The authors also highlight the profile of the population assessed since the study was carried out with a vulnerable group consisting of newborn babies with birth weight less than or equal to 1800 g and who needed assistance in the NICU. As a consequence of the limitations of this study, the authors can mention the non-randomization of the sample since, for ethical reasons, women cannot be prevented from participating in the second stage of the Kangaroo Method. In addition, it is possible that there were mother-child dyads that met the eligibility criteria, but there were no vacancies available at KNICU.
The self-efficacy of breastfeeding and the permanence of the low birth weight newborn baby in the KNICU acted positively and independently in EBF. Initiatives such as the Kangaroo Method are important for the promotion of EBF in this public since this care model is based on the humanization of care and the continuous presence of the mother. In addition, breastfeeding self-efficacy measured by the BSES-SF is an assessment tool for maternal perception and confidence that can be used by the multidisciplinary team at the bedside, being an alternative for planning interventions since higher scores are related to higher rates of EBF. Prospective studies that assess this possible mediating relationship are important to seek ways to encourage breastfeeding and promote increased EBF rates in low birth weight newborn babies.
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES) – Finance Code 001.