To discuss the associations between habits and environment in childhood and cardiovascular effects on adults.
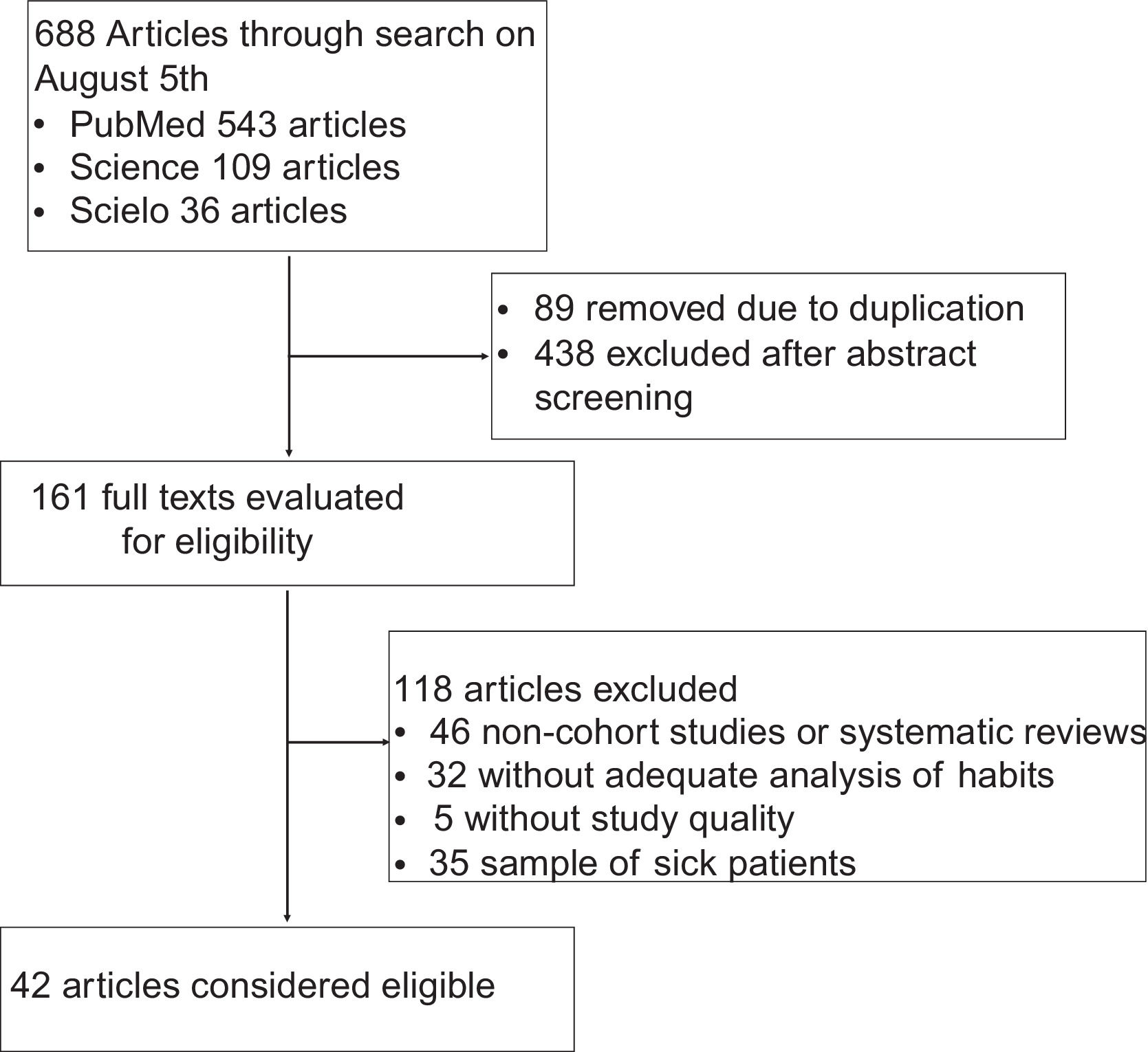
Source of dataSearch in PubMed, Scielo and Science databases, cohort or case-control studies, and systematic or scope-based reviewson the causal relationship among exposures in the pediatric age group and cardiovascular effects in adults.
