Comprehend the profile and prevalence of non-suicidal self-injury (NSSI) in adolescents and its association with impulsiveness and loneliness.
MethodsCross-sectional study carried out in 2017 in Maceió-Alagoas, Northeast Brazil, in the households of 505 adolescents aged 12–17 years, using a sample stratified and randomized by gender and neighborhood. The following instruments were used: a sociodemographic questionnaire, Brazilian version of Functional Assessment of Self-Mutilation (FASM), the Brazilian Barratt Impulsiveness Scale (BIS-11), and the Brazilian Loneliness Scale (UCLA-BR).
ResultsA prevalence of 6.53% was found for non-suicidal self-injury disorder (DSM-5). Significant differences ( p ≤ 0.05) were observed regarding: the most frequently used forms of NSSI were the items “cut oneself” and “scratch oneself”; engaging in three or more different forms of self-injurious behavior (66.67%) and, reporting as reasons, “to relieve feelings of emptiness or indifference” and “to stop bad feelings/sensations.” Significance was also related to the sociodemographic profile: 72.73% were females and 63.54% had family income below one minimum wage. Individuals with self-injurious behavior also had higher impulsiveness and loneliness scores (p ≤ 0.05).
ConclusionsThe study identified a direct association between NSSI and impulsiveness and loneliness among adolescents, being more prevalent in females and in young individuals with socioeconomic vulnerability. The data provide support for improving public health policies, aimed at education, prevention, and treatment of adolescents with NSSI.
Non-suicidal self-injury (NSSI), according to the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5),1 in section III, noted as a “Condition for Further Studies,” is characterized by intentional self-inflicted injury to the body surface, on five or more days, with the expectation of leading to minor or moderate physical damage, without suicidal intent. Self-injury is intended to relieve negative feelings or cognition, to resolve an interpersonal difficulty, or to induce a state of positive feelings. This behavior is not socially approved and is not limited to picking at wounds or biting nails; with suffering or interference with interpersonal, academic, or other functions. It should also be noted that the behavior is not better explained by another mental disorder or medical condition.
Although NSSI is a relevant public health concern,2 with a greater risk in adolescence and young adulthood,3 not every adolescent with self-injurious behavior seeks professional help and, therefore, part of this information does not reach the knowledge of health systems.4
International estimates reported that prevalence rates of self-reported NSSI varied between 7% and 66%, depending on the adopted NSSI definition, the sample heterogeneity, and the employed assessment tools.5 In Europe,4 the prevalence was as follows: 21.4% in Turkey; 35.6% in Sweden; 25.6% in Germany; 23.6% in Italy, and 25.8% in the Netherlands. Other studies pointed to a prevalence of 21.9% in the United States6; 17.1% in Mexico7; 31.2% in India8; 29% in China9; and 48.7% in New Zealand.10 However, there is little research on NSSI in developing countries.11,12 In Chile,11 the prevalence of self-injurious behavior in adolescents with socioeconomic vulnerability was 23%. In Brazil, research carried out in the state of Minas Gerais13 identified a NSSI prevalence of 9.48% in adolescents. However, there is little research in Brazil with a community sample of adolescents.
Research findings14 have identified an association between impulsiveness and NSSI, associated with the behavior frequency, the number of methods used, and the condition severity. Moreover, an association was observed between loneliness and NSSI,6 in that higher levels of loneliness were associated with a higher probability of self-injurious behavior. However, few studies have assessed the association of NSSI with impulsiveness and loneliness.
Considering this context, the aim of the study was to assess the profile and prevalence of NSSI in adolescents and its association with impulsiveness and loneliness.
MethodsA cross-sectional study was carried out in 2017 in the participants’ households, with a sample stratified by gender and neighborhood, including all administrative regions of the city of Maceió, state of Alagoas, located in the Northeast region of Brazil. The sample consisted of adolescents aged 12–17 years old, the age group indicated in the literature4,7,8 for the onset of NSSI behavior. The methodological strategy of data collection in households allowed obtaining representative data about the population’s sociodemographic diversity, since it was possible to include individuals without access to the school environment.
The sample size dimensioning was performed using the Lee® Calculator, using the following as parameters: proportion in the population of 13%,14 absolute precision of 3, and a significance level of 5%. The calculated sample consisted of 483 adolescents, adding 5% to correct for eventual losses, totaling (n) 505 adolescents. During data analysis, two participants were excluded (one with a diagnosis of autism and one with psychotic disorder – self-declared in the sociodemographic questionnaire), in line with the differential diagnosis criteria proposed by DSM-5,1 from which a self-injurious behavior could arise from another mental disorder or medical condition.
