Reference values for lung function tests differ in samples from different countries, including values for preschoolers. The main objective of this study was to derive reference values in this population.
MethodsA prospective study was conducted through a questionnaire applied to 425 preschool children aged 3 to 6 years, from schools and day-care centers in a metropolitan city in Brazil. Children were selected by simple random sampling from the aforementioned schools. Peak expiratory flow (PEF), forced vital capacity (FVC), forced expiratory volumes (FEV1, FEV0.50), forced expiratory flow (FEF25-75) and FEV1/FVC, FEV0.5/FVC and FEF25-75/FVC ratios were evaluated.
ResultsOf the 425 children enrolled, 321 (75.6%) underwent the tests. Of these, 135 (42.0%) showed acceptable results with full expiratory curves and thus were included in the regression analysis to define the reference values. Height and gender significantly influenced FVC valuesthrough linear and logarithmic regression analysis. In males, R2 increased with the logarithmic model for FVC and FEV1, but the linear model was retained for its simplicity. The lower limits were calculated by measuring the fifth percentile residues.
ConclusionFull expiratory curves are more difficult to obtain in preschoolers. In addition to height, gender also influences the measures of FVC and FEV1. Reference values were defined for spirometry in preschool children in this population, which are applicable to similar populations.
: Valores de referência para testes de função pulmonar diferem em amostras de diferentes países, incluindo valores para pré-escolares. O objetivo principal do presente estudo foi derivar valores de referência em nossa população.
Métodos: Foi realizado estudo prospectivo, com aplicação de questionário a 425 crianças pré-escolares com idade variando entre três e seis anos, provenientes de escolas e creches públicas e privadas de uma cidade metropolitana do Brasil. As crianças foram selecionadas por amostragem aleatória simples dos referidos educandários. Foram avaliados: PFE, CVF, VEF1, VEF0,50, FEF25-75 e as relações: VEF1/CVF, VEF0,5/CVF e FEF25-75/CVF.
Resultados: Das 425 crianças recrutadas, 321 (75,6%) realizaram os testes. Destas, 135 (42,0%) apresentaram manobras aceitáveis, com curvas expiratórias completas e fizeram parte da análise de regressão para definir os valores de referência. Por análise de regressão linear e logarítmica, a estatura e o sexo influenciaram significativamente nas medidas de CVF. No sexo masculino, o r2 se elevou com o modelo logarítmico, para a CVF e VEF1, porém o modelo linear foi mantido, por sua simplicidade. Os limites inferiores foram calculados através das medidas do 5° percentil dos resíduos.
Conclusão: Curvas expiratórias completas são de mais difícil obtenção em pré-escolares. Além da estatura, o sexo também influencia nas medidas de CVF e VEF1. Foram definidos valores de referência para espirometria em crianças pré-escolares, nessa população, aplicáveis a populações semelhantes.
Several studies have verified that preschool children can adequately perform spirometry tests.1–6 They have been the basis for spirometry assessment in preschool children in an important document of the American Thoracic Society (ATS) and European Respiratory Society (ERS),7 and some of these studies have defined reference values for spirometry in this age range.1–4 Recent studies have added to these assessments.8,9 In 2001, the first study that defined reference values (RV) in 184 white preschool children was published.1 Subsequently, several authors began to establish RV in other populations,2–4,10–16 and a comparison of data from some of these studies showed agreement among them.1–3,13,15,16 Others observed the inappropriateness of applying equations of a given population to another, dissimilar one, and recommended that RV should be defined for each population with similar characteristics.4,12
The expiratory maneuver in children at this age range can last less than one second. Reference values for forced expiratory volume in the first 0.5 s or after 0.75 s from the start of forced expiration have been described.10,12–14
Regarding schoolchildren, there are RV values available in Brazil for children older than six years (Mallozi),17 but RV values are not available for the age range of 3 to 6 years.
Thus, the aim of this study was to derive reference values for spirometry in preschool children in a Brazilian population sample.
