To verify the association between nutritional risk on admission and clinical outcomes of COVID-19 in hospitalized children and adolescents.
MethodsMulticenter cohort study was conducted in two cities in the northeastern region of Brazil, with children under 18 years of age laboratory diagnosed with COVID-19. Sociodemographic data and nutritional risk screening by STRONGKids (low, medium and high risk) were collected remotely and in hospital records, respectively. The outcomes assessed were the need for ICU admission, length of stay (< 10 days or ≥ 10 days), critical cases, and death. Multivariable logistic regression models were used to evaluate the effects of high nutritional risk on COVID-19 clinical outcomes.
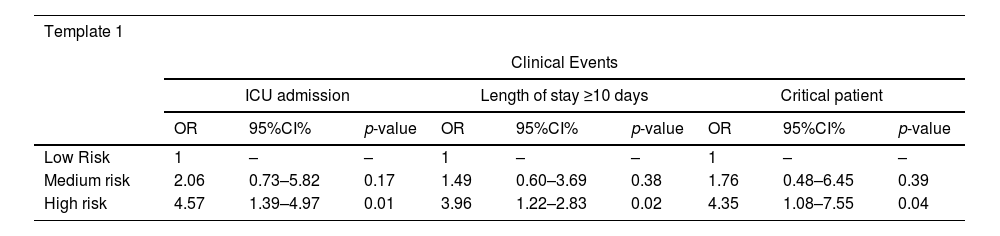
Results103 individuals were evaluated, of these 35 (34.0%) had low risk, 44 (42.7%) medium risk, and 24 (23.3%) had high risk of malnutrition. In multivariate analysis, ICU bed admission (OR: 4.57; 95%CI, 1.39-4.97; p = 0.01), hospitalization longer than or equal to ten days (OR: 3.96; 95%CI, 1.22-2.83; p = 0.02) and critical cases (OR: 4.35; 95%CI, 1.08-7.55; p = 0.04) were associated with high nutritional risk. Death was not associated with high nutritional risk.
ConclusionsChildren and adolescents with high nutritional risk by STRONGkids at hospital admission were more likely to be admitted to the ICU, have hospitalization longer than or equal to ten days, and have critical cases when infected with SARS-CoV-2.
The pediatric population has also been considerably affected by the spread of the new coronavirus, SARS-CoV-2. According to data from United Nations Children's Fund (UNICEF), it is estimated that approximately 21% of all cases and 0.4% of all deaths associated with COVID-19 were reported in children and adolescents up to 20 years of age.1 In Brazil, the 0-19 age group accounted for 2.46% of total hospitalizations and 0.62% of all deaths in the year 2020.2
Children and adolescents with COVID-19 present mostly asymptomatic or mild cases.1,3 Severe presentation has been associated with preexisting chronic conditions,3,4 and the most severe evolution is frequent in infants under 1 year of age.5 These factors have been related to an increased need for hospitalization in intensive care units, the use of invasive ventilation, and death.3,6 “Furthermore, the rate of child mortality due to Covid-19 is much higher in low- and middle-income countries than in high-income countries and may be associated with nations where access to timely and appropriate treatment as well as prevention strategies such as vaccination have not been optimal”.7
Greater severity of infection and hospitalization for SARS-CoV-2 in the pediatric population has also been demonstrated in the presence of obesity4,5 or malnutrition,8,9 the latter as a condition still prevalent in low and middle-income countries, which is a risk factor for insufficient immune response in infectious diseases.8 A previous inadequate nutritional status in pediatric patients, in general, negatively interferes with recovery and disease prognosis.8 Also, infectious processes and prolonged hospitalization may favor impaired nutritional status in this age group.10
In the context of the pandemic by COVID-19, where access to patients was sometimes restricted, nutritional risk screening tools contributed to the prediction of nutritional status.11 In hospitalization, these tools, which are practical and fast to apply, have been widely used, helping to identify the nutritional status and enabling early nutritional intervention, preventing morbidity and mortality12,13 Literature data show an association between higher risk in nutritional screening and longer hospitalization time by COVID-19 in the pediatric age group.11
Thus, considering that the nutritional status influences the clinical evolution during hospitalization10 and that there is a nutritional risk screening tool validated in Brazil,13 widely used in hospital settings, in addition, to the need for understanding the course of SARS-CoV-2 infection in the pediatric population, the objective of this study is to verify the association between nutritional risk at admission and the clinical outcomes of COVID-19 in hospitalized children and adolescents.
