Evaluate the association between perinatal factors and amplitude-integrated electroencephalogram abnormalities in preterm infants on the first day of life.
MethodsThis was a cross-sectional study of 60 infants with gestational age between 23 and 32 weeks, without malformations. Infants were continuously monitored by amplitude-integrated electroencephalogram on the first day of life, for at least 3h. The tracings were recorded and analyzed in each column for the following: burst-suppression pattern, sleep-wake cycle, and amplitude of the lower margin (<3μV or <5μV). The association of maternal complications, mode of delivery, birth weight, gestational age, neonatal sex, resuscitation procedures, hypothermia on admission, and the Score for Neonatal Acute Physiology, Perinatal Extension, Version II [SNAPPE-II]) with amplitude-integrated electroencephalogram alterations was assessed by multiple logistic regression.
ResultsA discontinuous pattern occurred in 65% of infants, and a continuous pattern occurred in 23%. The burst-suppression pattern was associated with vaginal delivery (OR: 7.6; 95% CI: 1.1–53.1) and SNAPPE-II≥40 (OR: 13.1; 95% CI: 1.8–95.1). A lower margin of the amplitude-integrated electroencephalogram of <3μV was also associated with SNAPPE-II≥40 (OR: 10.6, 95% CI: 2.3–49.2), while a value <5μV was associated with lower GA (OR: 0.51, 95% CI: 0.34–0.76). There were no associations between the perinatal variables and the absence of a sleep-wake cycle in amplitude-integrated electroencephalogram recordings on the first day of life.
ConclusionBiological variables and clinical severity are associated with electroencephalographic characteristics of preterm infants on the first day of life and should be considered in clinical practice when amplitude-integrated electroencephalogram is performed.
Avaliar a associação entre fatores perinatais e anormalidades no eletroencefalograma de amplitude integrada em recém-nascidos prematuros no primeiro dia de vida.
MétodosEste é um estudo transversal de 60 bebês com idade gestacional entre 23-32 semanas, sem malformações. Os recém-nascidos foram continuamente monitorados por eletroencefalograma de amplitude integrada no primeiro dia de vida por pelo menos 3 horas. Os traçados foram registrados e analisados em cada coluna para: padrão de surto-supressão, ciclo de sono-vigília e amplitude da margem inferior (<3μV ou <5μV). A associação de complicações maternas, tipo de parto, peso ao nascer, idade gestacional, sexo do neonato, procedimentos de reanimação, hipotermia na admissão e Escore para Fisiologia Neonatal Aguda, Extensão Perinatal, versão II (SNAPPE-II) com alterações no eletroencefalograma de amplitude integrada foi avaliada por regressão logística múltipla.
ResultadosUm padrão descontínuo ocorreu em 65% dos recém-nascidos e o padrão contínuo ocorreu em 23%. O padrão de surto-supressão foi associado ao parto vaginal (OR 7,6; IC95% 1,1-53,1) e SNAPPE-II≥40 (OR 13,1; IC95% 1,8-95,1). Uma margem inferior do eletroencefalograma de amplitude integrada <3μV também foi associada com escore SNAPPE-II≥40 (OR 10,6, IC95% 2,3-49,2), enquanto um valor <5μV foi associado com menor IG (OR 0,51, IC 95% 0,34-0,76). Não houve associações entre as variáveis perinatais e a ausência de ciclo sono-vigília nas gravações de eletroencefalograma de amplitude integrada no primeiro dia de vida.
ConclusãoAs variáveis biológicas e a gravidade clínica estão associadas às características eletroencefalográficas dos recém-nascidos prematuros no primeiro dia de vida e devem ser consideradas na prática clínica quando o eletroencefalograma de amplitude integrada é realizado.
Brain function monitoring of preterm infants (PTI) is gaining importance due to the several factors that may injure their central nervous systems, especially during the first days of life.1–5 An increasingly used method is the evaluation of brain's electrical activity by amplitude-integrated electroencephalography (aEEG).6 This is due to the ease of use of the monitor, the possibility of interpretation by neonatologists at the bedside, the good correlation with conventional EEG,7,8 and because the method takes into account brain maturation.9 However, considering the multiple perinatal factors that can affect the brain's electrical activity, the interpretation of aEEG results in these patients is still limited.