Material and methodA prospective study was conducted from February of 2005 to December of 2006, through a questionnaire applied to 425 preschool children, aged 3 to 6 years, from schools and day-care centers in the city of Recife, Brazil. Children were selected by simple random sampling at the aforementioned institutions. All children whose parents or guardians adequately answered the questionnaire participated in this study. Initially, the sample size consisted of 315 children, of which 240 underwent testing and were part of a recent publication assessing the acceptability and reproducibility of spirometry in preschoolers.8
Subsequently, 110 additional children were included in the study to complete a number of tests with full expiration, necessary for the calculation of RV, totaling 425 children. Only children considered free of respiratory disease were selected for the tests, as defined by the questionnaire recommended by the Epidemiology Standardization Project, ATS-DLD-78-C, adapted and validated for use in Brazil.18 Children with reported birth weight<2.500g and gestational age<37 weeks, respiratory distress at birth, history of use of oxygen for more than 24hours, prior experience in performing spirometry, or with reported current or prior heart disease that needed or had indication for medication or surgery were also excluded.
The study was approved by the Research Ethics Committee of the Centro de Ciências da Saúde of Universidade Federal de Pernambuco (UFPE), Brazil. An informed consent was obtained from parents or guardians.
MethodsAll children were weighed and measured before each test session; both were performed in duplicate, and the means were calculated. Weight was measured using an electronic Filizola scale (Filizola – São Paulo, Brazil), previously calibrated by the manufacturer. The children were measured and weighed without shoes or socks. For height measurement, a WCS-112-Cardiomed stadiometer (Cardiomed – São Paulo, Brazil) was used, with the platform supported on firm and level ground, with the children standing, without shoes or socks, according to the standard technique.19
Three spirometers from the same manufacturer (WinDX™ Spirometry System, software v.1000.64 net; Creative Biomedics International, Inc. – Irvine, California, USA), were used for the tests, which were performed by the same technician, the main author of this study. For calibration, two syringes from the same manufacturer were used, both with three liters. The aforementioned equipment meets the instrument standards recommended by the ATS.19 In this spirometer, the expiratory flow is measured using a pneumotachograph, and the volume is derived from digital integration of the flow. Results are corrected for body condition, body temperature, ambient pressure, saturated with water vapor, and BTPS. A filter was attached to the spirometer (Creative Biomedics, Inc. – San Clement, CA, USA) and to that, a disposable mouthpiece 2.5cm in diameter – P/Esp. SX/PC.
The following parameters were assessed: peak expiratory flow (PEF), forced vital capacity (FVC), forced expiratory volumes (FEV1, FEV0.50), forced expiratory flow (FEF25-75), as well as FEV1/FVC; FEV0.5/FVC and FEF25-75/FVC ratios. Forced expiratory volume in 0.75 of the first second of FVC (FEV0.75) could not be assessed, as it was not part of the spirometer program used. Calibration was performed at the examination site before each series of five tests and standardized according to the manufacturer's instructions.
The flow-volume curves were monitored by direct visualization on the computer screen during each test. A computed animation program with visual stimuli, which was already included in the spirometer, was used to better encourage the children. With these encouragements, the children were stimulated to perform the tests as if they were a playing a game; only seven children (2%) refused to perform it. This program consists of several incentive screens, but only two were used: one with a picture of a birthday cake with candles that go out after blowing at them, and another with the image of a circus with a column that becomes colored after being blown at.
Test sessions were suspended after a mean of 12 attempts to achieve acceptable maneuvers, or earlier if the child showed fatigue or disinterest in continuing the test. Each test session, including the instruction time, had a maximum duration of 20minutes, so there would be subsequent feasibility for its application in clinical practice. The curves were recorded for subsequent analysis.
Each child was individually instructed at the time of the examination, asked to place the disposable cartridge in the mouth, and had it well adjusted, to prevent leaks. The nasal passage was occluded by a nose clip; for the smaller children, the occlusion was performed by the technician using his fingers, as the clip was not adequate for these children. Children were instructed to breathe in tidal volume and then were asked to fill their lungs as much as possible, then to blow as strong, fast, and long as possible. The tests were performed with the children in the standing position for their convenience, as they were better adjusted to the spirometer mouthpiece. The tests were analyzed by two authors of this study.
The highest values of FVC and FEV1 were obtained from three best flow-volume curves, not necessarily from the same curve. The FEF25-75 values were obtained from the curve with the highest sum of FVC and FEV1 or FEV0.5, according to the forced expiratory time (FET). The values of FEV0.5 were obtained from the curves with higher values of FEV1 or FEV0.5, when the FET was ≤ 1s.