MethodsDynamic cohort study with non-probability sampling, consisting of children and adolescents hospitalized from July 2020 to July 2021 in health services in Salvador and Natal, cities in northeastern Brazil. The study was approved by the Research Ethics Committee (REC) of the coordinating center at the Universidade Federal de Alagoas, under opinion number 4.090.285/2020, and by the RECs of the centers participating in the study. Ethical and bioethical principles were respected in all stages of the research, according to Brazilian legislation and the Declaration of Helsinki.
Initially, the patients were identified by health professionals, who were part of the team, in the research hospitals. Then, the admission to the study was carried out by a remote collection team, through telephone contact, after agreeing to voluntary participation in the study by signing the informed consent form (ICF), the guardians, and the informed consent form (ICF), children and adolescents aged seven years or older. The Informed Consent Form was waived in cases where death had occurred before admission to the study.
Children and adolescents between 0 and 18 incomplete years of age, hospitalized and with a laboratory diagnosis of COVID-19 by RT-PCR (Reverse Transcription Polymerase Chain Reaction) were included in this study. In addition, patients who had not been evaluated by nutritional risk screening tool and/or did not have information on the primary outcome related to COVID-19 (discharge/healing or death) and the secondary outcomes, type of hospitalization (clinical bed or intensive care unit - ICU), clinical condition of the disease (critical or non-critical) and length of hospitalization (< 10 days or ≥ 10 days) were excluded.
Demographic and socioeconomic dataThe adults responsible for the patients remotely provided demographic data (gender and age) and socioeconomic data, by answering questions from the Brazilian Economic Classification Criterion – CCEB.14 In this study, participants were categorized into classes A-B-C, as better off socioeconomically favored, and classes DE, when less favored.
Clinical data of hospitalization by COVID-19Data from hospital records were collected by professionals from hospitals, regarding the type of hospital stay (clinical or ICU), presence of comorbidities (hypertension, diabetes, cancer, heart disease, respiratory diseases, chronic renal failure, others), type of feeding route (oral or enteral/tube) and characterization of the outcome (discharge/healing or death). Length of hospital stay was categorized in days (<10 or ≥10 days) from the 50th percentile of the study population.
Regarding the clinical classification of COVID-19, clinical signs and symptom information were considered for definition, as indicated by the Chinese expert consensus.15 The ‘critical cases’ were those who required ICU care and meet any of the following criteria: 1. respiratory failure that requires mechanical ventilation, 2. shock, and 3. combined with the failure of other organs. The remaining cases were characterized as "non-critical".
Nutritional risk screeningThe nutritional risk screening information by the STRONGkids12 tool was obtained from the hospital records. This tool is a four-question questionnaire for nutritional risk assessment, which addresses aspects of the subjective clinical assessment, previous comorbidities, weight changes, food intake, and losses. This score generates a score of up to 5 points, and nutritional risk is characterized as high risk (4-5 points), medium risk (1-3 points), and low risk (0= no score).
Anthropometric dataWeight and height were measured in the hospital environment, and the Z scores of the body mass index for age (BMI/I) were calculated. Nutritional status was characterized according to World Health Organization guidelines,16 with children up to 5 years of age with a Z score < -2 standard deviations categorized as lean, and with a Z score > 2 SD as overweight (overweight or obese); for children 5 years and older and adolescents with a Z score < -2 SD categorized as lean, and with a Z score > +1 SD as overweight. Children or adolescents requiring unconventional methods for anthropometric assessment were not assessed, due to lack of data for estimation.