In recent years, two studies have investigated the effect of perinatal factors on aEEG.10,11 Natalucci et al. analyzed aEEG tracings in the first 96h of life of neonates with gestational age (GA) <32 weeks, hemodynamic stability, and no malformations; they observed increased maturation with increases in corrected GA.10 Reynolds et al. evaluated 136 infants with GA<30 weeks for 72h in the first two weeks of life and for 4h at corrected ages of 30, 34, and 40 weeks. An immature periodic pattern in the initial aEEG was associated with a high clinical severity score, vaginal birth, male sex, and progression to death.11 However, none of the studies above assessed whether the aEEG changes observed in the first days of life were associated with perinatal factors related to peripartum maternal and neonatal variables.
In this context, the aim of the present study was to evaluate the association between perinatal factors and changes in the aEEG tracing on the first day of life in preterm infants with GA between 23 and 32 weeks.
MethodsThis cross-sectional study was conducted in the neonatal intensive care unit (NICU) of the University Hospital of Escola Paulista de Medicina of Universidade Federal de São Paulo (EPM-UNIFESP) and was approved by the Institutional Review Board (Protocol No. 10309512.7.0000.5505). The parents or legal guardians of the participating infants authorized the study by signing an informed consent.
The study participants were preterm infants with GA between 230/7 and 326/7 weeks by the best obstetric estimate, in the first 24h of life, without major congenital abnormalities. Patients who required advanced resuscitation in the delivery room, those whose mothers used illegal drugs or alcohol before birth, and those who received general anesthesia during delivery were excluded. The infants for whom the aEEG device was not available and those monitored for a period shorter than 3h were also excluded. The calculation of sample size considered the need to assess at least five independent factors for each response variable and the need to include ten to 15 patients for each independent variable analyzed in the logistic regression model,12 for a total of 60 patients.
The monitoring of the aEEG began in the first 24h of life, after admission and stabilization of the patient in the NICU, characterized by normothermia, initiation of intravenous infusion, and use of surfactants, when needed. The aEEG was monitored using an Olympic CFM 6000 monitor (Natus Medical Incorporated, California, USA). Scalp skin was prepared for electrode application.13 Two hydrogel electrodes were placed on the parietal positions P3–P4, as recommended in the international 10–20 system,14 with an approximate distance of 7.5cm between them. A neutral electrode was placed in the midline of the frontal area. The patients were monitored continuously on the first day of life for at least 3h after electrode placement. Handling of the infants was recorded in the tracings using the device markers.
The tracings were recorded and reviewed by the principal investigators using the Olympic CFM 6000 Viewer (Natus Medical Incorporated, California, USA), and the upper and lower margins of each recorded column, corresponding to a 10-min aEEG tracing, were analyzed. The recording of the aEEG tracing included the recording of raw EEGs. Raw EEG was analyzed to detect artifacts based on the pattern detailed by Hellström-Westas et al.6 If an artifact was detected, the corresponding 10-min aEEG interval was removed from the analysis. The periods of monitoring with impedance higher than 20kΩ, indicating poor electrode adhesion, were also discarded.
The variables analyzed in the aEEG, as detailed by Hellström-Westas et al.,6 were as follows: (1) predominant electrocortical background pattern (if present for over 50% of the analyzed recorded interval), classified as continuous, discontinuous, or burst suppression; (2) presence of a sleep-wake cycle (from sinusoidal variation of the lower margin to mature cycle); (3) mean lower and upper margins, reported in μV; (4) amplitude of the EEG band; (5) presence of seizures (confirmed by the raw EEG).
Maternal demographic and clinical data were collected, as well as neonatal demographic data and the procedures performed in the delivery room. After admission to the NICU, adequacy of the weight for GA,15 hypothermia at admission,16 the Score for Neonatal Acute Physiology, Perinatal Extension, Version II (SNAPPE II),17 opioid (fentanyl) administration, and caffeine treatment in the first day after birth were recorded.