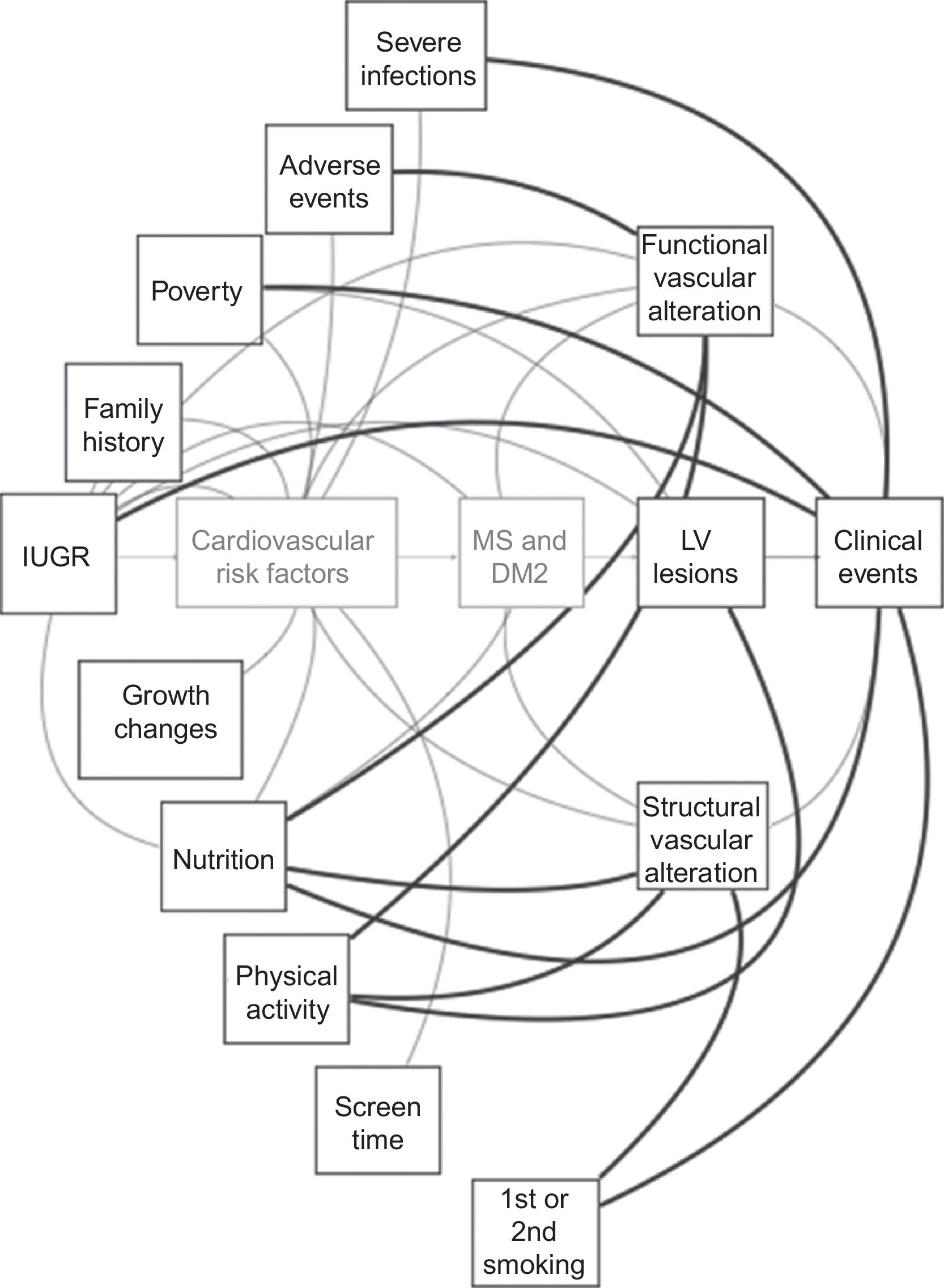
Synthesis of dataThe authors identified 41 eligible articles, which demonstrated an impact on cardiovascular health (characterized as surrogate events - structural or functional vascular alterations or left ventricular dysfunction - or clinical events - myocardial infarction, stroke or cardiovascular death) with environmental aspects (intrauterine or economically poor environment, violence, reduced life expectancy and serious infections) and habits (nutrition, physical activity and tobacco exposure). In addition to the direct and independent associations between exposures and outcomes, several traditional cardiovascular risk factors (CVRF) or family histories are also intermediate pathophysiological pathways in the described phenomena.
ConclusionsThere are direct relationships between lifestyle and inadequate environments in childhood and cardiovascular effects, although the observed associations showed divergences in terms of results and interpretation. In spite of these, it is recommended to encourage healthy lifestyles and protection against childhood adverse exposures, as habit formation occurs at this age, and its relationship with CVRF since childhood has already been well established. On the other hand, the format and intensity of the stimulus must respect the social, cultural and psychological aspects of each population, aiming to obtain the best and most lasting result without generating harmful consequences for the individuals.