The collection procedure involved the following: Stage one: selection of 13 neighborhoods obtained by drawing lots, covering the eight administrative regions of the city of Maceió, state of Alagoas, Brazil. Stage two: the selection of households was randomized, covering a sufficient number in each neighborhood to obtain the sample previously stratified by gender and neighborhood, so that the sample proportionally represented the youth population of Maceió. Stage three: visiting the households of the adolescents and their parents/guardians, which was performed by the research team, consisting of four pairs of previously trained and calibrated undergraduate students of psychology and medicine. When the household did not have an eligible adolescent, the research team went to the next neighbor’s household. If the visited household had an eligible adolescent, but he/she was not home at the time, a new visit was scheduled. When there was more than one eligible adolescent living in the same household, all were invited to participate and were included in the research collection. The researcher responsible for data analysis did not participate in the collection to ensure blinding of the research analysis.
In line with the literature,9,15 the participating adolescents were divided into three different groups regarding the frequency of NSSI: Group 1 – Without Non-Suicidal Self-Injury (WO-NSSI), adolescents in the sample who did not report self-injurious behavior, with a 0 (zero) frequency for all NSSI items; Group 2 – With Non-Suicidal Self-Injury Behaviors (B-NSSI), consisting of adolescents who showed at least one self-injurious behavior in the previous year, but who did not meet the diagnostic criteria of DSM-5; and Group 3 –Non-Suicidal Self-Injury Disorder (D-NSSI), consisting of adolescents who met the DSM-5 diagnostic criteria for a possible NSSI disorder.
The data were collected using four self-administered instruments: 1) a sociodemographic questionnaire. 2) Brazilian version of Functional Assessment of Self-Mutilation (FASM) (Escala de Comportamento de Autolesão [ECA]) –, elaborated or created by Lloyd-Richardson et al.16 in 1997, translated and adapted for Brazil by Scivoletto and Giusti17 in 2013. FASM lists 11 different types of self-injurious behaviors, with their frequency, the need for medical treatment, the influence of alcohol or drugs, suicide attempt, and 22 reasons for NSSI.18,19 It has significant psychometric properties in adolescent samples, being widely used in research on NSSI.2,4,8,9,15,17–21 3) Brazilian Barratt Impulsiveness Scale (BIS 11),22 after translation and cultural adaptation performed for the Brazilian context,23 validated and widely used to assess impulsive behavior,3 comprising 30 items to measure three factors of impulsiveness14,22,24: “motor impulsiveness,” as act without thinking, “impulsiveness due to lack of planning,” as a failure to plan for the future, focused only on the present, and “attentional impulsiveness,” such as making decisions quickly. 4) The UCLA Brazilian Loneliness Scale (UCLA-BR),25 validated in the Brazilian context, with evidence of construct and discriminant validity and good reliability, with 20 assertions for evaluating loneliness.
The data were coded and tabulated in a Microsoft Excel® (Microsoft, Excel®, WA, USA) spreadsheet. Quantitative variables were presented as mean and standard deviation, and the 95% confidence interval was calculated. Qualitative variables were presented as frequency tables. The presence of an association between independent and dependent variables was assessed using the chi-squared test. In the evaluation of the total impulsiveness and of the motor and planning impulsiveness dimensions of the three groups, the parametric ANOVA test was used, with Tukey’s post-test. In the evaluation of motor impulsiveness and the loneliness score in the three groups, Levene’s normality test was used, and then the Kruskal-Wallis non-parametric test, with Dunn’s post-test. In all analyses using the BioEstat® program (BioEstat®, PA, Brazil), p ≤ 0.05 was considered significant.
The study was approved by the Research Ethics Committee, CAAE No.61780016.0.0000.0039, Opinion No. 1.832.940. The study objectives, instruments, and contacts of the professionals involved were clarified. The adolescents’ parents or guardians signed an informed consent and the participating adolescents signed an informed assent form.
ResultsThe analyzed data are related to the 505 eligible adolescents, aged 12–17 years, living in the 13 selected neighborhoods, which cover all administrative regions of Maceió/Alagoas, Northeast Brazil.