The adopted acceptability criteria were those standardized by the ATS/ERS - update 2005 with full expiratory curves.20 Thus, curves with end-expiratory point ≥ 10% PEF were excluded, as recommended by the ATS/ERS, update 2007.7 Curves were accepted with FET ≥ 0.5, as well as tests with two or more acceptable curves.
Curves were considered unacceptable when, in addition to not meeting the current eligibility criteria, they had peak flow showing no evidence of effort, or were flat, round, had more than one peak or peak shifted to the right; FET<0.5 s; or had inspiratory pause (hesitation) before the forced expiration.
Statistical analysisRegarding the statistical analysis, the formula used to calculate the sample size was: N>50+8m, where m is the number of variables.21 Taking into account equations separated by gender, and considering that height would be the dependent variable, 50+8 individuals of each gender should be included. The sample size calculation was based on the height entry only, according to the studies by Nystad and Zapletal.2,3
The individual correlations among lung function parameters (PEF, FVC, FEV1, FEV0.5, FEF25-75, FEV1/FVC, FEF25-75/FVC and FEV0.5/FVC ratios) and the independent variables (height, weight, age) were evaluated. Independent variables with a correlation and p<0.10 were entered into multivariate regression equations, separated by gender.
ResultsOf the initial 425 children, 104 (24.4%) were excluded, 81 (19%) due to asthma diagnosis and 23 (5.4%) due to several other causes – preterm birth, low birth weight, heart disease, and refusal to be assessed. In the 321 children (75.6%) who underwent the test, age distribution was: 57 (17.7%) aged 3 years, 118 (36.7%) aged 4 years, 129 (40.1%) aged 5 years, and 17 (5.26%) aged 6 years. Of all children who underwent the tests, only 135 (42.0%) achieved full expiratory curves, according to the ATS/ERS recommendations, update 2005.18 Their distribution by age group were: eight (6.0%) at 3 years, 29 (21.4%) at 4 years, 74 (54,8,4%) at 5 years, and nine (6.6%) at 6 years of age. Despite the most recent document directed to preschool considers acceptable partial curves up to 10% of PEF,7 the authors chose to consider the stricter standards of the previous publication,20 as the study aim was to define RV.
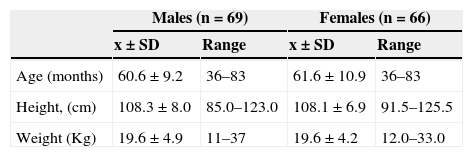
Anthropometric data are shown in Table 1. Regarding ethnicity, there were 66 (48.8%) white children, and 69 (51.2%) mixed-race children, which included 39 (28.8%) black children. Due to the high levels of mixed-race in Brazil, the black ethnicity was not assessed separately.
Anthropometric values of preschoolers submitted to complete acceptable expiratory curves.
| Males (n=69) | Females (n=66) | |||
|---|---|---|---|---|
| x±SD | Range | x±SD | Range | |
| Age (months) | 60.6±9.2 | 36–83 | 61.6±10.9 | 36–83 |
| Height, (cm) | 108.3±8.0 | 85.0–123.0 | 108.1±6.9 | 91.5–125.5 |
| Weight (Kg) | 19.6±4.9 | 11–37 | 19.6±4.2 | 12.0–33.0 |
SD, standard deviation.
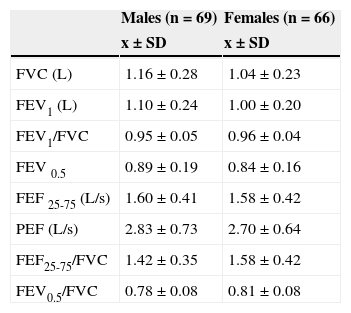
The assessment of acceptability and reproducibility of this study is detailed in another article by the same authors, recently published.8 The mean and standard deviation of spirometric parameters evaluated are shown in Table 2.