In non-pandemic times, cardiovascular diseases (CVD) are the main causes of death in the world: around 350,000 Brazilians die from acute myocardial infarction (AMI) per year, as well as approximately 100,000 from a stroke.1 Atherosclerosis, a systemic, inflammatory, and progressive disease that affects the entire vascular bed, starts in the fetal period, manifesting itself clinically most often in the 5th and 6th decades of life. Despite efforts to prevent and control cardiovascular risk factors (CVRF) and their complications in adulthood worldwide, there are still significant residual morbidity and mortality percentages, which are believed to be at least partially related to the effect of these risk factors in the pediatric age group.2
Therefore, cardiovascular prevention should be considered a priority in the pediatric age group. The promotion of a healthy lifestyle seems to be the most important measure at this age, as it is most often the etiology or aggravating factor of CVRF. Moreover, it is at this age that life habits are formed, and the promotion of these habits is easier than pursuing habit changes at older ages.3
And what habits or environmental factors, present in childhood, represent independent risk factors for atherosclerotic events, such as AMI, stroke or cardiovascular death?
The aim of this study is to discuss the associations between habits and the environment in childhood or adolescence and cardiovascular effects in adults.
Materials and methodsThis is an integrative review on the relationship among lifestyle or environmental aspects of children and adolescents and their cardiovascular impact on adulthood.
Eligibility criteriaClinical trials,cohort or case-control studies, as well as systematic or scope reviews were selected, which determined the causal relationship among life habits or adverse exposures in children under 18 and major cardiovascular outcomes - AMI, stroke, or cardiovascular death - or surrogate outcomes, namely: left ventricular alterations - left ventricular hypertrophy (LVHT) or left ventricular diastolic dysfunction (LVDD) -, structural vascular alterations - carotid intimal-medial thickness (cIMT), atheromatous plaques or coronary calcium score (CCS) - and functional vascular alterations - arterial stiffness (AS), pulse wave velocity (PWV) or flow-mediated dilation (FMD) were considered eligible.
Literature search and data extractionEligible studies were identified in the PubMed, Science and Scielo databases, using the following Boolean combinations:
- •
((childhood OR child) AND (habits OR diet OR tobacco OR alcohol OR physical activity)) AND ((adult OR adulthood) AND (atherosclerosis OR cardiovascular events OR myocardial infarction OR stroke))
- •
((criança) AND (estilo de vida)) AND ((doença cardiovascular) OR (infarto do miocárdio) OR (acidente vascular cerebral))
Based on this premise, 42 articles were considered eligible, according to the procedure described in Figure 1.
ResultsBased on the literature search, it was identified that, in addition to traditionally known habits, other conditions also have significant and independent associations with CVD in adult life, and factors that interfere in the entire cycle of child formation, since the fetal period, may be involved.
Intrauterine environmentBased on the observation of children who were born in historical periods of the great famine (such as in World War II due to the German siege of the Netherlands and the forced Chinese urbanization policy of the “Great Leap Forward”), it was evident that, from an unfavorable intrauterine environment, there is an epigenetic adaptation to an energy-sparing phenotype, called intrauterine programming. This programming tends to be maintained throughout the life cycle, with serious consequences for cardiovascular health.4,5
Regarding cardiovascular consequences, two systematic reviews showed that there is yet no consensus on the topic. On the other hand, numerically, there are more data that sustain this association than the opposite, and there are not enough data yet to carry out meta-analyses.6,7 Despite this, the Chinese 4C Study cohort (77,925 participants born between 1959 and 1962), showed that food deprivation in the fetal period, when compared to unexposed fetuses, increases the risk of diabetes mellitus in adulthood by 17% (CI: 1.05-1.31), but the presence of overweight or obesity in these individuals is necessary for this association to manifest.4 The China Health and Retirement Longitudinal Study (2,383 participants) demonstrated that, after controlling for gender, the severity of deprivation, smoking, alcohol consumption, and body composition, exposed fetuses were 41% more likely (95%CI: 1.06-1.88) to develop hyperuricemia and metabolic syndrome in adulthood than unexposed fetuses.8 The study also described a relationship with abdominal obesity, stronger in women, as well as a tendency towards hyperglycemia and hypertension.5 The Australian Longitudinal Cohort (MUSP Study), with 1,780 participants, demonstrated that other perinatal disorders, such as pre-gestational obesity and hypertensive disease of pregnancy, are also related to hypertension in adulthood.9
On the other hand, a recent systematic review found a relationship between low birth weight and AS. The authors believe that for each lower standard deviation of the birth weight, the risk of cardiovascular disease increases between 1.11 and 1.43.6
Socioeconomic aspects, violence and other adverse eventsAlthough the fetal and early childhood periods are considered the most critical for the metabolic modulation related to the previously described sparing and pro-inflammatory profile, several conditions in childhood and adolescence, such as poverty and different types of violence, have also shown profound and permanent alterations in the late cardiovascular risk.
