In this brief review, the authors focus on the effects of gestational exposures to urban air pollution on fetal development and neonatal outcomes.
Source of dataIn this review the authors used PubMed, Web of Science and SciELO research platforms, analyzing papers from the last 30 years.
Summary of the findingsEpidemiological and experimental evidence agree that gestational exposure to air pollution in urban increases the risks for low birth weight, preterm birth, congenital malformation, intrauterine growth restriction, and neonatal mortality. Furthermore, exposures are associated with increased risks for preeclampsia, hypertension, gestational diabetes.
ConclusionsTherefore, it is time for greater involvement and engagement of the health sector in the discussion of public policies that may affect the quality of the environment, and that directly or indirectly impact the health of those who were not yet born.
The first evidence of the relationship between exposure to environmental pollution and reproductive effects were derived from observational studies of unintentionally exposed wildlife.1 The reproductive process is subject to toxic effects from a variety of substances present in the environment, particularly anthropogenic contaminants, including agrochemicals, traffic-derived air pollutants, and industrial wastes.2
In the last 3 decades, numerous studies have been published showing that environmental air pollutants that the authors have contact with in daily life affect reproductive health and, in particular, produce adverse effects on fertility, pregnancy outcomes, fetal health, and development.3-5
In addition to immediately observable gestational outcomes, such as low birth weight, IUGR, neonatal mortality, the authors must not forget that any perturbation that occurs during an intrauterine period of life is determinant not only for fetal development but also can predispose individuals to later life diseases.6
From their early stages of development, still in the womb, children are one of the most sensitive groups to air pollution. Children breathe more air per kilogram of body weight, they spend more time in outdoor activities significantly increasing their exposure dose. Moreover, as they have a longer life expectancy, they would have more time to develop health problems resulting from exposures that occurred earlier.
According to the World Health Organization (WHO), 1.7 million children under the age of 5 have died worldwide from diseases and conditions related to the environment, including air pollution, non-drinking water, poor sanitation, and hygiene or exposure to toxic chemicals. Air pollution (AP), a widespread environmental contaminant and causes approximately 600 000 deaths in children under 5 years annually and increases the risk for respiratory infections, asthma, and adverse neonatal conditions.7
Science and health authorities have been warning for a long time about the harmful effects that air pollution can have on people's health, and the impacts can range from minor transient irritation to the eyes and throat, breathing difficulties to death from cardiorespiratory problems and lung cancer. The outcome will depend on some factors, the authors highlight the two most important: age and exposure dose. And despite the development of cleaner technologies in the energetic and transport sector, the problem of air pollution seems to be far from solved.
In this brief review, the authors focus on the effects of gestational exposures to urban air pollution on fetal development and neonatal outcomes.
Urban air pollutionUrban air pollution, which is derived largely from combustion processes of fossil fuels (vehicle emissions), is a mixture containing many toxic components which include carbon monoxide (CO), nitrogen dioxide (NO2), Sulphur dioxide (SO2), ozone (O3), lead (Pb), polycyclic aromatic hydrocarbons (PAH) and particulate matter (PM). Particulate matter is a complex mixture of microscopic particles and liquid droplets composed of nitrates, sulfates, organic substances (e.g. polycyclic aromatic hydrocarbons), metals (e.g. cadmium, Pb), and dust particles.8 Particles are classified according to their size in PM10 and PM2.5, which means that these particles have diameters of 10 and 2.5 micrometers, respectively. If the authors compare the size of PM2.5 to a grain of sand or to an erythrocyte, they are 40 times and 3 times bigger than PM2.5, respectively.9
Among the main pollutants mentioned above, particulate matter is the most harmful to health due to its small size and its characteristic of adsorbing other toxic agents on its surface. These particles can translocate almost all physiological barriers (e.g. alveolar-capillary barrier, blood-brain barriers, dermal barrier, maternal-fetal interface.10-13
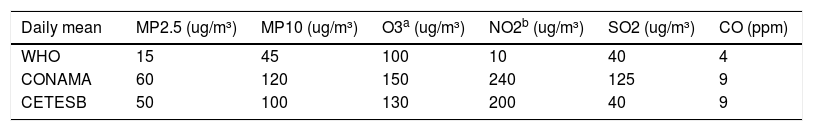
Air quality is determined by the concentration of criteria pollutants that are measured daily. There are defined limits for each pollutant and the acceptable values vary depending on the environmental authority that has defined them. These levels are determined by the health risks associated with them and by public health relevance. WHO has an air quality guideline that recommends levels for 6 pollutants – PM₁₀, PM 2.5, O₃, NO₂, SO₂, and CO.8 In Brazil, standard limits are defined by the National Environment Council of Brazil (CONAMA)14 and Sao Paulo State has its local standard,15 which is very similar to those established by the CONAMA. It is important to note that the study's tstandard is less stringent than the WHO's posing greater risks to the population's health.9Table 1 depicts the current mean 24hs limits for the criteria pollutants defined by WHO, CONAMA and Environmental Company of the State of São Paulo (CETESB).
