The predisposing factors for pericarditis recurrence in the pediatric population have not yet been established. This study aimed to define the risk factors for the unfavorable prognosis of pediatric acute pericarditis.
MethodsThis was a retrospective study that included all patients with acute pericarditis treated from 2011 to 2019 at a tertiary referent pediatric center.
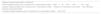
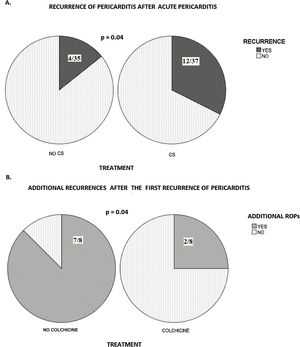
ResultsThe study included 72 children. Recurrence was observed in 22.2% patients. Independent risk factors for recurrence were: erythrocyte sedimentation rate≥50mm/h (p=0.003, OR 186.3), absence of myocarditis (p=0.05, OR 15.2), C-reactive protein≥125mg/L (p=0.04, OR 1.5), and non-idiopathic etiology pericarditis (p=0.003, OR 1.3). Corticosteroid treatment in acute pericarditis was associated with a higher recurrence rate than treatment with non-steroid anti-inflammatory therapy (p=0.04). Furthermore, patients treated with colchicine in the primary recurrence had lower recurrence rate and median number of repeated infections than those treated without colchicine (p=0.04; p=0.007, respectively).
ConclusionIndependent risk factors for recurrence are absence of myocarditis, non-idiopathic etiology pericarditis, C-reactive protein≥125mg/L, and erythrocyte sedimentation rate≥50mm/h. Acute pericarditis should be treated with non-steroid anti-inflammatory therapy. A combination of colchicine and non-steroid anti-inflammatory drugs could be recommended as the treatment of choice in recurrent pericarditis.
Acute pericarditis is the cause of cardiac-related chest pain in 1–5% of children presenting to the emergency service.1 In addition to chest pain, which increases with inspiration, children with pericarditis also have pericardial friction rub, elevated inflammatory laboratory parameters in the acute phase, and electro- and echocardiography abnormalities.2 This is usually a self-limited disease, but potential complications are incessant, chronic, recurrent, with constrictive pericarditis as the most challenging but still treatable condition. Recurrent pericarditis is defined as a relapse occurring after a symptom-free period of at least four to six weeks.2 The recurrence rate is 15% to 30% in adulthood, and it is dependent on the etiology of the acute pericarditis and colchicine use.2,3 The risk factors for recurrence of pericarditis (ROP) can be either patient or treatment-related. The factors are clearly defined in the adult population, but the definitions of risks in children are still lacking.3
This study aimed to establish the risk factors for ROP in the pediatric population.
Materials and methodsThis was a retrospective cohort study that included all patients (range 0–18 years of age) with acute pericarditis treated at the Mother and Child Health Institute of Serbia during the period from January 2011 to December 2019. The local institutional ethical committee approved the study (Ethical code number 8/34).
According to the European Society of Cardiology (ESC) guidelines, the diagnosis of acute pericarditis is based on presence on two out of four criteria: (1) Chest pain which worsens with inspiration; (2) changes in the electrocardiogram; (3) an elevated level of the reactants of the acute phase (erythrocyte sedimentation rate [ESR], C-reactive protein [CRP], white blood cells [WBC] count); (4) echocardiographic visualization of the pericardial effusion.2 The myocardium-epicardium diameter of pericardial effusion was measured in diastole in standard echocardiographic views. The classification of pericardial effusion diameter adopted was that by Pérez-Casares et al.4 Recurrent pericarditis was defined as a symptom-free interval of four to six weeks or longer and evidence of subsequent recurrence of pericarditis after documented acute pericarditis (initial presentation). Pericarditis was considered as incessant when signs and symptoms persisted for more than four to six weeks.2,3
The following data were recorded for all patients: gender, age, inflammatory parameters, etiology, echocardiographic findings, and therapeutic protocol. The etiologies of acute pericarditis were: idiopathic, PCR-positive, autoimmune and others. In patients with PCR-positive pericarditis, the viral nucleic acids of the most common cardiotropic viruses were detected by polymerase chain reaction (PCR) technique in the blood, pericardial fluid, pharyngeal swab, and stool. The samples of blood, throat, and pericardial fluid were sent for microbiology testing. Immunological analysis was performed in all patients with ROP and patients with acute pericarditis with clinical suspicion of connective tissue systemic disease. The immunological analysis involved determining the levels of IgG, IgA, IgM, C3 and C4 complement components, anti-nuclear antibodies (ANA), anti-double-stranded DNA (Anti-dsDNA), perinuclear anti-neutrophil cytoplasmic antibodies (pANCA), cytoplasmic anti-neutrophil cytoplasmic antibodies (cANCA), and rheumatoid factor (RF) in patients’ blood samples. The immune types of pericarditis covered postpericardiotomy syndrome (PPS), systemic lupus erythematosus (SLE), and Henoch-Schoenlein purpura. Although PPS is a consequence of pericardiotomy, it is believed that the etiopathogenetic basis of PPS is an autoimmune response to injury.5 The diagnosis of idiopathic pericarditis was established after the exclusion of all others putative etiologies of the disease.