Regarding the sample characterization, the mean age of the participants was 14.32 ± 1.61 (Mean ± SD), of both genders (50.3% males), of whom 208 (41.19%) self-declared to be brown, 335 (66.34%) attended elementary school, 230 (45.54%) adolescents reported that the family receives less than one minimum wage, and 259 (51.29%) lived with both their parents (Table 1).
Sociodemographic characteristics of the groups of adolescents: without non-suicidal self-injury (WO-NSSI), and with non-suicidal self-injury behaviors (B-NSSI), and possible non-suicidal self-injury disorder (D-NSSI).
| Sociodemographic characteristic | Sample n = 505 | % | WO-NSSI (1) n (%) | B-NSSI (2) n (%) | D-NSSI (3) n (%) | p | ||
|---|---|---|---|---|---|---|---|---|
| (2/1) | (3/1) | (3/2) | ||||||
| Gender | ||||||||
| Male | 254 | 50.30 | 148 (55.22) | 92 (46.94) | 9 (27.27) | n/s | 0.001 | 0.004 |
| Female | 251 | 49.70 | 120 (44.78) | 104 (53.06) | 24 (72.73) | |||
| Age (years) | ||||||||
| 12 | 81 | 16.04 | 43 (16.04) | 32 (16.33) | 5 (15.15) | n/s | ||
| 13 | 92 | 18.22 | 50 (18.66) | 34 (17.35) | 8 (24.24) | |||
| 14 | 108 | 21.39 | 53 (19.78) | 43 (21.94) | 9 (27.27) | |||
| 15 | 97 | 19.21 | 55 (20.52) | 37 (18.88) | 5 (15.15) | |||
| 16 | 60 | 11.88 | 30 (11.19) | 26 (13.27) | 3 (9.09) | |||
| 17 | 67 | 13.27 | 37 (13.81) | 24 (12.24) | 3 (9.09) | |||
| Skin color/ethnicity | ||||||||
| White | 152 | 30.10 | 78 (29.10) | 63 (32.14) | 9 (27.27) | n/s | ||
| Black | 98 | 19.41 | 51 (19.03) | 38 (19.39) | 8 (24.24) | |||
| Yellow | 30 | 5.94 | 15 (5.60) | 13 (6.63) | 2 (6.06) | |||
| Brown | 208 | 41.19 | 119 (44.40) | 72 (36.73) | 12 (36.36) | |||
| Native | 10 | 1.98 | 3 (1.12) | 7 (3.57) | – | |||
| Schooling | ||||||||
| No schooling | 8 | 1.58 | 4 (1.49) | 4 (2.04) | – | n/s | ||
| Grade School | 335 | 66.34 | 172 (64.18) | 135 (68.88) | 23 (69.70) | |||
| High School | 160 | 31.68 | 91 (33.96) | 57 (29.08) | 9 (27.27) | |||
| Marital status | ||||||||
| Single | 497 | 98.42 | 263 (98.13) | 194 (98.98) | 33 (100) | n/s | ||
| Married/Common-law marriage | 7 | 1.39 | 4 (1.49) | 2 (1.02) | – | |||
| Family income | ||||||||
| Minimum wages (MW) | ||||||||
| <1 MW | 230 | 45.54 | 121 (45.15) | 86 (43.88) | 21 (63.64) | n/s | 0.0087 | 0.0051 |
| 1 to 3 MW | 180 | 35.64 | 109 (40.67) | 56 (28.57) | 11 (33.33) | n/s | ||
| 3 to 5 MW | 36 | 7.13 | 16 (5.97) | 20 (10.20) | – | n/s | 0.0131 | 0.001 |
| 5 to 7 MW | 23 | 4.55 | 10 (3.73) | 12 (6.12) | 1 (3.03) | n/s | ||
| 7 to 9 MW | 4 | 0.79 | 2 (0.75) | 1 (0.51) | – | |||
| 9 or more MW | 21 | 4.16 | 8 (2.99) | 13 (6.63) | – | n/s | 0.0088 | |
| Activity | ||||||||
| Does not study or works | 16 | 3.17 | 12 (4.48) | 3 (1.53) | – | n/s | 0.0323 | n/s |
| Only studies | 456 | 90.30 | 236 (88.06) | 180 (91.84) | 33 (100) | n/s | 0.0004 | 0.0035 |
| Only works | 7 | 1.39 | 5 (1.87) | 2 (1.02) | – | n/s | ||
| Studies and works | 25 | 4.95 | 14 (5.22) | 11 (5.61) | – | n/s | 0.0206 | 0.0163 |
| Lives with | ||||||||
| Both Parents | 259 | 51.29 | 141 (52.61) | 99 (50.51) | 18 (54.55) | n/s | ||
| Mother | 147 | 29.11 | 66 (24.63) | 63 (32.14) | 12 (36.36) | n/s | ||
| Father | 15 | 2.97 | 12 (4.48) | 3 (1.53) | – | n/s | 0.0323 | n/s |
| Spouse | 6 | 1.19 | 3 (1.12) | 2 (1.02) | – | n/s | ||
| Relatives | 55 | 10.89 | 33 (12.31) | 20 (10.20) | 2 (6.06) | n/s | ||
| Others | 23 | 4.55 | 13 (4.85) | 9 (4.59) | 1 (3.03) | n/s | ||
| Number of children | ||||||||
| 0 | 488 | 96.63 | 260 (97.01) | 189 (96.43) | 32 (96.97) | n/s | ||
| 1 or more | 17 | 3.37 | 8 (2.99) | 7 (3.57) | 1 (3.03) | |||
n/s, non-significant.
