To evaluate the ability of neck circumference to identify excess android fat and to propose cutoff points for Brazilian children.
MethodThis was a cross-sectional study with 376 children aged 8 and 9 years enrolled in public and private schools in the urban area of the municipality of Viçosa, Minas Gerais. A semi-structured questionnaire containing sociodemographic and lifestyle information was applied. The following were collected: neck circumference, weight, and height for the calculation of body mass index. The percentage of fat in the android region was determined by dual energy X-ray absorptiometry. Linear regression analysis was used to evaluate the association between neck circumference and android fat, adopting a significance level of 5%. Receiver operating characteristic curves were used to evaluate the capacity of neck circumference to determine the excess android fat, as well as to estimate the cutoff points of neck circumference according to gender.
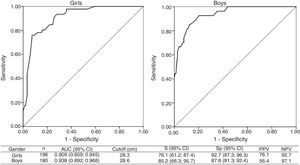
ResultsMultiple linear regression showed an association between neck circumference and android fat (β: 2.94, 95% CI: 2.41, 3.47). Neck circumference was able to identify excess android fat in girls (AUC: 0.909, 95% CI: 0.999, 0.945) and boys (AUC: 0.938, 95% CI: 0.892, 0.968). The proposed cutoff points showed satisfactory sensitivity, specificity, and predictive values.
ConclusionsNeck circumference is capable of identifying excess android fat in children and can be used in clinical practice and in population studies to determine central adiposity. The proposed cutoff points were satisfactory, but should be validated for other populations.
Avaliar a capacidade do perímetro do pescoço em identificar o excesso de gordura androide e propor pontos de corte para crianças brasileiras.
MétodoEstudo transversal com 376 crianças de oito e nove anos, matriculadas em escolas públicas e privadas da área urbana de Viçosa, Minas Gerais. Foi aplicado um questionário semiestruturado contendo informações sociodemográficas e de estilo de vida. Foram coletados: perímetro do pescoço, peso e estatura para o cálculo do índice de massa corporal. O percentual de gordura na região androide foi determinado pela absorciometria de raios X de dupla energia. A análise de regressão linear foi utilizada para avaliar a associação entre o perímetro do pescoço e a gordura androide, adotando-se o nível de significância de 5%. Por meio das curvas Receiver Operating Characteristic avaliou-se a capacidade do perímetro do pescoço de determinar o excesso de gordura androide, bem como estimaram-se os pontos de corte de perímetro do pescoço segundo o sexo.
ResultadosA regressão linear múltipla demonstrou associação entre o perímetro do pescoço e a gordura androide (β: 2,94; IC95%: 2,41; 3,47). O perímetro do pescoço foi capaz de identificar o excesso de gordura androide em meninas (AUC: 0,909; IC95%: 0,859; 0,945) e meninos (AUC: 0,938; IC95%: 0,892; 0,968). Os pontos de corte propostos tiveram valores de sensibilidade, especificidade e preditivos satisfatórios.
ConclusõesO perímetro do pescoço é uma medida capaz de identificar o excesso de gordura androide em crianças, pode ser usado na prática clínica e em estudos populacionais para determinar a adiposidade central. Os pontos de corte propostos foram satisfatórios, entretanto devem ser validados para outras populações.
Childhood obesity is considered a worldwide public health problem, as it is associated with different comorbidities, such as dyslipidemias, type 2 diabetes mellitus, and arterial hypertension.1 In Brazil, the Family Budget Survey (Pesquisa de Orçamentos Familiares, POF 2008–2009) indicated the presence of obesity in 14.3% of children aged 5 to 9 years, while 33.5% were overweight.2 However, it is important to consider the body fat distribution, since it plays a crucial role in the development of cardiometabolic risk.3
There are different techniques to evaluate body fat, with dual energy X-ray absorptiometry (DXA) being considered a reference method to evaluate central adiposity in children of all ages, since it estimates the amount of fat in the android region.4 However, its use in epidemiological studies and clinical practice is also limited due to its high cost and complex performance, requiring simple and less expensive methods.
In this context, neck circumference (NC) has been proposed as a useful tool to identify young individuals with excess weight and cardiometabolic risk, as it is a simple, low-cost method and shows a smaller variation throughout the day compared to the waist circumference.5 However, to date, no studies have been found in the literature that evaluated the association and the ability of NC to identify excess central adiposity estimated by a reference method, such as fat content in the android region determined by DXA.
The lack of the definition of NC-specific cutoff points for Brazilian children may be a limitation to its routine use. In the literature, to the best of our knowledge, there is only one cross-sectional study with Brazilian adolescents enrolled in public schools in the city of São Paulo, Brazil, which proposed NC cutoff points to identify overweight and obesity.6 Therefore, studies using this approach at earlier age ranges are scarce.
Thus, the objective of this study was: (1) to evaluate the ability of NC to identify excess android fat; (2) to propose NC cutoff points to determine excess android fat in Brazilian children.