Coexisting myocardial inflammatory involvement (e.g. inflammatory myopericardial syndrome) was confirmed in patients with pericarditis and an increased level of specific cardiac biomarkers (cardiac troponin I and troponin T) with or without decreased left ventricle contractility registered by echocardiography.6 Cardiac nuclear magnetic resonance was performed in all patients with an inflammatory myopericardial syndrome.
Children with pericarditis were treated with non-steroid anti-inflammatory drugs (NSAIDs), corticosteroids (CS), and colchicine. Drug dosage and tapering were mostly adapted from the ESC guidelines for the treatment of pericardial disease.2 Before the guidelines, in the majority of patients, CS was used at a dose of 1mg/kg. After the guideline, CS was administered to a few patients and at smaller doses (0.5mg/kg). Moreover, CS was added to the treatment of all patients with autoimmune pericarditis, inflammatory myopericardial syndrome, in patients with moderate to severe (echo-free space of >10mm during diastole) pericardial effusion diameter, after pericardial drainage, and in patients who did not respond adequately to NSAIDs.
After the normalization of the clinical and laboratory parameters, the drugs were stopped gradually and sequentially. CS were tapered first and slowly if they had been administered for longer than two weeks. If the dose had been>50mg/day, it was decreased by 10mg/day every one to two weeks; if the dose had been between 25 and 50mg/day, it was decreased by 5–10mg/day every one to two weeks; when the administered dose was between 15 and 25mg/day, the decrease was by 2.5mg/day every two to four weeks followed by a decrease of 1.25–2.5mg per day every two to six weeks. The next step was the tapering of NSAID, and colchicine was discontinued after several months to one year.
ROP appearance was the primary aim of the study; therefore, the influences of etiology, simultaneous myocardial involvement and, treatment of acute pericarditis on the recurrence rate were assessed.
Basic (descriptive) statistics included mean values, standard deviations, median, and interquartile range of monitored parameters. Moreover, the difference in the distribution of specific characteristics among the groups was assessed using the χ2 or Fisher's test. The normality of the distribution of numerical variables was examined by the Shapiro Wilk and Kolmogorov Smirnov tests. The comparison between the groups was made using Student's T-test, Mann–Whitney's test, and Kruskal Wallis’ test. Binominal and multinomial logistic regression analyses were used to define the relationship between the dependent binary variable and independent variables. All statistical methods were considered to be significant if the p-value was ≤0.05. Data processing was performed using statistical software SPSS 25.0 for Windows 10.
ResultsThe study included 72 patients, 52 of whom were boys (72.2%). The mean age of patients at the time of the acute pericarditis presentation was 11.5±4.0 years. The follow-up period was 36 months (range, 6–70 months). ROP was observed in 16 patients (22.2%) with a mean age of 10.9±4.9 years, 12 of whom were boys (75%; p=0.8). Patients’ age did not influence ROP onset (p=0.3). The first recurrence occurred in the mean period of four (IQR 2–6) months after the acute disease onset. The total recorded number of the recurrences was 56 (2; IQR: 1–3). One patient developed incessant pericarditis.
