To assess children with myocarditis, the frequency of various presenting symptoms, and the accuracy of different investigations in the diagnosis.
MethodsThis was an observational study of 63 patients admitted to PICU with non-cardiac diagnosis. Cardiac enzymes, chest-X ray, echocardiography, and electrocardiogram were performed to diagnose myocarditis among those patients.
ResultsThere were 16 cases of definite myocarditis. The age distribution was non-normal, with median of 5.5 months (3.25–21). Of the 16 patients who were diagnosed with myocarditis, 62.5% were originally diagnosed as having respiratory problems, and there were more females than males. Among the present cases, the accuracy of cardiac enzymes (cardiac troponin T [cTn] and creatine phosphokinase MB [CKMB]) in the diagnosis of myocarditis was only 63.5%, while the accuracy of low fractional shortening and of chest-X ray cardiomegaly was 85.7 and 80.9%; respectively. Cardiac troponin folds 2.02 had positive predictive value of 100%, negative predictive value of 88.7%, specificity of 100%, sensitivity of 62.5%, and accuracy of 90.5%.
ConclusionsChildren with myocarditis present with symptoms that can be mistaken for other types of illnesses. When clinical suspicion of myocarditis exists, chest-X ray and echocardiography are sufficient as screening tests. Cardiac troponins confirm the diagnosis in screened cases, with specificity of 100%.
Determinar as crianças com miocardite, a frequência de vários sintomas apresentados e a precisão de diferentes investigações no diagnóstico.
MétodosEstudo observacional de 63 pacientes internados na UTIP com diagnóstico de problemas não cardíacos. Os exames de enzimas cardíacas, raio-X do tórax, ecocardiograma e eletrocardiograma (ECG) foram realizados para diagnosticar miocardite dentre os pacientes.
ResultadosHouve 16 casos de miocardite definida. A distribuição etária não foi normal, com média de 5,5 meses (3,25-21). Dos 16 pacientes diagnosticados com miocardite, 62,5% foram originalmente diagnosticados como com problemas respiratórios, e a mulheres estavam em maior número que os homens. Dentre nossos casos, a precisão das enzimas cardíacas (cTn e CKMB) no diagnóstico da miocardite foi de apenas 63,5%, apesar de a precisão da baixa fração de encurtamento (FS) e do raio-X de tórax revelando cardiomegalia ter sido 85,7% e 80,9%; respectivamente. A Troponina Cardíaca em 2,02 vezes apresentou valor preditivo positivo=100%, valor preditivo negativo=88,7%, especificidade=100%, sensibilidade=62,5% e precisão=90,5%.
ConclusõesAs crianças com miocardite apresentam sintomas que podem ser confundidos com outros tipos de doenças. Quando há suspeita clínica de miocardite, raio-X de tórax e ecocardiografia são testes de rastreamento suficientes. As Troponinas Cardíacas confirmam o diagnóstico em casos examinados, com especificidade de 100%.
Myocarditis is an inflammatory condition of the myocardium characterized by leukocyte infiltration and subsequent fibrosis and necrosis.1–4 However, because children with myocarditis may be asymptomatic, the true incidence is unknown,5–7 with an estimate of around 0.05%.8–10
It is a potentially life-threatening condition,9 causing significant morbidity and mortality with long-term sequelae, including congestive heart failure (CHF) and cardiomyopathy.4,9 Since the mortality rates for infants and children with myocarditis may be as high as 75 and 25%, respectively, and early initiation of therapy is potentially beneficial, prompt diagnosis is imperative.11,12
Myocarditis in children is a challenging diagnosis to make.10 They have a wide range of non-specific signs and symptoms, overlapping with more common disorders such as respiratory distress and gastrointestinal disease.10,13,14 Most cases of myocarditis are preceded by a viral or flu-like illness,15 but bacteria, fungi, protozoa, parasites, and rickettsiae are also causative agents.16 The use of a variety of invasive and non-invasive methods is usually mandatory, mainly based on history and clinical features.17 It is clearly important to have a high degree of suspicion to diagnose myocarditis.18
Historically, the gold standard for the diagnosis of acute myocarditis required an endomyocardial biopsy according to the Dallas criteria.19,20 More recently ancillary diagnostic modalities have been used to help make the diagnosis less invasive and more rapid. The use of laboratory testing (cardiac troponin T, I [cTnT and cTnI, respectively] and creatine phosphokinase MB [CKMB]), echocardiography, and cardiac magnetic resonance imaging (MRI) can make the diagnosis in the absence of invasive biopsy.21
High-dose intravenous immunoglobulin has been proven to improve the recovery of the left ventricular function, with a tendency to present better survival rate in acute myocarditis. Considering the cost of this regimen, the accuracy of the diagnosis is essential, especially in developing countries in which the high cost of healthcare is a concern.20
This study aimed to determine the prevalence of myocarditis in association with other systems involved in critically ill cases and to test the use of cardiac enzymes (cTnT, cTnI, and CKMB), chest X-ray (CXR), and echocardiogram for screening of those cases.