Regarding the prevalence of NSSI, 33 (6.53%) adolescents met the DSM-5 diagnostic criteria for a possible disorder26 (D-NSSI); additionally, 196 (38.81%) adolescents exhibited at least one self-injurious behavior in the previous year but did not meet the DSM-5 diagnostic criteria (B-NSSI).
As for the sociodemographic differences (Table 1), the D-NSSI group had a significantly higher proportion of female adolescents. In characterizing income, the D-NSSI group had a significantly higher number of adolescents whose family income was less than one minimum wage (63.54%). Regarding the activity performed by the adolescents, all participants of the D-NSSI group reported they only studied.
Considering the different types of NSSI used (Table 2), in the B-NSSI group 148 (75.51%) adolescents used one or two different types of NSSI; on the other hand, this number was significantly higher in the D-NSSI group, as 22 (66.67%) adolescents used three or more different forms of NSSI. The most frequently used forms in the D-NSSI group were “cutting oneself” and “scratching oneself.”
Frequency, percentage, mean, and standard deviation of the types of non-suicidal self-injury (NSSI) used by adolescents in the groups with non-suicidal self-injury behaviors (B-NSSI) and with possible non-suicidal self-injury disorder (D-NSSI).
| NSSI types | B-NSSI | D-NSSI | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | Episodes Mean ± SD | 95%CI | n | % | Episodes Mean ± SD | 95%CI | p | |
| Cut oneself | 33 | 16.84 | 1.71 ± 0.95 | 1.57–1.84 | 23 | 69.70 | 9.35 ± 20.07 | 2.50–16.19 | 0.0001 |
| Hit oneself | 22 | 11.22 | 1.89 ± 0.60 | 1.80–1.97 | 15 | 45.45 | 5.8 ± 7.32 | 3.30–8.29 | 0.0001 |
| Pull one’s hair | 11 | 5.61 | 5.20 ± 4.44 | 4.57–5.82 | 5 | 15.15 | 4.2 ± 3.56 | 2.98–5.41 | 0.027 |
| Pick at sores | 103 | 52.55 | 5.90 ± 7.70 | 4.88–6.97 | 11 | 33.33 | 16.45 ± 28.90 | 6.58–26.31 | 0.006 |
| Burn oneself | 27 | 13.78 | 1.38 ± 0.74 | 1.27–1.48 | 6 | 18.18 | 9.83 ± 19.69 | 3.11–16.54 | n/s |
| Insert objects under oneself's nails or skin | 19 | 9.69 | 1.20 ± 0.45 | 1.13–1.26 | 5 | 15.15 | 4.20 ± 1.64 | 3.64–4.75 | n/s |
| Bite oneself | 107 | 54.59 | 5.36 ± 4.84 | 4.68–6.03 | 15 | 45.45 | 10.60 ± 16.77 | 4.87–16.32 | n/s |
| Pinch and poke oneself until bleeding | 11 | 5.61 | 2 | – | 12 | 36.36 | 6.33 ± 8.00 | 3.60–9.05 | 0.0001 |
| Scratch oneself | 26 | 13.27 | 2.17 ± 1.19 | 2.00–2.33 | 23 | 69.70 | 9.14 ± 21.00 | 1.97–16.30 | 0.0001 |
n/s, non-significant.