Growth and development in poverty environmentsThe systematic review that evaluated 35 studies on the effect of poverty on child development showed that poverty determines an association of undesirable characteristics: 1) high physical and psychological stress; 2) high exposure to toxic substances; 3) low access to health care; 4) low access to healthy food choices; and 5) low access to safe places to practice physical activities. When these socio-ecological conditions occur in an associated and chronic manner, there is a biological and behavioral adaptation that predisposes a defense phenotype - neuroendocrine changes that regulate body stress, behavior, sexual development, and the immune system. This response leads to the possibility of greater defense, with the development of a pro-inflammatory profile and acceleration of sexual maturation.10
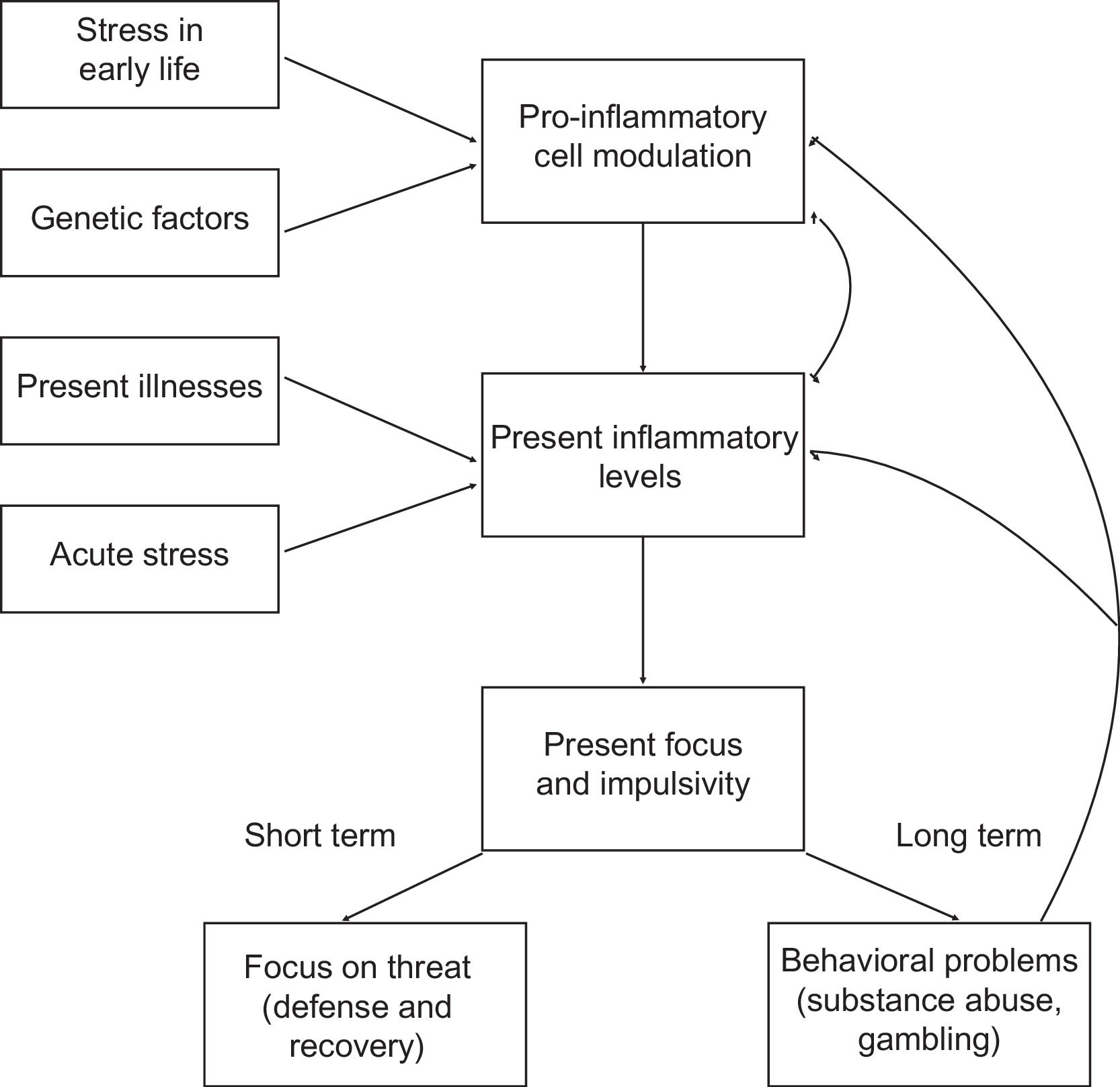
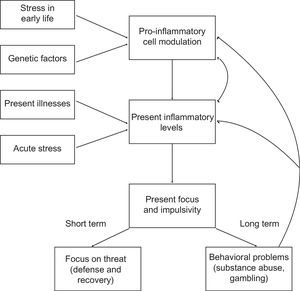
This programming of the immune system is associated with a tendency towards pro-inflammatory states, with high activation of pro-inflammatory cytokine pathways and high monocytic activity, which induces chronic inflammation. This association - exposure to an unfavorable environment in childhood and pro-inflammatory tendency in adults - is maintained even when other pro-inflammatory factors in adult life, such as obesity, hypertension, and dyslipidemia, are controlled. This is more evident when the injury occurred in early childhood, during the immune system maturation. This pro-inflammatory state seems to have other effects, such as increased impulsivity for immediate rewards and, consequently, an increase in behaviors such as tobacco use, alcohol abuse, binge eating, and illicit drug use. These behaviors, in turn, closing the vicious circle, feed the pro-inflammatory state (Figure 2).10
The pro-inflammatory state tends to perpetuate itself, demonstrating the difficulty of leaving this vicious circle for children born in an unfavorable environment.