Statistical analysisThe Statistical Package for Social Sciences (SPSS) software, version 20.0 (IBM Inc, Chicago, IL, USA) was used for statistical analysis. The variables were checked for normality (Kolmogorov-Smirnov test). The chi-square test or Fisher's exact test was used for a univariate association between categorical variables, and Kruskal-Wallis was used for the analysis of variance. Multivariable binary logistic models, adjusted based on sex and age were used to calculate the adjusted odds ratio (OR) between STRONGkids categories (low, medium, and high nutritional risk) and secondary outcomes (length of stay, type of hospitalization, and critical cases). For the multivariable binary logistic model of the outcome, death STRONGkids was categorized into two groups (low/medium risk = score < 4; high risk = score 4). All analyses considered a significance value of less than 5%. Considering the statistical test (Chi-square) and the effect size (d = 0.234), calculated from the frequency of death in the low, medium, and high-risk groups. To obtain a power of 80%, keeping the effect size and α = 5%, a total of 235 individuals would be necessary (G*Power Software, version 3.1.9.2).
ResultsThis study had an initial sample consisting of 120 patients, where 15 were excluded for not having information about STRONGKids nutritional risk screening, 1 patient for not having information about the length of hospitalization, and 1 child for not having information about the type of hospitalization (clinical bed or ICU). Thus, the study population consists of 103 children and adolescents.
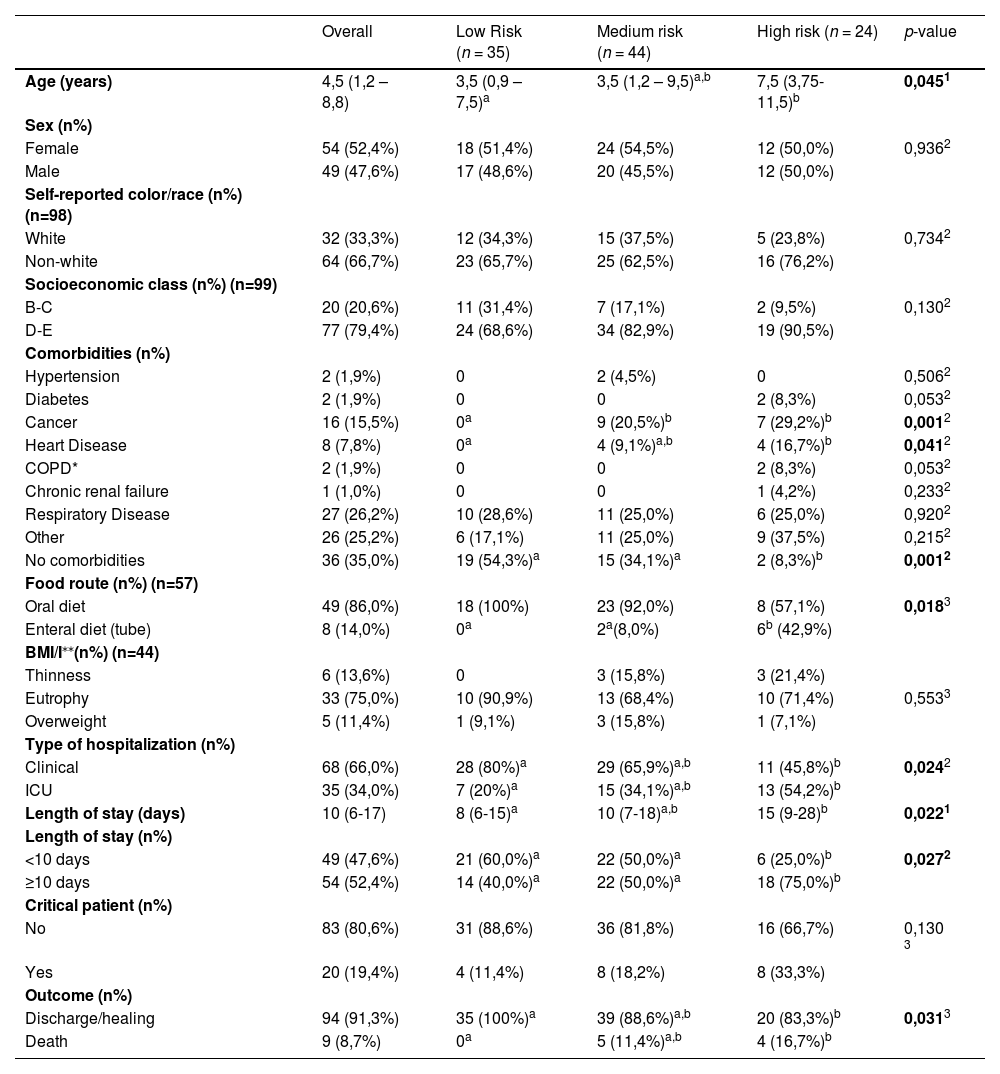
In the nutritional risk assessment, it was found that 35 (34.0%) had low risk, 44 (42.7%) medium risk, and 24 (23.3%) had high risk. There was a statistically significant difference in age when comparing the low and high nutritional risk categories [3.5 (0.9–7.5) versus 7.5 (3.75-11.5) years, respectively; p = 0.045]. Regarding previous comorbidities, a higher frequency of cancer was seen in the medium and high-risk groups compared to the low risk [9 (20.5%); 7 (29.2%) vs 0, respectively; p = 0.001)]; heart disease was more frequent in the high-risk group compared to those at low risk [4 (16.7%) vs 0, respectively; (p = 0.041)]. In 19 (54.3%) patients at low risk and 2 (8.3%) at high risk, no comorbidities were reported (p = 0.001) (Table 1).