MethodsThis was an observational study, in which all children admitted to Cairo university Hospital Pediatric Intensive Care Unit (PICU) were enrolled based on the following inclusion criteria:
- •
All patients presenting with respiratory distress;
- •
Symptoms and signs of heart failure;
- •
Any infectious lesions, either focal or septicemia;
- •
Multiple organ system failure.
The exclusion criteria were children with known cardiac lesions, either congenital or acquired, and presenting with heart failure.
On admission, children were subjected to full history and clinical examination: assessment of the degree of respiratory distress and need for respiratory support (oxygen or mechanical ventilation [MV]); assessment of cardiac decompensation and need for cardiac support (inotropes or antifailure drugs); routine laboratorial exams (complete blood count, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), cultures); CXR; cardiac enzymes: Troponin T, Troponin I, and CKMB; electrocardiogram; and detailed echocardiographic examination including M-mode, 2-dimensional, and Doppler echocardiography (echo) with color-coding character.
Examinations were performed using a Philips equipment with an 8MHz transducer. The following standard windows were used:
- 1.
Subxiphoid
- 2.
Apical
- 3.
Long and short parasternal
- 4.
Long and short suprasternal.
Measurement of cardiac dimensions:
The M-mode echocardiographic tracings derived from the two-dimensional echocardiography were used. It is generated from the parasternal long axis view. The M-mode cursor line was positioned perpendicular to the major axis of the left ventricle at the level of the posterior mitral valve leaflet.
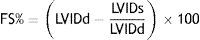
The calculation of the fractional shortening (FS%) from the data obtained from M-mode measurement followed the equation:
LVIDd, internal dimension of the diastolic LV (left ventricle). LVIDs, internal dimension of the systolic LV.22Children with suspected cardiac affection (myocarditis) by cardiac enzymes, echocardiography, or ECG were treated with intravenous immunoglobulin 2mg/kg over 48h, in accordance with the usual protocol of this PICU.
Patients were categorized as having probable myocarditis (diagnosis made by a pediatric cardiologist based on medical history, physical examination, and investigation results in the absence of an endomyocardial biopsy or no myocarditis). The investigations considered were:
- •
ECG criteria of sinus tachycardia disproportionate to the fever or age of the patient.
- •
Cardiomegaly in chest radiograph.
- •
Dilated left ventricle or both ventricles during echocardiography associated with impaired systolic or diastolic function and associated mitral valve regurgitation (MR).
- •
Cardiac enzymes mostly cardiac troponins elevated more than 2.02 folds of the normal level of the enzyme.
Echocardiographic findings (fractional shortening) or elevated cardiac enzymes were considered as the most reliable keys for diagnosis of myocarditis.
The outcome was evaluated by:
- •
Length of PICU stay,
- •
Survival to discharge,
- •
Follow-up echo.
This study was approved by Cairo University Ethics Committee, and was conducted in accordance with the guidelines for human research.
Statistical analysisNominal data were expressed as frequency and percentage and were compared using chi-squared test. Numerical data were expressed as median and range (25th–75th), and were compared using Student's t-test. Non-parametric data were compared using the Mann–Whitney test. Pearson's correlations were used to explore associations between numerical variables. A p-value <0.05 was considered as statistically significant.