EtiologyThe etiology of acute pericarditis and ROP is shown in Table 1. Idiopathic acute pericarditis was the most prevalent classification among the present patients. In the group of patients with ROP, five patients presented autoimmune pericarditis. One patient had neoplastic pericarditis six months after the onset of the treatment of non-Hodgkin's lymphoma. The patient with the most prominent number of recurrences (20) had no specific genetic finding for familial Mediterranean fever. The etiology of the disease differed in groups of patients with acute and ROP (p<0.001). ROP occurred more frequently in the group with non-idiopathic pericarditis (n=11/22, 50%) than in the group with idiopathic pericarditis (n=5/50, 10%; OR 10.8; 95% CI=3.1–37.2).
Etiology of acute pericarditis and the first recurrence.
| Etiology | Acute pericarditis – n (%) | First recurrence – n (%) |
|---|---|---|
| Total | 72 (100) | 16 (100) |
| Idiopathic | 50 (69.4) | 5 (31.2) |
| ViralAdenoEBVCoxsackieParvo B 19Influenza | 11 (15.3)43211 | 4 (25.0)31000 |
| AutoimmuneSLEHenoch-Schonlein purpuraPostpericardiotomyASDMyxomaVSD | 9 (12.5)315311 | 5 (31.2)302101 |
| OtherHypothyroidismNon-Hodgkin lymphoma | 2 (2.7)11 | 2 (12.5)11 |
EBV, Epstein–Barr virus; SLE, systemic lupus erythematosus; ASD, atrial septal defect; VSD, ventricular septal defect.
Multinomial logistic regression analysis demonstrated that ESR value≥50mm/h (p=0.003, OR 186.3; 95% CI 6.1–5741.0), absence of inflammatory myopericardial syndrome (p=0.05, OR 15.2; 95% CI=0.9–254.3), CRP≥125mg/L (p=0.04, OR 1.5; 95% CI=0.003–0.9) and non-idiopathic etiology pericarditis (p=0.003, OR 1.3; 95% CI 0.002–0.3) were independent risk factors for ROP (Table 2).
Independent risk factors for ROP (multinominal logistic regression analysis).
| p-Value | OR | CI | |
|---|---|---|---|
| Non-idiopathic acute pericarditis | 0.003 | 1.3 | 0.02–2.293 |
| Treatment (NSAID+CS) | 0.346 | 2.4 | 0.39–14.20 |
| ESR≥50mm/h | 0.003 | 186.3 | 6.1–5741.0 |
| CRP≥125mg/L | 0.04 | 1.5 | 0.003–0.886 |
| Absent of myocardial inflammatory syndrome | 0.05 | 15.20 | 0.91–254.29 |
ROP, recurrence of pericarditis; NSAID, non-steroid anti-inflammatory drug; CS, corticosteroids; ESR, erythrocyte sedimentation rate; CRP, C reactive protein; OR, odds ratio; CI, confidence interval.
The mean CRP level was 116.7±58.9mg/L. At admission, mean effusion diameter was 9.9±6.2mm, and it did not affect the recurrence rate (p=0.5). Fever >38°C did not influence the recurrence rate (p=0.09). Inflammatory myopericardial syndrome was registered in 17 patients (11 patients with idiopathic and six with PCR-positive pericarditis), and in 2/17 children ROP was diagnosed. Most of these patients had a normal or nearly normal LV systolic function (EF 53.7±7.5%) at presentation and generally improved during the follow-up period (EF 63.4±3.5%; p=0.03).
The laboratory parameters (CRP, ESR, and WBC count) at admission were higher in patients with ROP than in those with acute pericarditis without recurrence (CRP: 151.6±69.9 vs. 110.9±53.1mg/L, p=0.03; ESR: 70.8±17.6 vs. 45.7±16.2mm/h, p<0.001; WBC: 19.3±4.1 vs. 15.7±3.5, p=0.003).
TreatmentAcute pericarditis treatment included NSAID with or without CS. Approximately an equal number of patients were treated without CS (35/72 or 48.6%) and with CS (37/72 or 51.4%).
The treatment was statistically different regarding the etiology of the disease (p=0.04). NSAID therapy was more often used in patients with idiopathic pericarditis. In turn, almost all patients with acute autoimmune pericarditis were treated with NSAID and CS. One patient who had been treated shortly with colchicine in acute pericarditis developed incessant pericarditis. Initially, he presented a good response, but colchicine was administered for only two weeks.
Patients with ROP treated with CS in the initial presentation had higher ESR and CRP than those patients without ROP (72.0±17.9 vs. 44.0±14.7mm/h; p=0.002, and 170.4±60.2 vs. 106.8±44.4mg/L; p=0.005, retrospectively). CS was more frequently used in patients with moderate to severe pericardial effusion (12/16; p=0.04).