Sociodemographic and clinical characteristics and outcomes of COVID-19 in hospitalized children and adolescents, according to the nutritional risk categories by STRONGkids.
| Overall | Low Risk (n = 35) | Medium risk (n = 44) | High risk (n = 24) | p-value | |
|---|---|---|---|---|---|
| Age (years) | 4,5 (1,2 – 8,8) | 3,5 (0,9 – 7,5)a | 3,5 (1,2 – 9,5)a,b | 7,5 (3,75-11,5)b | 0,0451 |
| Sex (n%) | |||||
| Female | 54 (52,4%) | 18 (51,4%) | 24 (54,5%) | 12 (50,0%) | 0,9362 |
| Male | 49 (47,6%) | 17 (48,6%) | 20 (45,5%) | 12 (50,0%) | |
| Self-reported color/race (n%) (n=98) | |||||
| White | 32 (33,3%) | 12 (34,3%) | 15 (37,5%) | 5 (23,8%) | 0,7342 |
| Non-white | 64 (66,7%) | 23 (65,7%) | 25 (62,5%) | 16 (76,2%) | |
| Socioeconomic class (n%) (n=99) | |||||
| B-C | 20 (20,6%) | 11 (31,4%) | 7 (17,1%) | 2 (9,5%) | 0,1302 |
| D-E | 77 (79,4%) | 24 (68,6%) | 34 (82,9%) | 19 (90,5%) | |
| Comorbidities (n%) | |||||
| Hypertension | 2 (1,9%) | 0 | 2 (4,5%) | 0 | 0,5062 |
| Diabetes | 2 (1,9%) | 0 | 0 | 2 (8,3%) | 0,0532 |
| Cancer | 16 (15,5%) | 0a | 9 (20,5%)b | 7 (29,2%)b | 0,0012 |
| Heart Disease | 8 (7,8%) | 0a | 4 (9,1%)a,b | 4 (16,7%)b | 0,0412 |
| COPD* | 2 (1,9%) | 0 | 0 | 2 (8,3%) | 0,0532 |
| Chronic renal failure | 1 (1,0%) | 0 | 0 | 1 (4,2%) | 0,2332 |
| Respiratory Disease | 27 (26,2%) | 10 (28,6%) | 11 (25,0%) | 6 (25,0%) | 0,9202 |
| Other | 26 (25,2%) | 6 (17,1%) | 11 (25,0%) | 9 (37,5%) | 0,2152 |
| No comorbidities | 36 (35,0%) | 19 (54,3%)a | 15 (34,1%)a | 2 (8,3%)b | 0,0012 |
| Food route (n%) (n=57) | |||||
| Oral diet | 49 (86,0%) | 18 (100%) | 23 (92,0%) | 8 (57,1%) | 0,0183 |
| Enteral diet (tube) | 8 (14,0%) | 0a | 2a(8,0%) | 6b (42,9%) | |
| BMI/I⁎⁎(n%) (n=44) | |||||
| Thinness | 6 (13,6%) | 0 | 3 (15,8%) | 3 (21,4%) | |
| Eutrophy | 33 (75,0%) | 10 (90,9%) | 13 (68,4%) | 10 (71,4%) | 0,5533 |
| Overweight | 5 (11,4%) | 1 (9,1%) | 3 (15,8%) | 1 (7,1%) | |
| Type of hospitalization (n%) | |||||
| Clinical | 68 (66,0%) | 28 (80%)a | 29 (65,9%)a,b | 11 (45,8%)b | 0,0242 |
| ICU | 35 (34,0%) | 7 (20%)a | 15 (34,1%)a,b | 13 (54,2%)b | |
| Length of stay (days) | 10 (6-17) | 8 (6-15)a | 10 (7-18)a,b | 15 (9-28)b | 0,0221 |
| Length of stay (n%) | |||||