The following abnormalities in aEEG in the first day of life, as defined Hellström-Westas et al.6 and Burdjalov et al.,9 were adopted as response variables in the study: (1) predominant burst-suppression pattern in the aEEG; (2) absence of sleep-wake cycle; (3) mean lower margin of the aEEG tracing <5μV; (4) mean lower margin of the aEEG tracing <3μV. For each variable, the infants with and without the alteration were compared for maternal and neonatal characteristics using the chi-squared test or Fisher's exact test for categorical variables, and Student's t-test or the Mann–Whitney test for numerical variables. To construct the logistic regression models and identify the factors associated with each of the four abnormalities in the aEEG tracing, independent variables with p<0.20 in the univariate analysis were chosen. The variables with p>0.05 were removed one by one, and the model fit was evaluated at each stage. The results were described by odds ratios (OR) and 95% confidence intervals (95% CI). All logistic models were adjusted for duration of the recorded tracings, hours of life at the beginning of monitoring, and gestational age, since the ten-week gestational age spread of the included infants could be the most important determinant of the different aEEG patterns. Because fentanyl administration presented a strong correlation with vaginal delivery and SNAPPE II≥40 (Spearman correlation; p=0.016 and p<0.001, respectively), opioid use was not included in the logistic models. The goodness of fit of all logistic models was analyzed by the Hosmer–Lemeshow test. SPSS software (IBM SPSS Statistics for Windows, v. 19.0, IBM Corp., Armonk, New York, USA) was used.
ResultsFrom June 2013 to November 2015, 2097 births occurred at this hospital. Of these, 145 infants met the inclusion criteria for the study; however, 80 were excluded for technical reasons. Of the remaining 65 patients, four were not allowed by their parents to be monitored as part of the study, and one neonate was excluded after diagnosis of a genetic syndrome. Therefore, the study included 60 preterm infants.
Among the study population, 51 (85%) were singleton pregnancies, 15 (25%) were born by vaginal delivery, 48 (80%) mothers received at least one dose of antenatal corticosteroids, 33 (55%) mothers received magnesium sulfate for neuroprotection, and ten (17%) mothers had a peripartum infection. Of the 60 neonates, three (5%) had 24 weeks of gestation, ten (17%) had 25–26 weeks, 17 (28%) had 27–28 weeks, 16 (27%) had 29–30 weeks, and 14 (23%) had 31–32 weeks. The mean GA was 28.5±2.4 weeks (range: 24–32 weeks), and the mean birth weight was 1045±369g (range: 380–2050g). Nineteen (32%) infants were small for gestational age, and 33 (55%) were male. In the delivery room, 42 (70%) infants required positive pressure ventilation, and 15 (25%) required intubation. On admission to the NICU, 23 (38%) patients had an axillary temperature <36°C. The mean SNAPPE II was 26±24, and this score was at least 40 in 16 (27%) neonates.
The aEEG recordings started at 12±6h of life, and the mean duration of the monitoring was 1281±314min (median and mode of 1440min). The aEEG tracing allowed the analysis of brain activity in 85% of these recordings. The mean lower margin was 4.2±1.3μV, and the mean upper margin was 24.6±6.0μV. The presence of continuous aEEG, discontinuous aEEG, and burst suppression was observed in 14 (23%), 39 (65%), and seven (12%) infants, respectively. A sleep-wake cycle was observed in 42 (70%) neonates, and electroencephalographic seizures were observed in two (3%) patients.