When investigating the reasons for NSSI (Table S1; Supplementary), the D-NSSI group showed a significantly higher number of answers in the item “to alleviate feelings of emptiness or indifference.” However, the item “to stop bad feelings/sensations” was the most frequently found in the two groups ( B-NSSI and D-NSSI).
When analyzing the association between NSSI and impulsiveness (Table 3), the D-NSSI group showed a significantly higher total impulsiveness score among the groups; in addition, the B-NSSI group also had a significantly higher total score than the WO-NSSI group.
Mean, standard deviation, and confidence interval of the scores of the impulsiveness (Barrat Impulsiveness Scale – BIS 11) and loneliness (Brazilian Loneliness Scale – UCLA-BR) of the groups of adolescents without non-suicidal self-injury (WO-NSSI), with non-suicidal self-injury behaviors ( B-NSSI), and with possible non-suicidal self-injury disorder (D-NSSI).
| Variable | WO-NSSI (1) Mean ± SD | 95%CI | B-NSSI (2) Mean ± SD | 95%CI | D-NSSI (3) Mean ± SD | 95%CI |
|---|---|---|---|---|---|---|
| IMPULSIVENESS TOTAL SCORE | 62.72 ± 9.36 | 61.59–63.84 | 67.23 ± 9.28b | 65.93–68.52 | 73.39 ± 10.12a·c | 69.93–76.84 |
| Motor impulsiveness | 17.96 ± 3.92 | 17.49–18.42 | 20.15 ± 4.26b | 19.55–20.74 | 21.64 ± 4.57a | 20.08–23.19 |
| Attentional impulsiveness | 15.79 ± 3.33 | 15.39–16.18 | 17.78 ± 3.71b | 17.26–18.29 | 20.09 ± 4.50a·c | 18.55–21.62 |
| Impulsiveness due to lack of planning | 28.97 ± 5.01 | 28.37–29.56 | 29.31 ± 4.84 | 28.63–29.98 | 31.67 ± 4.95a·c | 29.98–33.35 |
| LONELINESS | ||||||
| TOTAL SCORE | 11.42 ± 10.08 | 10.21–12.62 | 17.30 ± 11.95b | 15.62–18.97 | 25.48 ± 15.81a·c | 20.08–30.87 |
p ≤ 0.05 ( a 3 > 1; b 2 > 1; c 3 > 2).
When analyzing the dimensions of impulsiveness, it was observed that in “motor impulsiveness,” both the B-NSSI and the D-NSSI groups showed scores that were significantly higher than those in the WO-NSSI group.
In “attentional impulsiveness,” the D-NSSI group showed a significantly higher score among all the groups, just as the B-NSSI group also reported a significantly higher score than the WO-NSSI group.
In the “impulsiveness due to lack of planning,” the D-NSSI group showed a significantly higher level among all the groups.
Analyzing the association between NSSI and loneliness (Table 3), the D-NSSI group showed a significantly higher level of loneliness among all the groups; just as the B-NSSI group also had a significantly higher loneliness score than the WO-NSSI group.
DiscussionThe first studies27 that adopted the DSM-5 diagnostic criteria for NSSI1 reported prevalence rates between 4–7% in community samples of adolescents, data consistent with the prevalence of 6.53% of adolescents with a possible disorder (D-NSSI) identified in the present study.
The findings of the present study were similar to the research carried out in Belgium15 regarding the following: the prevalence of 7.6% for a possible D-NSSI (DSM-5); the predominance in females, also reported in several studies,4,6,9,20,26 the profile, in which the majority lived with both parents; and reporting, on average, three different NSSI methods.
In a comparative analysis between the present study and research carried out in Sweden,4 the prevalence was similar for a possible disorder (D-NSSI), according to DSM-5 (6.7% in the Swedish study and 6.53% in the present research). The socioeconomic vulnerability profile was found in both studies: in the Swedish research,4 the adolescents reported that their families were in greater financial difficulties, and in the present research, 63.64% of the adolescents in the D-NSSI group reported that their families had a family income of less than one minimum wage.
The convergence of results was also observed in the study carried out in Mexico,7 in which a prevalence of 5.6% of NSSI (DSM-5) was identified, with “relief from negative feelings” being the most frequently reported reason. This similar findings may be due to similarities regarding the sociodemographic profile, as both are developing countries in Latin America.