MethodsStudy population and designThis is a cross-sectional study, carried out with a representative sample of 8- and 9-year-old children enrolled in public and private schools in the urban area of the municipality of Viçosa, state of Minas Gerais, Brazil, from May to December 2015. The municipality of Viçosa is located in Zona da Mata Mineira, 227km from the capital city of Belo Horizonte. According to the 2010 Census, Viçosa has a land area of 299km2 and 72,244 inhabitants, of whom 93.2% live in urban areas. The per capita gross domestic product (GDP) is R$ 19391.087 (US$5272.82).
The study participants came from the Schoolchildren Health Assessment Survey (Pesquisa de Avaliação da Saúde do Escolar, PASE), a cross-sectional investigation that aimed to evaluate the cardiovascular health of this pediatric population in the municipality of Viçosa.8 In 2015, the municipality had 17 public schools and seven private ones in the urban area, attended by children aged 8 and 9 years, totalling 1464 enrolled children.
Sample calculation and sampling processThe sample was calculated using Epi Info software (version 7.2, Atlanta, GA, United States), considering the total number of students aged 8 and 9 years in the year 2015 (n=1446), a prevalence of 10.7% of obesity,9 tolerated error of 3%, a 95% confidence level, and an increase of 20% to cover losses, totalling 384 children to be studied.
The children were selected by stratified random sampling, and the sample of each school reached the proportionality of students enrolled by age and gender. The children's selection was performed by simple random draw until the number needed for each school was reached.
After the selection, a telephone contact was made with the children's parents or guardians, inviting them to participate in the study. The study aim and methodology were explained to the children's parents or guardians, the first meeting was scheduled, and those who agreed to participate signed the free and informed consent form after receiving explanations about each step of the study.
Children who had any health problems that altered their nutritional status or body composition (physical, cognitive, or multiple deficiencies, thyroid disorders, etc.), as well as those with chronic use of medications that interfered with glucose and/or lipid metabolism (corticosteroids, statins, hypoglycemic agents, etc.), and those using vitamin or mineral supplements during the study or in the previous three months (vitamin D and zinc supplementation) were not included, as well as cases in which it was not possible to contact parents or guardian after three attempts. A pilot study was carried out in February 2015 with 10% of the sample, including children aged 8 and 9 enrolled in a randomly selected public school, which were not part of the final study sample. Through the pilot study, it was possible to test the application of the questionnaires.
Demographic, socioeconomic, and lifestyle dataA semi-structured questionnaire containing socioeconomic and demographic information, such as age, gender, type of school (public or private), and per capita income (categorized according to the median of the total sample, equivalent to R$ 500.00 - US$ 135.96) was applied.
A questionnaire on lifestyle was applied to estimate the screen time in hours per day (time spent sitting for long periods in front of the television, video game, or computer). Sedentary behavior was classified as screen time >2h/day.10
Anthropometry and body compositionData collection was performed in an appropriate environment by a trained team member, with barefoot volunteers, who were wearing light clothing. The weight was measured on an electronic digital scale, with a capacity of 150kg and a precision of 0.1kg (Tanita® Model Ironman BC 553; Tanita Inc., Arlington Heights, IL, United States) and stature was determined using a stadiometer, divided into centimeters and subdivided into millimeters (Alturexata®, Belo Horizonte, MG, Brazil).
Using body weight and height data, the body mass index (BMI) was calculated, and the BMI cutoff point for age (BMI/A) Z-scores were used for the classification of the children's nutritional status, as established by World Health Organization.11 To assess the mothers’ nutritional status, the criteria for BMI classification recommended by the World Health Organization were used.12 Overweight and obese children and mothers were grouped in the excess weight group.
The NC was evaluated with the child standing upright, with the head in the horizontal plane of Frankfurt, using an inextensible measuring tape (TBW®, São Paulo, Brazil), just below the laryngeal prominence in the neck, perpendicular to the largest neck axis. Minimum pressure was exerted to allow full contact of the tape with the skin. The measurement was performed in duplicate, considering the average of the two measurements. For the classification, the authors used the cutoffs obtained from the receiver operating characteristic (ROC) curves with the best values of sensitivity, specificity, and predictive values for excess android fat, according to gender.
The percentage of fat in the android region was determined by dual energy X-ray absorptiometry (DXA; Lunar Prodigy Advance, GE Medical Systems Lunar – Milwaukee, WI, United States) using the equipment software for the analysis of body composition. The android fat was identified in the region between the ribs and the pelvis, with the upper demarcation being made at 20% of the distance of the iliac crest and the neck, whereas the lower demarcation was made above the pelvis.4 No cutoff points were found in the literature for the diagnosis of elevated android fat in children. Therefore, the 85th percentile of the sample according to gender was considered as increased values, which corresponded to 34.0% and 28.9% for girls and boys, respectively.