Chronic hunger in childhood also increases the risk of a sparing somatic phenotype, characterized by short stature, slower metabolism, and less active behavior. Moreover, in adults who suffered from hunger in childhood, there is a tendency to increase food intake without the presence of hunger, due to loss of homeostasis in the hunger-satiety regulation; they are, therefore, people at high risk of developing obesity in adulthood.10
One of the most important studies on the association of the role of pediatric aspects in cardiovascular risk is the Finnish The Cardiovascular Risk in Young Finns Study (CRY Finns Study). The authors followed more than 2,000 children from birth in 1980 to the present day. In this study, a direct relationship was demonstrated between having been raised in a poor neighborhood and worse habits (lower intake of fruits and vegetables and less physical activity in the preschool period, as well as a higher frequency of tobacco use in adolescence), resulting in a greater chance of obesity (OR: 1.44; 95%CI: 1.01-2.06), arterial hypertension (OR: 1.83; 95%CI: 1.14-2.93) and diabetes mellitus (OR: 3.71; 95%CI: 1.77-7.75) in adulthood.11
The same cohort demonstrates that worse socioeconomic conditions in childhood increase the risk of hepatic steatosis (OR: 1.42, 95%CI: 1.18-1.7), even when controlling for age, gender and risk for steatosis in childhood (body mass index - BMI, high insulin and low birth weight). The explanation seems to be related to same physiological and behavioral adaptations, which at the same time determine a greater chance of survival under risk conditions, and worse long-term metabolic patterns.12
As for cardiovascular consequences in adulthood, poverty during childhood is associated with worse LVDD, accessed on echocardiography by the ratio of E/e' waves (difference of 0.2; 95%CI 0-0.5 for the lowest tertile versus highest income tertile), as well as greater left ventricular mass (difference of 1.5; 95%CI:0.2-2.8 when comparing the lower tertile versus the upper tertile), even when adjusted for age, gender and traditional CVRF in childhood and adulthood.13
Two German case-control studies analyzed the risk of stroke in adults who had been exposed to poverty and its complications in childhood. The first showed that this chance is 77% higher in exposed individuals (95%CI: 1.2-2.6) than in non-exposed ones, regardless of the parents' profession, living conditions or family income.14 The other study demonstrated that unfavorable conditions caused high risk of smoking, alcohol abuse and sedentary lifestyle, factors that, when controlled, had less impact on this association.15 According to another meta-analysis, poverty is associated with a higher incidence of CVD (RR of 1.3 to 1.8) including AMI, stroke and CV mortality.6
Traumatic childhood experiencesA scope review of childhood traumatic experiences and cardiovascular risk demonstrates a proinflammatory state similar to that caused by an unfavorable intrauterine environment or poverty, with increased risk of obesity, smaller chromosome telomere size, and increased cortisol levels in adults.16 The Mexican Teacher's Cohort, with 9,853 female participants, demonstrated that when exposed to adverse childhood experiences, they are more likely to become smokers (RR: 1.58; 95%CI: 1.37-1.81) sedentary (RR: 0.83; 95%CI: 0.69-0.99), develop diabetes mellitus (RR: 1.49; 95%CI: 1.13-1.96), dyslipidemia (RR: 1.49; 95%CI: 1 .26-1.75) and obesity (RR: 1.37, 95%CI: 1.19-1.57) when compared to unexposed ones.17
The British Birth Cohort, which has followed nearly 9,000 participants since 1958, has found different associations with late cardiovascular effects when considering exposure to childhood neglect or abuse. An association was found between neglect and abdominal obesity, hypertriglyceridemia and low levels of HDL-cholesterol. For physical violence, an association was found with high concentrations of LDL-C and glycated hemoglobin (HbA1c).18 Among the CV consequences of this exposure, adults can develop AS, regardless of the influence of gender, systolic blood pressure, obesity, or physical activity.19
Severe infectionsA Dutch case-control study with 153 pairs showed an association between severe infections in early childhood and early AMI (before 55 years of age), with an odds ratio of 2.67 (95%CI: 1.47-4.83), even when adjusted for traditional FRCV, lifestyle, diet, economic class, and family history. This study also found a direct relationship with the Framingham risk score (p = 0.052).20
Survival expectancy and mental healthIn addition to habits, a Korean case-control study, the National Longitudinal Study of Adolescent and Adult Health demonstrated that the expected survival of adolescents, as well as juvenile delinquent behavior, can have an impact on habits, such as healthy eating, alcohol and tobacco use, behaviors that are usually perpetuated into adulthood.21 These characteristics are associated with high values in the Framingham risk score for cardiovascular risk in 30 years.22
LifestyleChildhood eating habitsThe UK Multi-ethnic Determinants of Adolescent Social Well-being and Health Cohort (DASH Cohort) study followed 665 participants observed that eating habits in childhood and adolescence impact the adult body composition and lipid profile, as well as the presence of obesity in childhood increases the risk of hypertension, HbA1c high levels, and low HDL in adulthood.23