Spirometric values of the children who performed acceptable curves with full exhalation.
| Males (n=69) | Females (n=66) | |
|---|---|---|
| x±SD | x±SD | |
| FVC (L) | 1.16±0.28 | 1.04±0.23 |
| FEV1 (L) | 1.10±0.24 | 1.00±0.20 |
| FEV1/FVC | 0.95±0.05 | 0.96±0.04 |
| FEV 0.5 | 0.89±0.19 | 0.84±0.16 |
| FEF 25-75 (L/s) | 1.60±0.41 | 1.58±0.42 |
| PEF (L/s) | 2.83±0.73 | 2.70±0.64 |
| FEF25-75/FVC | 1.42±0.35 | 1.58±0.42 |
| FEV0.5/FVC | 0.78±0.08 | 0.81±0.08 |
FEF, forced expiratory flow; FEV, forced expiratory volume; FVC, forced vital capacity; PEF, peak expiratory flow; SD, standard deviation.
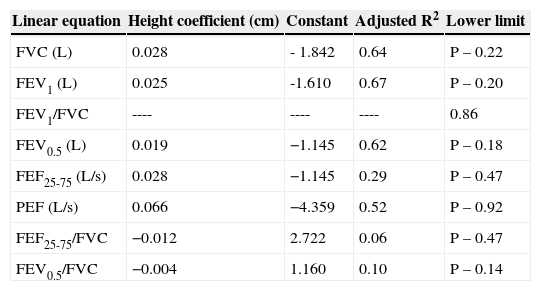
A linear and logarithmic regression analysis was performed, separated by gender (males, n=69; females, n=66), with height as the predictive variable. Next, the linear and logarithmic models were compared, and no difference was observed for FVC and FEV1 in females; in males, however, the R2 increased with the logarithmic model for FVC (0.64 to 0.70) and for FEV1 (0.67 to 0.73). Preference was given to the linear model, due to its simplicity. Predicted values were then calculated, separated by gender. The regression equations, also separated by gender, are shown in Tables 3 and 4.
Regression equations, coefficient of determination (R2), and lower limits for spirometric variables in the male reference population.
| Linear equation | Height coefficient (cm) | Constant | Adjusted R2 | Lower limit |
|---|---|---|---|---|
| FVC (L) | 0.028 | - 1.842 | 0.64 | P – 0.22 |
| FEV1 (L) | 0.025 | -1.610 | 0.67 | P – 0.20 |
| FEV1/FVC | ---- | ---- | ---- | 0.86 |
| FEV0.5 (L) | 0.019 | −1.145 | 0.62 | P – 0.18 |
| FEF25-75 (L/s) | 0.028 | −1.145 | 0.29 | P – 0.47 |
| PEF (L/s) | 0.066 | −4.359 | 0.52 | P – 0.92 |
| FEF25-75/FVC | −0.012 | 2.722 | 0.06 | P – 0.47 |
| FEV0.5/FVC | −0.004 | 1.160 | 0.10 | P – 0.14 |
Linear Equations: Height x coefficient+weight x coefficient - constant (as weight had no influence on the calculations, its coefficient was not be considered).
Lower limit=Predicted (P) - fifth percentile of the residual or fifth percentile found.
FEF, forced expiratory flow; FEV, forced expiratory volume; FVC, forced vital capacity; PEF, peak expiratory flow; SD, standard deviation.
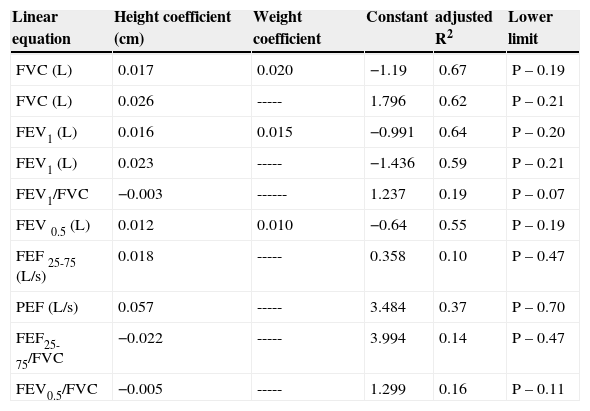
Regression equations, coefficient of determination (R2), and lower limits for spirometric variables in the female reference population.