ResultsThis study comprised 63 critically-ill children admitted to the PICU, following the inclusion and exclusion criteria.
Regarding their admission diagnosis, they were divided into respiratory infections (41 cases), encephalitis (12 cases), and others (ten cases; diabetic ketoacidosis, enterocolitis, Guillain-Barré syndrome, septicemia, and multisystem organ failure).
Sixteen (25.3%) of them were diagnosed with myocarditis. Among those, 62.5% (10/16) had respiratory infections as the diagnosis at admission, 12.5% (2/16) had encephalitis as the diagnosis at admission, and 25% (4/16) had either diabetic ketoacidosis, enterocolitis, Guillain-Barré syndrome, septicemia, or multisystem organ failure as the diagnosis at admission.
Although there was difference in the number of females (62.5%) versus males (37.5%) with myocarditis, this difference was statistically insignificant (p=0.126). The median age for those diagnosed myocarditis was 5.5 months (3.25–21), and for those with negative myocarditis median was 9 months (4–17; p=0.618).
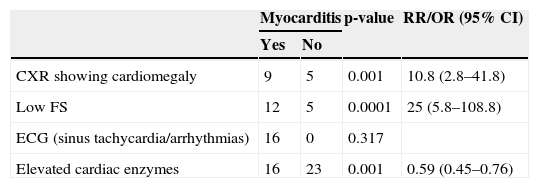
A significant association was observed between patients with myocarditis and the following investigations: CXR cardiomegaly, low FS, and elevated cardiac enzymes (Table 1). Among the cases, the accuracy of cardiac enzymes (cTn and CKMB) in the diagnosis of myocarditis was only 63.5%, while the accuracy of low FS and of CXR cardiomegaly was 85.7 and 80.9%, respectively.
Relation between different investigations and myocarditis.
| Myocarditis | p-value | RR/OR (95% CI) | ||
|---|---|---|---|---|
| Yes | No | |||