| <10 days | 49 (47,6%) | 21 (60,0%)a | 22 (50,0%)a | 6 (25,0%)b | 0,0272 |
| ≥10 days | 54 (52,4%) | 14 (40,0%)a | 22 (50,0%)a | 18 (75,0%)b | |
| Critical patient (n%) | |||||
| No | 83 (80,6%) | 31 (88,6%) | 36 (81,8%) | 16 (66,7%) | 0,130 3 |
| Yes | 20 (19,4%) | 4 (11,4%) | 8 (18,2%) | 8 (33,3%) | |
| Outcome (n%) | |||||
| Discharge/healing | 94 (91,3%) | 35 (100%)a | 39 (88,6%)a,b | 20 (83,3%)b | 0,0313 |
| Death | 9 (8,7%) | 0a | 5 (11,4%)a,b | 4 (16,7%)b |
Regarding clinical characteristics, the median length of stay increased progressively the higher the nutritional risk, and a statistically significant difference was seen between low-risk and high-risk categories [8 (6–15) vs 15 (9-28) days; p = 0.022]. The need for ICU admission was more frequent in the high-risk group compared to the low risk [13 (54.2%) vs 7 (20.0%), respectively; p = 0.024]. A higher frequency of death was seen in patients at high risk, with a statistical difference compared to those at low nutritional risk, in which no case of death was found [4(16.7%) vs 0, respectively; p = 0.030]. As for the criticality of COVID-19, no difference was found between the nutritional risk categories.
In sub-sample analysis, the feeding route was evaluated in 57 patients (18 low risk, 25 medium risk, and 14 high risk), and 8 (14.0%) had tube feeding. A higher frequency of tube feeding was observed among those at high risk [6 (42.9%)] when compared to those at low and medium risk [0; 2 (8.0%), respectively; p = 0.018].
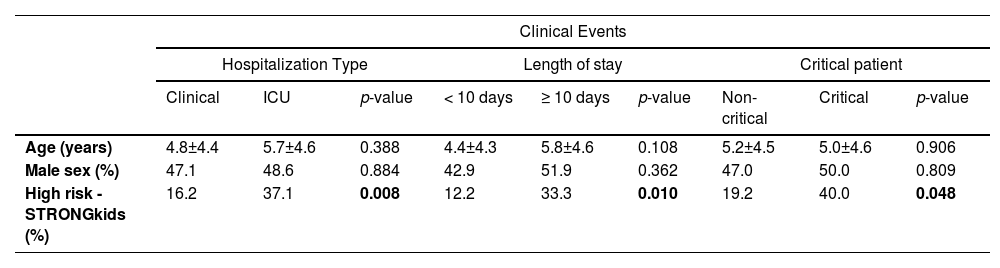
In univariate analysis, only high risk by STRONGkids showed statistical significance for the clinical outcomes type of hospitalization (p = 0.008), length of stay (p = 0.010), and critical cases (p = 0.048) (Table 2). Multivariate analysis was performed to identify the association between the STRONGkids categories with the clinical outcomes studied (Table 3). In model (n = 103) the adjustment variables were age and gender, identifying that ICU bed admission (OR: 4.57; 95%CI, 1.39-4.97; p = 0.01), hospitalization longer than or equal to ten days (OR: 3.96; 95%CI, 1.22-2.83; p = 0.02) and critical cases (OR: 4.35; 95%CI, 1.08-7.55; p = 0.04) were associated with high nutritional risk. No association was observed between death and high nutritional risk (OR: 2.96; 95% CI, 0.73-12.06; p = 0.068).