| Linear equation | Height coefficient (cm) | Weight coefficient | Constant | adjusted R2 | Lower limit |
|---|---|---|---|---|---|
| FVC (L) | 0.017 | 0.020 | −1.19 | 0.67 | P – 0.19 |
| FVC (L) | 0.026 | ----- | 1.796 | 0.62 | P – 0.21 |
| FEV1 (L) | 0.016 | 0.015 | −0.991 | 0.64 | P – 0.20 |
| FEV1 (L) | 0.023 | ----- | −1.436 | 0.59 | P – 0.21 |
| FEV1/FVC | −0.003 | ------ | 1.237 | 0.19 | P – 0.07 |
| FEV 0.5 (L) | 0.012 | 0.010 | −0.64 | 0.55 | P – 0.19 |
| FEF 25-75 (L/s) | 0.018 | ----- | 0.358 | 0.10 | P – 0.47 |
| PEF (L/s) | 0.057 | ----- | 3.484 | 0.37 | P – 0.70 |
| FEF25-75/FVC | −0.022 | ----- | 3.994 | 0.14 | P – 0.47 |
| FEV0.5/FVC | −0.005 | ----- | 1.299 | 0.16 | P – 0.11 |
Linear Equations: Height x coefficient+weight x coefficient - constant.
Lower limit=Predicted (P) - fifth percentile of the residual or fifth percentile found.
FEF, forced expiratory flow; FEV, forced expiratory volume; FVC, forced vital capacity; PEF, peak expiratory flow; SD, standard deviation.
In males, the weight did not influence the derived predicted values. It was observed that the FEV1/FVC ratio decreased with height, but the coefficient of determination was only 4%, demonstrating that it was better to have the lower limit fixed at 0.86, calculated by the fifth percentile, which facilitates interpretation. The correlation of FEF25-75/FVC ratio with height was significant, but low. The lower limit of the predicted value, 0.92, can be used for this correlation, based on the fifth percentile value found. The correlation of FEV0.5/FVC ratio with height was also significant, but low (R2=0.11, p=0.006). For the latter, the lower limit of the predicted value of 0.65 can be used, based on the fifth percentile value found.
In females, FVC and FEV1 were augmented with increasing weight, which did not occur in males. Table 4 shows that the calculation of predicted FVC and FEV1, when taking only height into account, results in lower adjusted R2.
The FEV1/FVC ratio in females also decreases with height; however, height explains only 19% of the variation. Thus, a constant lower limit could be used, calculated by the 5th percentile of the values found, which would be 88%. The correlations of FEF25-75 and FEF25-75/FVC ratio with height were significant, but low. The lower limit of the predicted value for both, 1.00, can be used based on the fifth percentile of the values found.
The correlation of VEF0.5/FVC with height was also significant (R2=0.06, p=0.046), but low. The lower limit of the predicted value, which is 0.67, can be used also based on the fifth percentile value found.
DiscussionIn the present study, reference values were derived for forced spirometry in preschool children from Recife, Northeastern Brazil, which are applicable to similar populations.
According to the sample calculation obtained, the sample size was sufficient for the study purpose. Only 42.0% of the preschoolers aged 3 to 6 years were able to perform acceptable maneuvers with full expiration, in agreement with the requirements of the ATS/ERS, update 2005.20 This percentage is similar to that found by Zapletal et al., of 40% acceptability at the age range of 3 to 5 years, accepting as a criterion for test conclusion only curves with full expiration.3 Studies with a high percentage of acceptability applied less stringent curve end criteria, with the inclusion of partial end-expiratory curves ≤ 10% of PEF.2,4,10,16 Other authors agreed to accept maneuvers with end-expiratory curves ≤ 25% of PEF.1,14 These studies derived reference equations for preschoolers considering valid measures of FVC obtained from partial expiration curves.
The large sample loss – 58% of the original sample – should not influence the results, considering that the sample size was increased to 2.8 times the initial sample calculation - from 116 to 321 children. The analysis performed with the database of a recently published study, to which the present study is a part of, showed that partial end-expiratory curves up to 10% of PEF, as recommended in a recent document of the ATS/ERS for preschoolers,7 are also valid for FVC values.8 However, no studies have tested the validity of early termination curves, such as ≤ 25% of PEF.