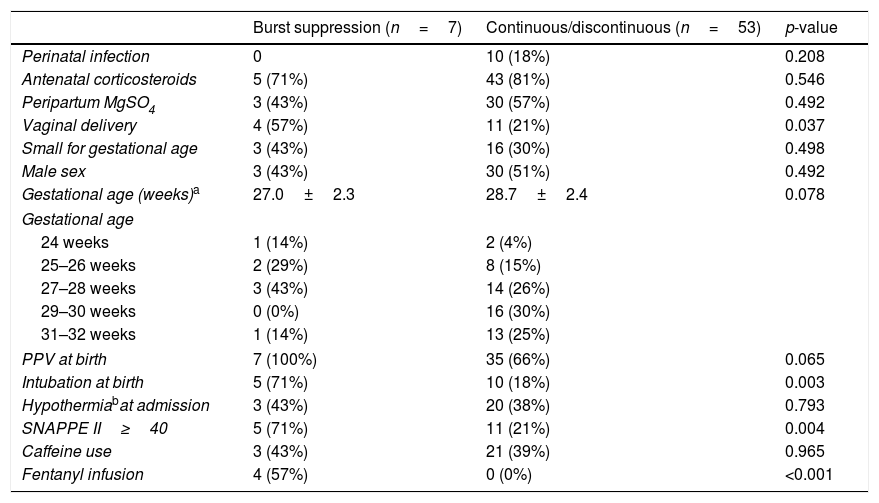
The univariate analysis of the factors associated with burst suppression in the study population is shown in Table 1. In the multivariate analysis for the outcome “burst-suppression,” two logistic models were built, considering the collinearity of the variables “positive pressure ventilation at birth” and “intubation at birth.” Both models indicated that vaginal delivery (OR=7.6, 95% CI=1.1–53.1; p=0.041) and a SNAPPE II≥40 (OR=13.1, 95% CI=1.8–95.1; p=0.011) increased the chance of the presence of a burst suppression pattern on the first day of life (Hosmer–Lemeshow test: p=0.736 for both models).
Factors associated with burst-suppression in the background pattern of the amplitude-integrated electroencephalogram (aEEG) tracing in preterm infants (PTIs) on the first day of life.
| Burst suppression (n=7) | Continuous/discontinuous (n=53) | p-value | |
|---|---|---|---|
| Perinatal infection | 0 | 10 (18%) | 0.208 |
| Antenatal corticosteroids | 5 (71%) | 43 (81%) | 0.546 |
| Peripartum MgSO4 | 3 (43%) | 30 (57%) | 0.492 |
| Vaginal delivery | 4 (57%) | 11 (21%) | 0.037 |
| Small for gestational age | 3 (43%) | 16 (30%) | 0.498 |
| Male sex | 3 (43%) | 30 (51%) | 0.492 |
| Gestational age (weeks)a | 27.0±2.3 | 28.7±2.4 | 0.078 |
| Gestational age | |||
| 24 weeks | 1 (14%) | 2 (4%) | |
| 25–26 weeks | 2 (29%) | 8 (15%) | |
| 27–28 weeks | 3 (43%) | 14 (26%) | |
| 29–30 weeks | 0 (0%) | 16 (30%) | |
| 31–32 weeks | 1 (14%) | 13 (25%) | |
| PPV at birth | 7 (100%) | 35 (66%) | 0.065 |
| Intubation at birth | 5 (71%) | 10 (18%) | 0.003 |
| Hypothermiabat admission | 3 (43%) | 20 (38%) | 0.793 |
| SNAPPE II≥40 | 5 (71%) | 11 (21%) | 0.004 |
| Caffeine use | 3 (43%) | 21 (39%) | 0.965 |
| Fentanyl infusion | 4 (57%) | 0 (0%) | <0.001 |
PPV, positive pressure ventilation; SNAPPE II, Score for Neonatal Acute Physiology, Perinatal Extension, Version II.
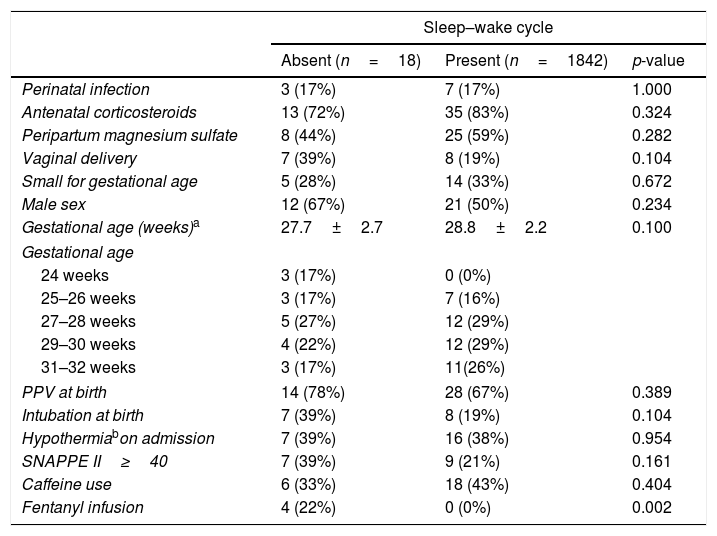
Differences between patients that did or did not present a sleep–wake cycle in aEEG tracing on the first day of life are shown in Table 2. No variables changed the chance of the absence of sleep–wake cycle in the aEEG on the first day of life in the study population.