Recurrence of the disease was more often observed in patients treated with CS (12/37) than in the patients treated without CS (4/35; p=0.04; Fig. 1A). A univariate regression model showed that CS treated patients had an almost four times higher recurrence rate (p=0.04, OR 3.7; 95% CI=1.1–12.9). The median number of relapses in NSAID group was 0 (IQR: 0–0) and 0 (IQR: 0–1) in CS group (p=0.04). CS was associated with a predisposition for ROP in children with idiopathic pericarditis (p<0.001). Children treated with a smaller dose of CS (0.5mg/kg; 2/12) presented a lower recurrence rate than those treated with high-dose CS (1mg/kg; 10/12; p=0.02).
Colchicine, NSAID, and CS were used for the treatment of the first ROP in deferent combinations (NSAID was used in all patients in combination with colchicine or CS). Additional relapses after the first ROP were registered in nine patients. In colchicine-treated patients, the number of additional ROPs (after the first recurrence) was lower (2/8) than in those treated without colchicine (7/8; p=0.04; Fig. 1B). Additionally, the median number of recurrences was lower in the group of patients who received colchicine (0, IQR: 0–0.75) than in the group who did not (2, IQR: 1–5; p=0.007).
Except for two patients who presented nausea during the first week of drug administration, no adverse events of colchicine were observed during the follow-up period.
DiscussionPediatric pericarditis accounts for <0.2% of the referrals to the emergency department of patients without prior cardiac disease.1 Many viruses may activate the inflammasome, and upon its activation, the proinflammatory cytokine interleukin-1 (IL-1) is released. Interleukin-1b stimulates the synthesis of inflammatory mediators, such as cyclo-oxygenase-2.7 Due to pericardial damage, antigens from the heart are released, after which patients develop anti-heart antibodies and anti-intercalated disk autoantibodies, which could be an explanation for ROP.8,9 Recurrent pericarditis is the most common complication of acute pericarditis. Risk factors are well established for adults,2,3 but not for the pediatric population.
The risks for complications in adults were separated into three groups: patient-related with or without increased risk in multivariable models and treatment-related risks3,10,11; and accordingly, the present results were stratified into similar groups (Table 3).
Risks for recurrence pericarditis in childhood, stratified into three different groups: patient-related, disease-related, and treatment-related variables with or without increased risk in multivariable models.
| Risks for recurrent pericarditis in childhood |
| Patient-related variables with increased risk in multivariable models•ESR≥50mm/h•CRP≥125mg/L |
| Disease-related variables with increased risk in multivariable models•Absence of coexistence myocarditis•Non-idiopathic etiology of acute pericarditis |
| Treatment-related variables without increased risk in multivariable models•Use of CS |
CS, corticosteroids; ESR, erythrocyte sedimentation rate; CRP, C-reactive protein.
Patient-related characteristics without increased risk in multivariable models in adults are female sex, age, and pericardial effusion diameter.3 The multicenter description that included the most prominent number of children (543 patients) with pericarditis showed that sex, age, race, in-hospital stay, treatment, and pericardial drainage did not influence the recurrence.12 That study indicated that acute pericarditis is most common in adolescents, particularly boys,12 suggesting the possibility that hormonal factors may play a role in the etiopathogenesis.6 The present results are in accordance with those findings.
Incomplete response to NSAID and elevated levels of high-sensitive CRP (hs-CRP) were defined as patient-related characteristics with increased risk in multivariable models in adults.3,10 Earlier studies in children demonstrated that the recurrence rate was higher in patients with febrile diseases associated with elevated serum inflammatory markers.13 The present study confirmed that the laboratory parameters (ESR and CRP) were independent factors for recurrence in pediatric pericarditis. ESR over 50mm/h increased recurrence rates by 186 times, and it was pinpointed as the most predictive risk factor. CRP values higher than 125mg/L increased the recurrence rate by 1.5 times. Imazio et al. showed that the presence of elevated hs-CRP during the first week of the disease increased chances for recurrence by 2.4 times.10 Some authors postulate that fever>38°C is one of the major predictive factors of complications or recurrences after acute pericarditis.9
The present study showed that the etiology of acute pericarditis was one of the independent risk factors. Children with the non-idiopathic form of the disease had a ten-fold higher chance of recurrence. A 15-fold lower predisposition for relapses was registered in patients with simultaneous myocardial inflammatory involvement. Imazio et al. demonstrated that adults with inflammatory myopericardial syndrome had less chance of having a recurrence than those with isolated pericardial infection.6 Some authors showed that the recurrence rate after inflammatory myopericardial syndrome is 13%.14 This data is in accordance with the present study.