Limits of the daily mean concentration of criteria pollutants according to the air quality guidelines from WHO, CONAMA (national standards, Brazil), and CETESB (São Paulo State, Brazil).
Respiratory and cardiovascular diseases are the most commonly observed and studied effects associated with exposure to air pollution followed by neoplasia. However, in the last two decades, lesser-known effects have been linked to chronic exposures to air pollution including adverse reproductive outcomes, neurodegenerative diseases and metabolic disorders.16
Special attention has been given to gestational exposures since these early exposures can predispose to other negative outcomes later in adult life, such as cardiovascular disease, stroke, chronic respiratory disease, diabetes and cancer.
The earliest published evidence of negative health effects on children was published in the 1970s and showed an association between exposure to industrial air pollution and infant mortality.17,18 However, it was only in the 1990s that new studies were published evaluating this issue in more detail and with a greater focus on prenatal exposures.
Studies conducted in Europe, Asia, and the Americas agree that expectant mothers exposed to environmental levels of air pollution are at greater risk of having the development of their pregnancy compromised and maternal and fetal health could be affected. However, it is not clear until now whether the effects are due to a specific pollutant or to the interactions of different pollutants and nor if pre-gestational exposure could aggravate the effects.
The main effects observed in epidemiological studies as a result of gestational exposure to pollution are low birth weight (LBW), intrauterine growth restriction (IUGR), prematurity, congenital malformations, and neonatal mortality.19,20
Meta-analysis results estimated that for every 10 μg/m3 increase in PM2.5 birth weight is reduced from −15.9 to −23.4 g. When analyzed, which trimesters are determinant for these effects, results are different, however, the critical windows of susceptibility seem to be the last third trimester.21-24 Greater risks for preterm birth seems also to be related to exposure in the 3rd trimester, DeFranco et al.25 found a 19% increased risk of PTB.
Intrauterine and neonatal mortality and preterm birth4,26 are outcomes less frequently associated with gestational exposure to air pollution.
More recently, new effects associated with gestational exposure were evidenced, such as preeclampsia,22,27 hypertension and gestational diabetes,28-30 placental abruption,31 premature rupture of membranes,32 placenta praevia, and accrete.33
A meta-analysis conducted by Pedersen et al.34 have shown that maternal exposure to 5 μg/m3 increments in ambient PM2.5 is associated with a 50% increased odds of pregnancy-induced hypertension and preeclampsia.
Fetal developmental disruptions may occur indirectly (maternally mediated), as a result of direct effects on the fetus, or can be a consequence of the combination of both. In most cases, embryo/fetal toxicity occurs via maternal exposure to toxic agents but the authors must keep in mind that male exposure to contaminants may be teratogenic or impair gestation if the chromosomes of the spermatozoa are damaged.35 There is also evidence of paternally mediated effects of air pollution on the risk of adverse health outcomes in offspring. However, the effects of the father's exposure on the health of his offspring are beyond the scope of this review.36-38
Low birth weight is a predominant effect associated with exposure to ambient air pollution. Birth weight is an important indicator of subsequent health issues; low-birth-weight babies are more prone to develop hypertension, coronary heart disease, and non-insulin-dependent diabetes during adulthood.39 Jedrychowski et al.40 observed that not only birth weight is affected, changes in other anthropometric measurements can be observed, such as reduction in head circumference. Studies conducted by van den Hoove et al.41 using ultrasound measurements observed that fetal growth is compromised by maternal exposure to air pollution. In this study, NO2 levels were inversely associated with fetal femur length in the second and third trimester, and PM10 and NO2 levels both were associated with smaller fetal head circumference in the third trimester.