Factors associated with the absence of sleep–wake cycle in the amplitude-integrated electroencephalogram (aEEG) tracing in preterm infants (PTIs) on the first day of life.
| Sleep–wake cycle | |||
|---|---|---|---|
| Absent (n=18) | Present (n=1842) | p-value | |
| Perinatal infection | 3 (17%) | 7 (17%) | 1.000 |
| Antenatal corticosteroids | 13 (72%) | 35 (83%) | 0.324 |
| Peripartum magnesium sulfate | 8 (44%) | 25 (59%) | 0.282 |
| Vaginal delivery | 7 (39%) | 8 (19%) | 0.104 |
| Small for gestational age | 5 (28%) | 14 (33%) | 0.672 |
| Male sex | 12 (67%) | 21 (50%) | 0.234 |
| Gestational age (weeks)a | 27.7±2.7 | 28.8±2.2 | 0.100 |
| Gestational age | |||
| 24 weeks | 3 (17%) | 0 (0%) | |
| 25–26 weeks | 3 (17%) | 7 (16%) | |
| 27–28 weeks | 5 (27%) | 12 (29%) | |
| 29–30 weeks | 4 (22%) | 12 (29%) | |
| 31–32 weeks | 3 (17%) | 11(26%) | |
| PPV at birth | 14 (78%) | 28 (67%) | 0.389 |
| Intubation at birth | 7 (39%) | 8 (19%) | 0.104 |
| Hypothermiabon admission | 7 (39%) | 16 (38%) | 0.954 |
| SNAPPE II≥40 | 7 (39%) | 9 (21%) | 0.161 |
| Caffeine use | 6 (33%) | 18 (43%) | 0.404 |
| Fentanyl infusion | 4 (22%) | 0 (0%) | 0.002 |
PPV, positive pressure ventilation; SNAPPE II, Score for Neonatal Acute Physiology Perinatal Extension, Version II.
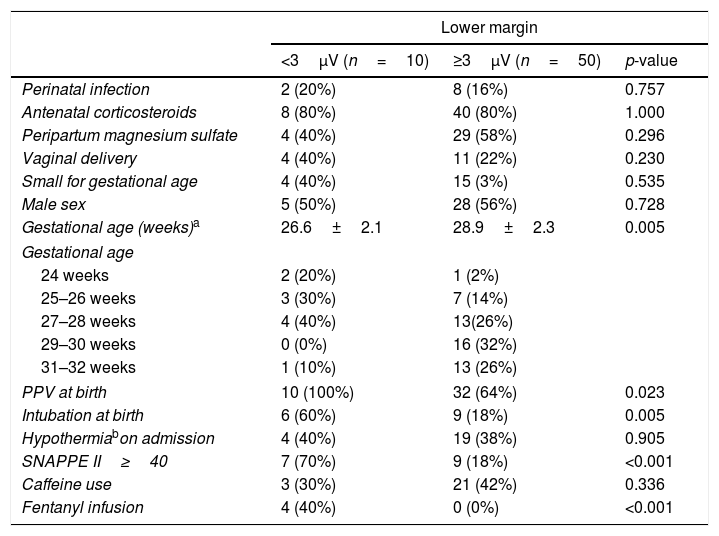
The univariate analysis of the factors associated with a lower margin, <3μV, in the aEEG of preterm infants on the first day of life is shown in Table 3. In the multivariate analysis, the presence of a SNAPPE II≥40 increased the likelihood of a lower margin, <3μV (OR=10.6, 95% CI=2.3–49.2; p=0.003; Hosmer–Lemeshow test: p=0.128). The variable “positive pressure ventilation at birth” was replaced by “intubation at birth” in the logistic model due to collinearity between them, with identical results: SNAPPE II≥40 was associated with a higher chance of detecting a lower margin <3μV in the aEEG of preterm infants on the first day of life (OR=10.6, 95% CI=2.3–49.2; p=0.003; Hosmer–Lemeshow test: p=0.128).