This same cohort demonstrated that skipping breakfast regularly during childhood and adolescence increases BMI and total cholesterol in adulthood,24 which was corroborated by the Childhood Determinants of Adult Health Study (CDAH Study), an Australian cohort, which showed an effect on waist circumference (+4.6cm; 95%CI: 1.7-7.5), on insulin concentrations (+2.0 mU/L; 95%CI: 0.7-3.3), on total cholesterol levels (+0.4 mmol/L; 95%CI: 0.1-0.7) and in LDL-cholesterol levels (+0.4 mmol/L; 95%CI 0.2-0.6).25
The International Childhood Cardiovascular Cohort Consortium (i3C), which integrates the Bogalusa Heart Study, the CDAH Study and The CRY Finns Study showed that high income children show a higher intake of healthy foods than low income ones, due to better economic conditions and greater access to information. This fact reinforces the explanatory power of the association between economic class in childhood and cardiovascular disease in adulthood, highlighting the importance of a better quality of dietary pattern during growth and development. Especially in women, eating healthy foods in childhood (high ingestion of fruits and vegetables and low ingestion of saturated fat) decrease the risk of high concentrations of TC, LDL-cholesterol, apolipoprotein B, and C-reactive protein.25 This same study showed that fiber intake from fruits or vegetables in childhood maintained a direct and independent relationship with a decrease in BMI in adulthood. This effect was independently maintained even in the presence of low serum concentrations of total cholesterol and triglycerides, decreased insulin resistance and reduced systolic arterial hypertension.26
As for the cardiovascular consequences, the systematic review on the role of fiber intake in childhood in the cardiovascular health of adults demonstrated that eating fruits and vegetables in childhood determines a lower PWV in adults, even when several CVRF are controlled, or even irrespective of the intake of fruits and vegetables in adulthood. Eating fruit in childhood also had an inverse relationship with cIMT in adulthood, and this relationship is maintained even when controlled for any other CVRF in adults, regardless of gender.27 Men who were fed with breast milk had higher FMD than those who were not.26 Finally, another systematic review showed that there is a relationship between a diet high in total saturated fat and AS, as well as the ingestion of milk and dairy products in childhood can reduce the risk of stroke.6
There are few clinical trials on the relationship between lifestyle and cardiovascular health in adults. Maybe the biggest one is the Special Turku Coronary Risk Factor Intervention Project (STRIP), started in 1990 and also based in Finland, which has already studied more than 1,000 children. In this study, children are followed from birth to age 20, with an annual counseling on nutrition and physical activity, with the investigation of CVRF, as well as several markers of subclinical atherosclerosis. This study demonstrated that the promotion of a healthy diet since infancy (decreased intake of saturated fatty acids and increased monounsaturated and polyunsaturated fatty acids, increased fiber and decreased sugar intake) leads to an improved quality of LDL-cholesterol and HDL-cholesterol subclasses in adults, as well as levels of VLDL-cholesterol, IDL-cholesterol, HOMA-IR, glucose, insulin, LDL-cholesterol, non-HDL-cholesterol, and lower apolipoprotein B/Apolipoprotein A1 ratio (p ≤ 0.003). The impact on hypertension, on the other hand, was more modest.28,29
Physical activity in childhoodIt is during childhood that the habit of being physically active is formed. The CRY Finns Study showed that the fact of staying active throughout life results in a protection against obesity (RR: 0.76; 95%CI: 0.59-0.98), abdominal obesity (RR: 0.82; 95%CI: 0.69-0.98) and hypertriglyceridemia (RR: 0.6; 95%CI: 0.47-0.75).30 The China Health and Nutrition 2009 Survey (9,000 participants) reinforces this idea, as it also showed that inactivity in childhood is associated with a high risk of developing an unfavorable metabolic profile in adulthood. When associated, in childhood, with general and abdominal obesity, the risk is especially high of developing glucose intolerance, diabetes mellitus, and dyslipidemia.31
The European Youth Heart Study, a multicentric cohort with 332 individuals, demonstrated that, for every one standard deviation of isometric muscle strength at 12 years of age, there is a proportional decrease in BMI (-0.6 kg/m2; 95%CI: -0.98 to -0.22), triglycerides (-0.09 mmol/L; 95%CI: -0.16 to -0.02) and diastolic blood pressure (-1.22 mmHg; 95%CI: -2.15 to -0.29) in adulthood.32
As for cardiovascular consequences, physical inactivity and obesity in childhood can also determine, regardless of adult blood pressure levels, worse LVDD (p < 0.001).33 Moderate to vigorous physical activity is associated, on the other hand, with lower AS and cIMT values.6
Screen timeDespite the established relationship between screen time and obesity - or even signs of vascular dysfunction - in childhood, there are little data on the influence of screen time during childhood on cardiovascular risk in adulthood. This may occur because the phenomenon of excess screen time during childhood is still recent in Human History. An American cohort, The SEARCH for Diabetes in Youth Study, demonstrated that, even in adolescence, chronic control of screen time decreases HbA1c plasma concentrations.34