In most studies in adults, treatment-related risks were the most important factors in the recurrence rate.2–4,10 In adults, the recommended treatment for acute pericarditis is the combination of NSAID and colchicine,2 and the lack of colchicine use and CS administration were defined as risk factors for relapses.2,3 The present study observed that the recurrence rate after CS treatment is dose-dependent, but the sample was too small for a final conclusion. The main obstacle is that there is no standardized therapy protocol for pericarditis in children. Almost half of the present patients were treated with NSAID. According to recommendations, patients were treated until clinical and laboratory findings (CRP) were normalized.15 In the present study, patients with idiopathic pericarditis treated with NSAID had a lower recurrence rate.
CS was used in cases of myocardial inflammatory involvements, moderate to severe pericardial effusions, and in cases of autoimmune etiology. Imazio et al. also added CS in the most severe cases in pediatric cases. The pericardial effusion diameter dominantly influenced the decision, as well as fever and idiopathic causes.13 Numerous authors suggested CS treatment as the second line of therapy, in cases when pericarditis is a part of connective tissue disease, autoreactive or uremic pericarditis, as well as in cases of intolerance, contraindications, or incomplete response to NSAID.1,3,6 In the present study, CS use was not classified as an independent risk factor for recurrence, but children treated with NSAID as monotherapy had lower recurrence rates and lower median number of relapses than those treated with NSAID and CS. In the case of idiopathic pericardial effusions, treatment with the drug combination had more influence on the recurrence occurrence. The occurrence of recurrences in patients treated with CS could be explained by its deleterious effect on viral replication and clearance.16
Colchicine is not routinely used as a treatment of acute pericarditis in children, but some studies showed that it prevented relapse of the disease in adults if it had been administrated for three months.2,3,17–19
In the present study, ROP was observed in 23.6% of children during the follow-up period.
Readmission was most common in the first three months after the initial presentation,10 both in the literature and in the present study. The treatment of choice in ROP was the combination of NSAID and colchicine. Some studies showed that colchicine had a favorable effect on relapses in childhood,9 while Raatikka et al. concluded that colchicine did not prevent relapses.20 In the present population, colchicine-treated patients had lower recurrence rates and lower median number of additional recurrences, without significant adverse effects. In conclusion, the authors consider the combination of NSAID and colchicine as the treatment of choice for ROP.
Children with a higher predisposition for recurrences might be treated with NSAID and colchicine in acute pericarditis, similar to the treatment for adults. Further clinical studies should be conducted to support this statement.
Anakinra is a recombinant IL-1β receptor antagonist. It is routinely used in adults who have had recurrences despite appropriate treatment.17,21–23 Picco et al. described anakinra use in three pediatric patients with CS-dependent idiopathic recurrent pericarditis.23 Some authors concluded that anakinra is a useful alternative for children with CS-dependent and colchicine-resistant pericarditis.17
To the best of the authors’ knowledge, the present study included the highest number of children with recurrent pericarditis who were treated in a single center. We showed that independent risk factors for recurrence are lack of concomitant myocardial, non-idiopathic etiology pericarditis, CRP≥125mg/L, and ESR≥50mm/h.
Although CS use was not an independent risk factor for recurrence, the recurrence rate was higher in CS-treated patients than in NSAID-treated, especially in idiopathic pericarditis. Consequently, the authors state that the treatment of acute pericarditis should not include CS. Furthermore, in children with ROP, the combination of colchicine and NSAID might be recommended as the treatment of choice.
LimitationsThe main limitation of the present study was its retrospective design. Although this is the most extensive study conducted in a single hospital, the number of patients with recurrent pericarditis is insufficient for drawing final conclusions and recommendations. Further studies with a higher number of patients should be conducted to define risk factors for ROP in childhood. In the present study, the IL-1β receptor antagonist was not used.
Conflicts of interestThe authors declare no conflicts of interest.