Factors associated with a lower margin, <3μV, on the amplitude-integrated electroencephalogram (aEEG) tracing of preterm infants (PTIs) on the first day of life.
| Lower margin | |||
|---|---|---|---|
| <3μV (n=10) | ≥3μV (n=50) | p-value | |
| Perinatal infection | 2 (20%) | 8 (16%) | 0.757 |
| Antenatal corticosteroids | 8 (80%) | 40 (80%) | 1.000 |
| Peripartum magnesium sulfate | 4 (40%) | 29 (58%) | 0.296 |
| Vaginal delivery | 4 (40%) | 11 (22%) | 0.230 |
| Small for gestational age | 4 (40%) | 15 (3%) | 0.535 |
| Male sex | 5 (50%) | 28 (56%) | 0.728 |
| Gestational age (weeks)a | 26.6±2.1 | 28.9±2.3 | 0.005 |
| Gestational age | |||
| 24 weeks | 2 (20%) | 1 (2%) | |
| 25–26 weeks | 3 (30%) | 7 (14%) | |
| 27–28 weeks | 4 (40%) | 13(26%) | |
| 29–30 weeks | 0 (0%) | 16 (32%) | |
| 31–32 weeks | 1 (10%) | 13 (26%) | |
| PPV at birth | 10 (100%) | 32 (64%) | 0.023 |
| Intubation at birth | 6 (60%) | 9 (18%) | 0.005 |
| Hypothermiabon admission | 4 (40%) | 19 (38%) | 0.905 |
| SNAPPE II≥40 | 7 (70%) | 9 (18%) | <0.001 |
| Caffeine use | 3 (30%) | 21 (42%) | 0.336 |
| Fentanyl infusion | 4 (40%) | 0 (0%) | <0.001 |
PPV, positive pressure ventilation; SNAPPE II, Score for Neonatal Acute Physiology, Perinatal Extension, Version II.
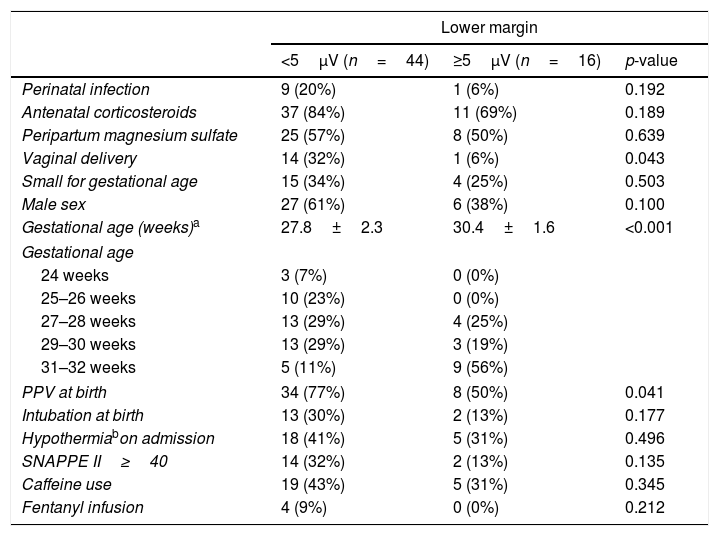
The univariate analysis of factors associated with a lower margin <5μV in the study population is shown in Table 4. In the logistic model, each additional gestational week decreased the probability of a lower margin <5μV by almost 50% (OR=0.51, 95% CI=0.34–0.761; p=0.001). The variable “sex” promoted a better model fit, although it was not significant (OR=4.03, 95% CI=0.96–16.04; p=0.057). The fit of the logistic model with the variables GA and sex showed a p-value of 0.210 in the Hosmer–Lemeshow test.