A Brazilian study,13 carried out in four schools in the state of Minas Gerais, identified a prevalence of 9.48% of adolescents with NSSI. According to the present study, the research conducted in Minas Gerais adopted the DSM-5 criteria and used the same instrument (FASM ). The similarities between the studies involved a predominance of females; tendency towards impulsiveness; and the main reasons for self-injury: “relieving feelings of emptiness or indifference” and “stopping bad feelings or sensations.”
Regarding the methodological aspects, when using a data collection method in the participants’ households, it was sought to minimize barriers indicated in the literature,7 because data collection performed in school environments results in not detecting information from those who were absent at the time of application or who dropped out of school, thus not being represented in the prevalence rates of most studies. Likewise, when identifying that in the present study most of the sample declared themselves to be brown (41.19%), it was possible to expand the profile on NSSI, since publications from developed countries mainly adopted samples of white/Caucasian individuals.28
In the literature, few studies have evaluated the association between loneliness and NSSI.6 In a study carried out in China 9 it was observed that NSSI was significantly associated with a higher level of loneliness. A similar profile was identified in the present study, as the loneliness score was significantly higher in the two groups with the presence of self-injurious behavior (B-NSSI and D-NSSI).
Regarding impulsiveness,14 a higher level was identified in individuals with self-injurious behaviors, as they can be motivated to obtain the immediate benefits of self-injurious behavior (e.g., relief) and have fewer concerns about the long-term consequences (e.g., scarring, discomfort, and stigmatization).
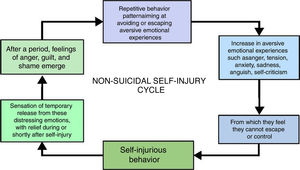
The present study proposes the “NSSI cycle” (Fig. 1), aiming to facilitate the understanding of this phenomenon. Self-injurious behavior arises when there is an increase in aversive emotional states14 such as anger, tension, anxiety, sadness, anguish, and self-criticism – from which the individuals feel they cannot escape or control. To induce a feeling of temporary release18 from these distressing emotions, they use self-injurious behaviors, which produce relief during or shortly after the self-injury. However, after a period, feelings of anger, guilt, and shame emerge, which in turn represent a further increase in aversive emotional experiences. Thus, a pattern of repetitive behavior is established, aiming to avoid or escape these distressing emotions. Despite the long-term negative consequences, NSSI is more likely to be considered an immediate solution4 for effectively interrupting unwanted emotional states. Considering that it reduces suffering, at least temporarily, it ends up reinforcing a repetitive and cyclical pattern of self-injurious behaviors.
The authors emphasize the need for intervention in adolescents with NSSI, as it is a stable behavior and may persist into adulthood. Moreover, adolescents with NSSI have a greater history18 of psychiatric treatment, hospitalization, comorbidities, and a tendency to engage in other health risk behaviors.6 Thus, the study data provide support for improving health policies,29 with the purpose of increasing protection factors30 among adolescents, contributing to their healthy psychosocial development and reducing risks and damages in adulthood.
Regarding the limitations of the present study, it should be considered that the data were collected through self-administered questionnaires and these depend on the memory and authenticity of their respondents.15 Moreover, the results reflect the reality of a capital city in the northeastern region of Brazil. Longitudinal studies with community and clinical samples are necessary to assess the DSM-5 criteria for NSSI, the course of its development, differentiation from other disorders, the short and long-term antecedents, and its consequences.
In conclusion, the present study identified the profile and prevalence of NSSI in adolescents, and its association with impulsiveness and loneliness. Regarding the prevalence, it was identified that 6.53% of the adolescents had the diagnostic criteria proposed by the DSM-5 for a possible D-NSSI. Regarding the profile, it was more prevalent in females and in young people with socioeconomic vulnerability. As for the connection, a direct association was identified between NSSI and impulsiveness and loneliness. These findings reinforce the importance of more appropriate intervention methodologies for early identification of NSSI, aiming to avoid worsening and chronicity of the condition. It should be noted that this study does not intend to exhaust the discussion on the phenomenon, but to contribute to give visibility to the topic and to assist in the creation of public health policy projects, aimed at education, prevention, and treatment of self-injuring adolescents.
Conflicts of interestThe authors declare no conflicts of interest.