Baïz et al.,42 found that maternal exposure to ambient urban levels of NO2 and PM10 during the whole pregnancy was a strong predictor of low vitamin D status in newborns. In other studies, it was observed that maternal exposure during pregnancy affects the distribution of NK, T lymphocytes in and IgE content of umbilical blood.43,44 The consequences of gestational exposure on lung development and childhood pulmonary function have also been reported.45
Different studies point out that diverse congenital deformities could be associated with maternal exposure to air pollutants. A recent meta-analysis was conducted for several combinations of air pollutants and congenital defects and reported that NO2 and PM2.5 were associated with the risk of pulmonary valve stenosis with OR = 1.74 and OR = 1.42 respectively. The risk of developing tetralogy of Fallot (TOF) was observed to be associated with PM2.5 with OR = 1.52. SO2 exposure was related to a high risk of the ventricular septal defect (VSD) with OR = 1.15 and orofacial defects (OR = 1.27).46
Despite the adoption of different study designs and statistical evaluations, and the presence of confounding variables (e.g. maternal smoking, gestational age, and socioeconomic factors), most of these investigations suggest that the reported associations are causal. Studies conducted using animal models give support to the epidemiological findings.5
MechanismsThere are many proposed mechanisms to explain how the noxious substances present in air pollution might interfere adversely in gestation.
Kannan et al.47 suggest a number of plausible biological mechanisms by which particulate matter would influence the development of pregnancy increases the risks of negative outcomes such as low birth weight. They proposed that exposure would increase oxidative stress and trigger systemic maternal inflammation, increase blood pressure, and impairments in endothelial function which negatively impact placental nutrient and oxygen transport functions.
Among the pollutants present in the complex mixture (CO, SO2, NOx, MP, O3, PAH) that constitute air pollution, it is only known how CO exerts its effects on the fetus. The mechanisms by which other pollutants influence fetal development remain unclear. It is possible that DNA damage, as well as the activation of P450 enzymes, endocrine alterations are involved, compromising placental function. The present study's research group has pioneered the experimental investigation of the impacts of exposure to particulate matter on placental and fetal development. Using exposure chambers receiving ambient air from a region of intense vehicular traffic in the city of São Paulo and filtered air, the authors showed that morpho-functional alterations of the placenta are really involved in the impairment of fetal development assessed by birth weight.48,49 Furthermore, exposure during pregnancy to PM2.5 lowers placental concentrations of the angiogenic factors VEGF and FLK-1 (receptors for a vascular endothelial growth factor (VEGF).50
UncertaintiesAll of the published reviews acknowledged that there are many uncertainties on the association between gestational exposure to air pollution and negative outcomes, such as limited information on personal exposures and difficulties in linking particulate matter (PM) composition or single component to the effects and to control confounding factors Undoubtedly these aspects point out that there is still a need of further toxicological and clinical studies.
Even though, these findings are important to serve as a guide for further studies and to generate questions that need to be answered:
- -
Which trimester of pregnancy is more relevant to the impairment of fetal development?
- -
Which component of the PM presents a higher risk for reduced birth weight and other outcomes?
- -
Could multigenerational exposure to ambient PM concentration present cumulative effects?
There must also increase de number of studies on the effects of air pollution generated by wildfires and agricultural fires, as in recent years the authors have seen numerous events of large proportions that certainly impacted the health of pregnant women, newborns, and children.
Conclusion and future directionsIn urban areas, exposure to air pollution is unavoidable. If the authors consider that half of the global population lives in urban areas, most of these areas have moderate to high levels of air pollution, prenatal exposure to air pollution increases the risk for LBW and IUGR, and that these outcomes are related to greater risks for hypertension, diabetes and metabolic disorders later in life, the impact of air pollution on the health status of the next generations will be of great concern. Therefore, it is time for greater involvement and engagement of the health sector in the discussion of public policies that may affect the quality of the environment and directly or indirectly negatively impact the health of those who were not yet born.