Factors associated with lower margins <5μV in the amplitude-integrated electroencephalogram (aEEG) tracing of preterm infants (PTIs) on the first day of life.
| Lower margin | |||
|---|---|---|---|
| <5μV (n=44) | ≥5μV (n=16) | p-value | |
| Perinatal infection | 9 (20%) | 1 (6%) | 0.192 |
| Antenatal corticosteroids | 37 (84%) | 11 (69%) | 0.189 |
| Peripartum magnesium sulfate | 25 (57%) | 8 (50%) | 0.639 |
| Vaginal delivery | 14 (32%) | 1 (6%) | 0.043 |
| Small for gestational age | 15 (34%) | 4 (25%) | 0.503 |
| Male sex | 27 (61%) | 6 (38%) | 0.100 |
| Gestational age (weeks)a | 27.8±2.3 | 30.4±1.6 | <0.001 |
| Gestational age | |||
| 24 weeks | 3 (7%) | 0 (0%) | |
| 25–26 weeks | 10 (23%) | 0 (0%) | |
| 27–28 weeks | 13 (29%) | 4 (25%) | |
| 29–30 weeks | 13 (29%) | 3 (19%) | |
| 31–32 weeks | 5 (11%) | 9 (56%) | |
| PPV at birth | 34 (77%) | 8 (50%) | 0.041 |
| Intubation at birth | 13 (30%) | 2 (13%) | 0.177 |
| Hypothermiabon admission | 18 (41%) | 5 (31%) | 0.496 |
| SNAPPE II≥40 | 14 (32%) | 2 (13%) | 0.135 |
| Caffeine use | 19 (43%) | 5 (31%) | 0.345 |
| Fentanyl infusion | 4 (9%) | 0 (0%) | 0.212 |
PPV, positive pressure ventilation; SNAPPE II, Score for Neonatal Acute Physiology, Perinatal Extension, Version II.
This study showed that discontinuous tracings were the predominant electroencephalographic tracings in the evaluated preterm infants, and that patients’ biological variables and their clinical severity were associated with electroencephalographic characteristics on the first day of life.
Burst suppression occurred in 12% of the preterm infants included in this study, and this rate was similar to that found by Chalak et al.18 (16%) in infants with GA<28 weeks monitored on the first day of life. Wikström et al.19 analyzed aEEG tracings during the first 72h of life and observed burst suppression in 25% of patients with GA between 28 and 30 weeks and 5 in 8% of those with GA<28 weeks. Compared to the present study, these authors monitored patients for a longer period, possibly amplifying the effect of complications associated with prematurity and neonatal care on brain electrical activity. The present results suggest an association of burst suppression with vaginal delivery and with clinical severity of infants, as demonstrated by the presence of SNAPPE II≥40. Vaginal delivery may increase central venous pressure and change cerebral blood flow, which is also affected by the clinical severity, since impaired autoregulation of cerebral blood flow is common in extremely preterm and severely ill infants.1,20 Changes in cerebral blood flow may lead to changes in brain electrical activity and the development of burst suppression. Fluctuation of cerebral blood flow is one of the mechanisms involved in the pathophysiology of peri-intraventricular hemorrhage in preterm infants, and burst suppression is associated with the occurrence of brain hemorrhages in these patients.18,21
A sleep–wake cycle was observed in 70% of the monitored patients, similar to that observed by Wikström et al.19 among infants with GA<30 weeks in the first 72h of life. The present study's result is also consistent with the findings of Soubasi et al.,22 who studied neonates with GAs<32 weeks during the first 12–72h of life. Reynolds et al.11 analyzed the perinatal factors associated with the absence of sleep–wake cycle in the first two weeks of life in neonates with GA<30 weeks, showing an association with high severity score, vaginal birth, male sex, and progression to death. In the present study, none of the evaluated perinatal factors were associated with the absence of sleep–wake cycle in the aEEG of preterm infants during the first day of life. The different results may be because Reynolds et al.11 initiated monitoring later (mean: 59h) than in the present study (mean: 12h), possibly reflecting the effects of complications of prematurity and neonatal care on the non-development of the sleep–wake cycle.