| CXR showing cardiomegaly | 9 | 5 | 0.001 | 10.8 (2.8–41.8) |
| Low FS | 12 | 5 | 0.0001 | 25 (5.8–108.8) |
| ECG (sinus tachycardia/arrhythmias) | 16 | 0 | 0.317 | |
| Elevated cardiac enzymes | 16 | 23 | 0.001 | 0.59 (0.45–0.76) |
RR, relative risk; OR, odds ratio; CI, confidence interval; CXR, chest-X ray; FS, fractional shortening; ECG, electrocardiogram.
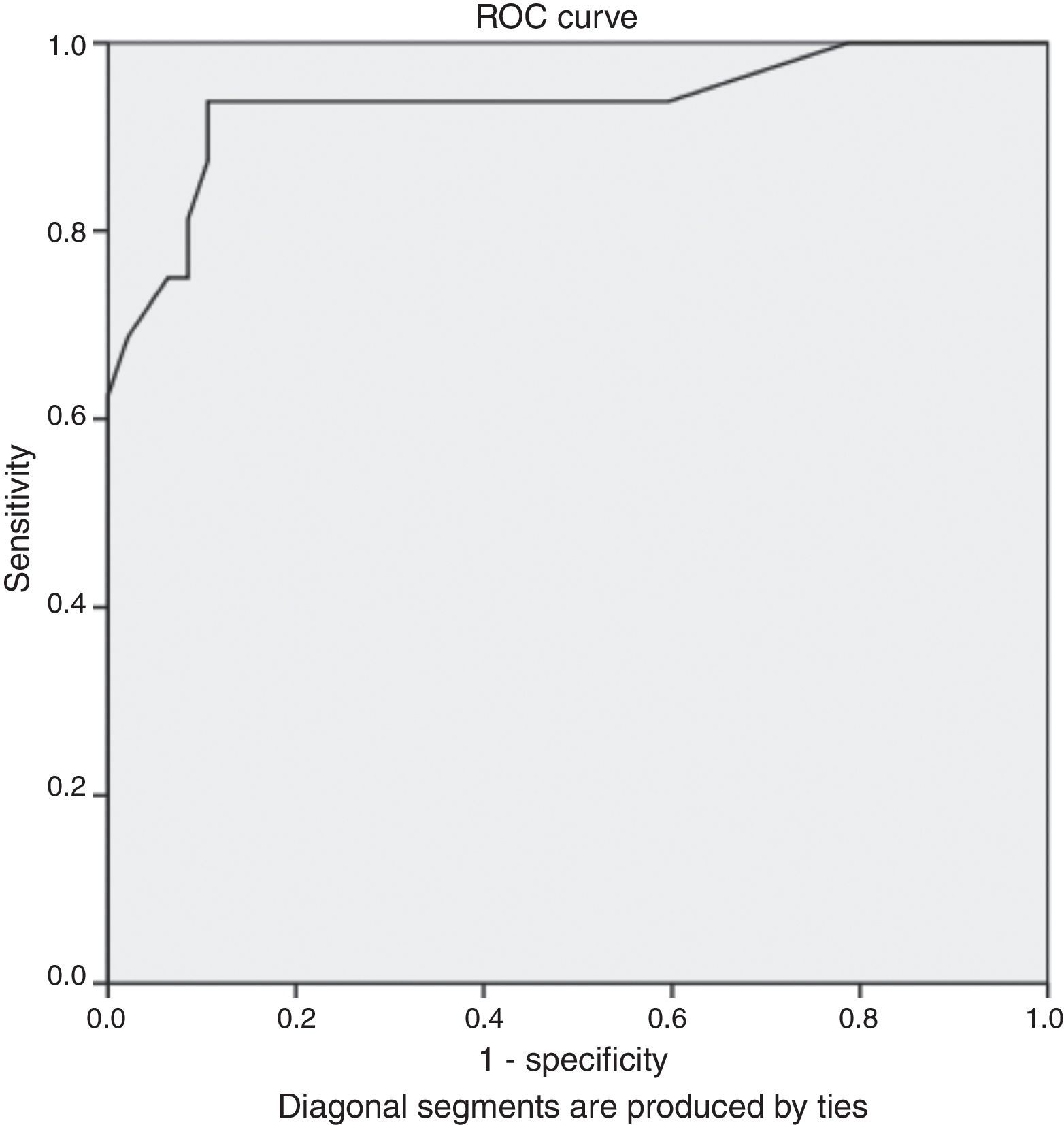
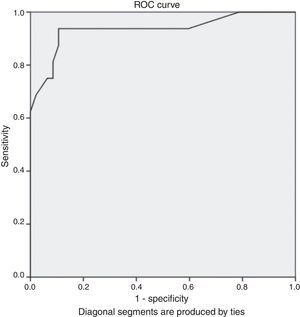
Fig. 1 presents the ROC curve of elevated cardiac troponin values represented in folds of increase. Because not all patients had the cTn level measured at the same laboratory, we considered the cTn as folds of increase rather than absolute value in order to compare them, due to reference ranges variability between different laboratories. The Area under the curve (AUC) was 0.936 (95% CI: 0.85–1, p=0.0001). Cardiac troponin folds 2.02 had a positive predictive value (PPV) of 100%, negative predictive value of negative (NPV) of 88.7%, specificity of 100%, sensitivity of 62.5%, and accuracy of 90.5%.
Negative CRP was more often found in patients diagnosed as myocarditis (62.5%; p=0.955). Fifty percent of patients diagnosed myocarditis had bandemia (p=0.412).
From the total cases diagnosed myocarditis, seven patients developed MR (7/16; 43.8%, p=0.014). Patients with myocarditis had almost five times increased odds of MR when compared with non-myocarditis patients.
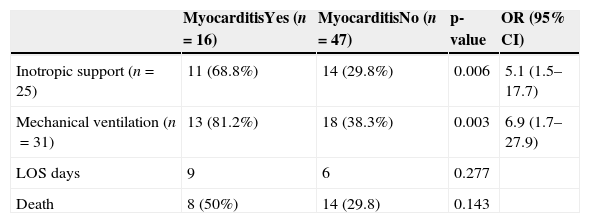
Patients with myocarditis had almost five-fold increased odds of inotropic support, and seven-fold increased odds of MV when compared with patients with no myocarditis (Table 2).