Univariate analysis between predictor variables and clinical outcomes of COVID-19 in hospitalized children and adolescents (n = 103).
Multivariate analysis between nutritional risk categories by STRONGkids on admission and clinical outcomes of COVID-19 in hospitalized children and adolescents.
OR, odds ratio; CI, confidence interval. Analyses adjusted for age and sex (n =103).
In this study where pediatric patients with COVID-19 were evaluated during hospitalization, it was found that patients with high nutritional risk had a higher frequency of ICU admission, longer length of stay, and critical clinical condition, related to SARS-CoV-2 infection.
The need for intensive care unit support is one of the clinical parameters to assess the severity of the course of COVID-19 in children and adolescents.15 A systematic review with meta-analysis17 that included 9335 children indicated that 22.9% were admitted to an ICU bed. A multicenter cohort18 found similar, noting 18% of 651 individuals requiring intensive care support. In the present study, 34% of the evaluated patients were in intensive care, and those who were at high nutritional risk had almost 5 times more chance of ICU admission. The present result is similar to a retrospective study11 carried out in São Paulo, where 40.5% of patients were admitted to ICU, which was associated with higher nutritional risk by STRONGkids, compared to those with lower nutritional risk [75% vs 28.3%; (p= 0.000)].
As for the length of hospital stay, data from a meta-analysis19 showed a mean of 10.3 days in the pediatric population with COVID-19, similar to the median of 10 days of hospitalization observed in the present findings. The authors found too, that high nutritional risk was associated with hospitalization for 10 days or longer.
Zamberlan and colleagues11 observed an association between longer hospital stays with higher nutritional risk assessed by STRONGkids, in children and adolescents with COVID-19, where STRONGkids ≥ 4 points was related to a later discharge date (p = 0.0107). The association between high nutritional risk and lower chance of hospital discharge has already been described in another study20 that evaluated 641 Brazilian individuals, in the period from 2014 to 2018. The relationship between high nutritional risk and length of hospital stay, in studies with patients hospitalized with COVID-19, is still scarce.
Another result observed in this study is related to the classification of the clinical condition of COVID-19 as a critical case and took into account information from clinical signs and symptoms for definition,15 with respiratory failure, indicated by requiring mechanical ventilation, being a main parameter. A high percentage of critical cases of COVID-19 (19.4%) was found, possibly because the authors evaluated a population of hospitalized patients. Regarding this outcome, a 4 times greater chance was found for children and adolescents with high nutritional risk to present a critical case of the disease. A systematic review21 described a 0.6% percentage of critical conditions of COVID-19 in the general pediatric population. Another study22 in Korea, with 39,146 individuals under 18 years of age diagnosed with COVID-19 identified 0.02% critical cases, considering similar parameters for defining the criticality of the disease.
In the present study, it was found that those with high nutritional risk by STRONGkids had higher median age when compared to patients with low or medium nutritional risk. Other authors11 who evaluated the nutritional risk of children and adolescents hospitalized with COVID-19 found that the mean age was also significantly higher in children with higher nutritional risk (mean of 10.5 years). Also, was observed that 2/3 of the deaths occurred in children under 5 years of age. This finding supports previous data that showed higher death rates associated with COVID-19 in infants and young children compared to other pediatric age groups.23
Another result observed refers to the fact that the majority (65%) of children and adolescents evaluated had previous comorbidities. Moreover, patients with high nutritional risk by STRONGkids showed a higher frequency of comorbidities cancer, and heart disease. This finding corroborates the literature, since the presence of comorbidities in patients with COVID-19 has been associated with more severe cases of the disease, also in the pediatric population,3,4 including greater need for hospitalization3,6 and need for intensive care.22
In this sense, it is important to highlight the characteristics of the screening tool STRONGkids,13 which scores disease with risk of malnutrition or prediction of major surgery, which directly influences the total score for categorization of nutritional risk.