Tobacco useA Swiss cohort, the SAPALDIA Young Study, demonstrated that tobacco use in adolescence is associated with subclinical atherosclerosis in young individuals, with an increase of approximately 3 micrometers in the CIMT/smoked cigarette/day of the week, even when controlled for familial confounding factors, such as secondhand smoke. Apparently, there are different impacts of tobacco use of children and adolescents on the cardiovascular risk of adults. In the situation of active smoking, there is a strong association with cIMT and CV events, such as AMI and stroke; in scondhand smoking, there is an association with cIMT and the presence of atherosclerotic plaque.35
CVRF in the mediation between childhood lifestyle and cardiovascular risk in adulthoodAlthough there is a less evidence of a direct and independent association between childhood habits and cardiovascular risk in adults, the relationship among lifestyle, CVRF and their late consequences is well established.
Family historyThe influence of genetic inheritance on cardiovascular risk is well established, especially among patients affected early in life by cardiovascular events. There is also robust evidence of the influence of genetics on CVRF and its tendency to remain at the same percentile throughout the life cycle, a phenomenon known as the tracking. However, the relationship between habits of parents and children is also important, which can significantly influence cardiovascular risk in the long term. A German study, which analyzed data from 832 families, showed that the high-calorie diet has a predictable behavior in different family members: between mothers and daughters, the odds ratio is 7.5; between mothers and sons, 3; and between parents and sons, 2.8.36
ObesityA meta-analysis on the association between childhood obesity and cardiovascular risk showed that childhood obesity seems to be associated with SAH, triglyceride and HDL-cholesterol serum concentrations, insulin resistance, and diabetes mellitus, but this effect is attenuated when controlled for the BMI of adults. Uric acid levels in adults, however, seem to have a strong and independent association with childhood obesity and rapid weight gain in childhood.37 Uric acid, therefore, seems to be more related to the obesity tracking phenomenon (tendency to remain obese during childhood and adulthood) than with childhood obesity alone.38
In fact, despite the existence of an association between unhealthy lifestyle and obesity, data from more than 300,000 people from the British Biobank show that obesity has a polygenic inheritance, which also impacts the association between childhood and adult obesity: individuals that carry certain genetic polymorphisms may have up to 25x more odds of developing severe obesity than non-carriers.39
The two CVRF during childhood that has the greatest impact on the occurrence of subclinical atherosclerosis in adulthood are dyslipidemia and obesity, in that order of importance. The Bogalusa study demonstrated, during the follow-up of 486 participants for up to 37 years, that being obese in childhood increases the cIMT in adults by 25%.40 Another scope review reinforced this thesis, being even stronger when obesity is present in adolescence. The association between childhood obesity and LVHT, in turn, is an independetrisk for cardiovascular events.40
In a meta-analysis on the association between obesity and risk of cardiovascular events, for each standard deviation of BMI, the risk of stroke increases by 1.15 to 1.29, and the risk of AMI by 1.09 to 1.21.41 Each increase of one BMI unit between 7 and 17 years of age is associated with a 1.05 increase in the relative risk of coronary heart disease in adulthood.42 According to the Harvard Growth Study, a retrospective cohort of 508 participants, being obese in adolescence increases their risk of death from coronary heart disease up to 50 years later. Obesity in adolescence increases the risk of death from any cause by approximately 80%, and the risk of death from cardiovascular causes by approximately 130%.43
Weight changes in childhoodA French retrospective cohort (1495 participants) demonstrated that another important childhood predictor for the association with adult cardiovascular risk is the early adiposity rebound, that is, at what age the lowest BMI between 2 and 10 years old is observed, due to the greater fat accumulation than by increasing lean mass that occurs at this age. This precocity is related to greater general and abdominal obesity, in addition to the occurrence of metabolic syndrome in adults, regardless of gender (p < 0.001). In women, it is associated with hypertriglyceridemia (p < 0.001), LDL-cholesterol serum concentrations (p < 0.001), systolic (p = 0.02), and diastolic (p = 0.04) blood pressure. Another study described the relationship between having overweight/obese parents and early adiposity rebound, which suggests the association between genetics and habits in this phenomenon.44
Arterial hypertension in childhoodHypertension is perhaps the cardiovascular risk factor that determines earlier cardiac consequences: LVHT and LVDD have been described as early as in the second decade of life, especially in children with severe and chronic hypertension. Even in the apparently healthy general population, an association has been described between SAH in childhood and AS, increased cIMT, increased CCS, and LVHT in adults. For each standard deviation of blood pressure, the risk of AMI increases by 1.05 to 1.15 in the long term.6