Relation between given support, length of stay, outcome, and myocarditis.
| MyocarditisYes (n=16) | MyocarditisNo (n=47) | p-value | OR (95% CI) | |
|---|---|---|---|---|
| Inotropic support (n=25) | 11 (68.8%) | 14 (29.8%) | 0.006 | 5.1 (1.5–17.7) |
| Mechanical ventilation (n=31) | 13 (81.2%) | 18 (38.3%) | 0.003 | 6.9 (1.7–27.9) |
| LOS days | 9 | 6 | 0.277 | |
| Death | 8 (50%) | 14 (29.8) | 0.143 |
OR, odds ratio; LOS, length of stay.
Median hospitalization of those diagnosed myocarditis was nine days (3.24–14.5) compared to 6 days (5–10) for those with negative myocarditis, p=0.277.
There was no significant difference regarding survival to discharge between those diagnosed myocarditis (eight cases, 50%) and those with negative myocarditis (33 cases, 70.2%; p=0.143; Table 2).
DiscussionWhile pediatric myocarditis presents with significant morbidity and mortality, data on the prevalence are limited, and the diagnosis remains challenging.10
This study provides analysis of children admitted to the PICU of Cairo University and when screened through CXR, echo, ECG, and cardiac enzymes (cTn and CKMB) it was found that the prevalence of myocarditis was 25.3%. In a post-mortem study of children who died without a history suggestive of myocarditis, researchers found evidence of active or healed myocarditis in 17 of 138 cases (12.3%).3
From those diagnosed as probable myocarditis, 62.5% had admission presentation related to the respiratory system. Freedman et al. found that 32% of their cases presented with respiratory symptoms.12 The present findings should remind clinicians that pulmonary complaints may be common for children with myocardial dysfunction, whereas cardiac findings may be minimal.23 Inflammation plays an important role in cardiac dysfunction under different situations. Acute systemic inflammation occurring in patients with severe burns, trauma, and inflammatory diseases causes cardiac dysfunction, which is one of the leading causes of mortality in these patients. Acute sepsis decreases cardiac contractility and impairs myocardial compliance.24 Although both usually have a viral cause, acute myocarditis and acute pericarditis are not always associated (in the same way that meningitis and encephalitis do not always occur together), and the clinical emphasis is usually on one or the other.25
The median age of the present myocarditis cases was 5.5 months (3.25–21), with insignificant difference compared to non-myocarditis patients. Soongswang et al. detected acute myocarditis among patients with mean age 5.4±5.1 years, p=0.912.19
Among the examinations performed, it was observed that echo (low FS) and CXR had an accuracy of 85.7 and 80.9%, respectively; hence, they can be used as screening for suspected myocarditis cases.
Cardiac enzymes cTn-folds of increase more than 2.02, had a high specificity 100%, but a low sensitivity, of 62.5%. Similar results were found in the study performed by Bohn and Benson.14 Another study found that a cTnT cutoff point of 0.052ng/ml had a sensitivity of 71% and specificity of 86% for diagnosis of myocarditis, with a false negative cTnT rate of 44%.19
In general, cardiac enzymes are elevated in myocarditis, but their reliability to detect myocarditis has been repeatedly questioned. Serum levels of cTn are more sensitive in patients with clinically suspected myocarditis than conventional determination of CKMB levels, and indicate myocyte injury. Cardiac troponin was mainly elevated in patients with acute, early-onset myocarditis, whereas the absence of increased levels suggests a long-term presence of myocarditis.26 Thus the difference in the present results compared to others can be due to the timing of blood sample collection.
Regarding the support offered to myocarditis cases, 81.2% required MV, while, in the study by Klugman et al., only 37.5% required MV.10 Moreover, inotropic support was offered to 68.8% of the present myocarditis cases, compared to around 35% in Klugman et al.’s study.10
The mortality rate among myocarditis cases was high (50%). Previous reports ranged from 13 to 38%.19,27
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Rady HI, Zekri H. Prevalence of myocarditis in pediatric intensive care unit cases presenting with other system involvement. J Pediatr (Rio J). 2015;91:93–7.
The study was conducted on PICU, New Children's Hospital, Cairo University, Cairo, Egypt.