Thus, only curves with full or partial expiration up to the limit of ≤ 10% of PEF should be considered for the analysis, aiming to derive reference equations. However, for greater accuracy of the reference equation, this study has not considered partial curves as valid for this purpose.
Similar to most studies that evaluated RV for spirometry in preschoolers,1–4,10–16 in the present study height was also the best predictor of lung function. It was observed that in addition to height, gender also influences the measures of FVC and FEV1, although the contribution was only 4%. By including gender in the analysis, several authors found it showed a small influence.2,10,12,14–16 Nystad et al. reported that gender had a slight, but significant influence on FVC and FEV1 measures. The increase in the coefficient of determination (R2) when gender was included was<1%.2 In adults, this influence is 30%.22 The observation in the present study, of a 4% increase in R2 when adding gender to the analysis, can be explained by the high reproducibility and low variability of parameters. Other studies found no influence of gender.1,3
There was a agreement between the coefficient of determination (R2) of FVC, FEV1, and FEV0.5 with findings in several other important studies carried out in preschoolers.2,13–15
Regarding the regression model, there was significant difference between linear or logarithmic model use in this study, but only for males. Some authors have found a better correlation when using the logarithmic model.1,3,13 For simplification purposes, the use of the linear regression model is suggested in both genders, considering height as the dependent variable.2,12,15,16
Most previous studies that evaluated RV in preschoolers used z-score measures for these calculations.2,3,12,15,16 Stanojevic et al., in a review study on RV in preschool children, showed that there are differences in the interpretation of spirometry results when using percentage of predicted values or z-scores.11 As in the present study, Piccioni et al. also used measures of percentile of predicted values and lower limits.14
Comparing the predicted values calculated by the present study with the values found by other authors, for FEV1 preschoolers with mean height and weight values corresponding to those observed in this sample values were found of 1.10, 1.11, 1.08, 1.05 and 1.14, respectively for Burity, 2012; Kjaer, 2008; Nystad, 2002; Zapletal, 2003 and Pesant, 2007. For FEV1 in females, these values were 1.03, 1.06, 1.05, 1.04, and 1.18, respectively. It is observed that, except for the study by Pesant, the values are very similar. In the Pesant study, different statistical models were used to predict values in males and females, which resulted in the finding of much higher values of FEV1 for females.
The limitations of this study include the deficit in the spirometric program used, due to lack of millimetric markings on flow-volume curve charts, preventing the identification of maneuvers with early termination. Moreover, the lack of data on weight and height of normal Brazilian preschool children makes it difficult to compare the data on weight and height obtained in this study in order to define its applicability to the Brazilian population. The data on weight and height were consistent with those of the World Health Organization (WHO) for this age group, so this reference equation can be extrapolated to the Brazilian population. The great difficulty in obtaining full expiratory curves in this age group demonstrates the importance of assessing the FEV0.5 in preschoolers. As spirometry quantifies the degree of airway obstruction and aids in the diagnosis of respiratory disease,23 it is necessary that further studies define the usefulness of FEV0.5 in the evaluation of obstructive diseases, as well as its bronchodilator response cutoff, to be used in the diagnosis of respiratory symptomatic patients.
In conclusion, reference values were obtained from a sample of preschoolers in the Brazilian population. Height and gender were predictive variables for functional parameters. There was little difference between the linear or the logarithmic regression model in this age range.
FundingThis study received financial support from Fundação de Amparo à Ciência e Tecnologia de Pernambuco (Facepe) – Brazil.
Conflicts of interestThe authors declare no conflicts of interest.
To FACEPE, for the funding of this study. To the principals and teachers of the following schools: Escolas Iputinga, Manoel Antônio Freitas, Engenheiro Edinaldo Miranda, Maria Helena Lucena, Espaço Alegre, Dom Helder Câmara, Carochinha, Sítio do Berardo, Creches Menino Jesus and Vinde a Mim, as well as all others selected, for allowing the tests to be performed in their schools. To the parents and guardians, for giving consent for the participation of their children in this survey. To all students, for having the leading role in this research.
Please cite this article as: Burity EF, Pereira CA, Rizzo JA, Brito MC, Sarinho ES. Reference values for spirometry in preschool children. J Pediatr (Rio J). 2013;89:374–80.