DyslipidemiaLDL-cholesterol levels constitute the biggest impact factor in atherosclerosis. In patients with very high levels, such as in familial hypercholesterolemia, an accelerated progression of atherosclerosis is already detected, sometimes in the second decade of life. The association between high LDL-cholesterol serum concentrations and increased cIMT, as well as CCS, has been described, even in cohorts of apparently healthy children, without the presence of risk genetic polymorphisms. The association between childhood hypertriglyceridemia and CV events in adults has also been described.6
Metabolic syndrome and diabetes mellitusMetabolic syndrome (MS), an association of several CVRF such as obesity, abdominal obesity, arterial hypertension, hypertriglyceridemia, and low HDL-cholesterol serum concentrations, induces a pro-inflammatory state in which, in adults, shows an already clear association with atherosclerosis and related events. In childhood, the i3C consortium defends the acceptance of its characterization, even in younger children. The prevalence of type 2 diabetes mellitus (DM2) has increased in adolescence and should be investigated in every adolescent with obesity. There is a direct and independent association between MS and DM2 in adolescence and stroke in adults.6,45
DiscussionThis review described the variables related to lifestyle and inadequate environments that surround children and adolescents and that can influence cardiovascular health in adults, as graphically described in Figure 3. The relationship between obesity, hypertension, dyslipidemia and hyperglycemia in childhood, and cardiovascular risk in adults is quite consistent.
There is evidence that intrauterine injuries or childhood exposure to high-risk environments can profoundly and permanently impact the metabolic pathways that, while on the one hand determine a protective phenotype against this unfavorable environment, on the other hand, increase the chance of cardiovascular complications in adulthood. Among the mechanisms that explain this relationship is the emergence of high-risk CVRF, such as obesity, dyslipidemia, hypertension, and the consequent pro-inflammatory state. These factors act both through direct mechanisms, promoting the acceleration of atherosclerotic disease, the common basis for CD, and through their interaction, as a result of a synergistic pathological progression that increases the velocity of disease onset.
This review, on the other hand, showed that there are scarce prospective studies on lifestyles in childhood and adolescence, such as diet, physical activity, sedentary activities, and tobacco use to affirm, with a high degree of evidence, that there is a direct and independent relationship between childhood lifestyle and adult cardiovascular risk.
With the analysis of data available in the literature so far, it is already possible to recommend, however, some cardiovascular prevention strategies. They are: seeking a healthy lifestyle and the protection of health against health problems since the gestational period, as avoiding unhealthy exposures during intrauterine life and reducing physical and emotional risk environments in childhood can modulate structural metabolic pathways that seem to perpetuate themselves throughout the life cycle.
Considering that life habits are formed in childhood and that the maintenance of healthy patterns in adult life predisposes to lower cardiovascular risk, the stimuli should be established early on, on a large scale, involving government guidelines for education and regulatory standards of the food industry. In parallel, it is important to establish, since childhood, the continuous monitoring of cardiovascular risk through the investigation of dietary habits, physical activity, smoking, obesity, dyslipidemia, and arterial hypertension, factors that act directly or multiply the risk of cardiovascular complications and which tend to perpetuate themselves throughout the life cycle.
Finally, we must emphasize that health professionals are dealing with children who develop habits in environments that are created and maintained by parents, teachers, and caregivers, so that the use of negative adjectives, such as inadequate, undesirable, unhealthy, or harmful, can carry derogatory messages, possibly generating negative feelings and demanding too much from the children. This is about not blaming the victims, also taking into account that it is necessary to observe possibilities of individual pathogenic modes of function, even in healthy habits and environments. Thus, embracement seems to be the best strategy, with understanding, positive reinforcement and stimuli, adapting the format and intensity of actions, aiming to respect the social, cultural, and psychological aspects of each child in their family and social system of relationships. Thus, it will be possible to obtain better and longer-lasting results, reducing trauma and harmful mortifications from care interventions, which can also have permanent consequences for the individual and their health in adulthood.
FundingBruno Caramelli is a researcher and 1C research productivity fellow at CNPq, process #309454/2020-4. Nelson Filice de Barros is a researcher and 1D research productivity fellow at CNPq, process #308452/2019-4.