In the present study, a lower margin, <3μV, was observed in 20% of patients, which is similar to the rate of 22% found by Soubasi et al. in infants with GA<32 weeks in the first 72h of life.22 For Griesmaier et al.,23 postnatal age was strongly associated with the presence of a lower margin, <3μV. The present study's findings indicated that a SNAPPE II≥40 was associated with the presence of a lower margin on the aEEG tracing <3μV. Similarly, Horst et al. observed a negative correlation between the mean lower margin and the SNAP II clinical severity score; this correlation was stronger on the first day of life and disappeared on the fourth day of life in infants with GA between 26 and 32 weeks.24 These results suggest that the hemodynamic instability of preterm infants immediately after birth3 changes brain activity and decreases the lower margin of the aEEG tracing; this effect is stronger in the first hours of life.
A lower margin <5μV was observed in 73% of patients on the first day of life, and this result is similar to that observed by Soubasi et al.22 in preterm infants monitored during the first 72h of life. In the present study, a lower margin <5μV was associated with GA, but male sex promoted a better model fit in the multivariable analysis. Several studies indicate that the amplitude of the lower margin is associated with GA and postnatal age, and that the lower margin increases as GA increases.10,23–26 With regard to sex, Olishar et al.27 found that male sex and a lower GA increased the likelihood of abnormalities in the aEEG composite score, defined by the baseline tracing, sleep–wake cycle, and seizures.
The difference in the factors associated with lower margins <3μV and <5μV in the present study should be noted (SNAPPE II≥40 vs. GA, respectively). It may be due in part to the more intense depression of brain electrical activity in the presence of structural or biochemical changes in the central nervous system, which are common in critically ill patients, as indicated by SNAPPE II≥40.22,24 Therefore, a lower margin <3μV on the first day of life may indicate brain function abnormalities in preterm infants, whereas a lower margin between 3 and 5μV is more strongly associated with infant maturity. Indeed, a lower margin between 3 and 5μV in infants with GA<26 weeks was considered normal by Burdjalov et al.9
The incidence of seizures in the present study (3%) was similar to that observed by Lloyd et al. (5%),28 using a multi-channel EEG. However, Shah et al.,29 using a two-channel aEEG, found electrographic seizures in 13.7% of the monitored infants. The present study and that of Lloyd et al. initiated the monitoring as soon as possible after birth, while Shah et al. started, on average, at the end of the first day of life (22h), with different windows for seizures incidence and diagnosis.
The present study has limitations, particularly regarding its observational cross-sectional design. The duration of monitoring of brain electrical activity ranged between 180 and 1650min; thus, the baseline tracing might not be fully established in patients monitored for a shorter period. There was a loss of newborns eligible for the study due to the lack of equipment and other technical problems. It is notable that these problems occurred at random, which likely decreased the possibility of bias. The aEEG tracings were analyzed visually and not with software, which would have increased the accuracy of the obtained values of the lower and upper margins. However, because lower margins were compared categorically (with cutoffs at 3μV and 5μV), the visual classification of this variable did not affect the results. Finally, the tracings were analyzed by a single researcher. To overcome this limitation and increase the accuracy of the reading, each record column was analyzed individually, paying attention to the occurrence of artifacts and excluding the period in which artifacts were observed.
In conclusion, factors such GA, mode of delivery, and the clinical severity of preterm infants are associated with electroencephalographic tracing characteristics in first day of life; they should be considered and discussed when seeking a standard of normality and characterizing abnormalities in this group of patients during clinical aEEG monitoring.
FundingJCS received a grant from Brazilian Ministry of Education (Comissão de Aperfeiçoamento de Pessoal de Nível Superior [CAPES]; Ministério da Educação, Brasil).
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Castro JS, Leslie AT, Guinsburg R. Perinatal factors associated with amplitude-integrated electroencephalography abnormalities in preterm infants on the first day of life. J Pediatr (Rio J). 2020;96:644–51.
Study conducted at Universidade Federal de São Paulo, Escola Paulista de Medicina, São Paulo, SP, Brazil.