A study in the UK that assessed comorbidities in children and adolescents hospitalized with COVID-19 found that 7.4% of the individuals had hematological, oncological, or immunological diseases.22 In a study conducted in Brazil, 27.1% of the cases of death in children hospitalized with COVID-19 had immunopathies.23 In the present study there was a percentage of cancer in 16.3%, a fact that may be associated with one of the partner hospitals in the study being a reference for children with cancer, but also because this comorbidity is associated with greater severity of COVID-19 in this population. A cohort study conducted in 131 pediatric institutions in 45 countries24 found that the mortality of children with cancer due to COVID-19 was four times higher when compared to the general pediatric population.24 The increased nutritional risk in children and adolescents with cancer is due to the increased metabolic demand of the disease and the treatment itself, where symptoms such as loss of appetite, vomiting, diarrhea, and mucositis are recurrent and can cause nutritional deficit.25
The same Brazilian study23 also found that of hospitalized children and adolescents, 25.6% of those who died and 18.3% of those who recovered from COVID-19 had some heart disease, while a study conducted in the UK found that approximately 6% of children hospitalized with COVID-19 had heart disease,18 similar to what was found in the present study. It is known that the risk of malnutrition in the pediatric population with chronic cardiac conditions occurs due to a higher metabolic demand because, besides the high demands for growth and development of the child, chronic cardiac diseases in general increase cardiorespiratory work, hypertrophy and cardiac muscle enlargement added to the occurrence of hypoxia and other factors that increase oxygen consumption and energy demand.26
The case fatality rate among hospitalized children was 8.7% (9 deaths in 103 cases hospitalized), with no deaths among children with low nutritional risk. Data from a meta-analysis involving hospitalized pediatric population with COVID-19 found that children with pre-existing medical conditions died more often (1.5%), revealing a higher mortality risk in those with pre-existing comorbidities compared to pediatric patients without comorbidities, the relative risk being 2.81.4
Similar to the present study, in multivariate analysis, another group of scholars,11 found no significant association between higher nutritional risk and the occurrence of death in children and adolescents hospitalized with COVID-19. The association of higher risk of malnutrition with higher mortality frequency from COVID-19 was described in adults, with a 1.23 times higher risk of death every 1 unit increase in the NRS (Nutritional Risk Screening 2002) score.27
The present study found no association between high nutritional risk and death from COVID-19. Based on this observation, the power of the test was analyzed. Considering the statistical test a total of 235 individuals would be necessary. Therefore, this constitutes a limitation of the study, which may justify the non-obtaining of statistical evidence in some analyses.
Other limitations of the study are the fact that most of the data were obtained by remote collection or by data from medical records, due to the restrictions of the pandemic period, with possible losses derived from incomplete information. Still, the authors need to consider the fact that STRONGKids is a nutritional screening tool, and its isolated use does not provide a nutritional diagnosis, being necessary to be associated with other methods such as anthropometry.12
It is important to note that in Brazil, the application of vaccines for adolescents was started in September 2021, and for children aged 5 to 11 years from January 2022, reducing the number of severe cases and the need for hospitalization.27 However, the information from the present study was conducted between the possible first and second waves of the disease in Brazil, before vaccination started in the pediatric population.
In conclusion, it was possible to verify the association between high nutritional risk by STRONGKids with ICU admission, longer length of stay, and critical clinical condition in children and adolescents hospitalized with COVID-19 in two cities in the northeastern region of Brazil. Based on the present findings, the authors observed the importance of applying a nutritional risk screening tool upon hospital admission of the pediatric patient, as part of the nutritional assessment that enables early nutritional intervention, in addition to adjuvant in characterizing the clinical prognosis of children and adolescents infected by SARS-CoV-2.
FundingThis study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior-Brasil (CAPES)-Finance Code 001.