Biochemical and blood pressure assessmentsBlood collection was performed after a 12-h fasting at the Clinical Analysis Laboratory of the Health Division of Universidade Federal de Viçosa (UFV). The samples were collected by venipuncture in appropriate tubes, centrifuged for 15min at 3500rpm, and then separated into 1.5mL-Eppendorf tubes and stored in an ultra-freezer at −80°C.
The lipid profile (total cholesterol, high-density lipoprotein [HDL-c], low-density lipoprotein [LDL-c], and triglycerides) and fasting glycemia were determined by the colorimetric enzymatic method using a commercial Bioclin® kit (Belo Horizonte, Brazil) and measured in an automatic analyzer device (BS-200 Mindray®, Nanshan, China) at the Laboratory of Clinical Analyses (LAC) of the Department of Nutrition and Health of UFV. The classification of the lipid profile components was performed according to the updated Brazilian Dyslipidemia and Atherosclerosis Prevention Guidelines.13
Fasting insulin was determined utilizing the chemiluminescent immunoassay method at the Diagnósticos do Brasil laboratory and quantified by the insulin assay (Elecsys Insulin®, Roche, Basel, Switzerland) with a detection limit of 0.200–1000μU/mL. A HOMA-IR value ≥3.1614 was used to classify insulin resistance.
A digital electronic device was used to measure blood pressure in the arm, with automatic air inflation and deflation, and cuff size that was appropriate for the patient.15 Blood pressure was assessed considering gender, age, and height percentile, also according to the classification recommended by the Brazilian Society of Cardiology.15
Statistical analysesStatistical analyses were performed using SPSS for Windows, version 23.0 (SPSS Inc., Chicago, IL, United States). The Kolmogorov–Smirnov normality test was used to determine whether the continuous quantitative variables had a normal distribution. The significance level was set at 5% for all hypothesis tests.
Descriptive analyses of the data were carried out through relative frequencies, means, (standard deviation) or medians (interquartile range). For the comparison of means or medians between two independent samples, Student's t-test or the Mann–Whitney test was performed, respectively. The association between the NC (independent variable) and android fat (dependent variable) was assessed by multiple linear regression.
The adjustment variables that constituted the final model were: gender, school type (public or private), total cholesterol, HDL-c, HOMA-IR, and maternal BMI. The final model was evaluated according to the assumptions of linearity, homoscedasticity, normality, independence, multicollinearity, and standardized residuals.
The receiver operating characteristic (ROC) curves determined the ability of NC to identify excess android fat. Additionally, NC cutoffs with better values of sensitivity (S) and specificity (Sp) were estimated, as well as positive (PPV) and negative (NPV) predictive values.
Ethical aspectsThis study was carried out in accordance with the guidelines established in the Declaration of Helsinki and approved by the Human Research Ethics Committee of Universidade Federal de Viçosa (Opinion No. 663.171/2014). It was also approved by the Municipal Secretariat of Education, the Regional Superintendent of Education, and school principals.
ResultsThe final sample consisted of 376 children, and there was a loss of 2.1% of the participants, as they did not complete all the research phases (they did not have blood collected for biochemical tests). Based on the proposed cutoff points in the ROC curves, it was observed that 20.2% (n=76) of the children had elevated NC (Table 1).
Values of neck circumference and android fat according to sociodemographic, anthropometric, biochemical, and clinical variables. Viçosa, MG, Brazil 2015.
| Variable | n (%) | Neck circumference (cm) | Android fat (%) |
|---|---|---|---|
| Total | 376 (100.0) | 27.0 (26.0; 28.5) | 14.9 (7.1; 26.4) |
| Gender | |||
| Female | 196 (52.1) | 26.7 (25.5; 28.1) | 17.1 (8.6; 20.0) |
| Male | 180 (47.9) | 27.4 (26.4; 28.5) | 9.7 (5.9; 22.7) |
| p-value | 0.001d | <0.001d | |
| Age | |||
| 8 years | 182 (48.4) | 26.6 (25.5; 28.0) | 13.1 (6.8; 23.9) |
| 9 years | 194 (51.6) | 27.5 (26.2; 28.5) | 16.30 (7.8; 27.8) |
| p-value | <0.001d | 0.101 | |
| School type | |||
| Public | 266 (70.7) | 27.2 (2.0) | 12.5 (6.9; 25.7) |
| Private | 110 (29.3) | 27.4 (1.9) | 19.3 (8.7; 27.1) |
| p-value | 0.448 | 0.018d | |
| Per capita income | |||
| ≥R$ 500.00 | 191 (50.8) | 27.4 (1.9) | 17.0 (7.3; 27.2) |
| 185 (49.2) | 27.1 (2.0) | 12.8 (7.1; 24.6) | |
| p-value | 0.085 | 0.115 | |
| Screen time/day | |||
| >2h | 178 (47.3) | 27.3 (26.0; 28.5) | 15.5 (7.3; 27.1) |
| ≤2h | 198 (52.7) | 27.0 (25.7; 28.1) | 13.2 (7.1; 25.6) |
| p-value | 0.119 | 0.377 | |
| Excess weight | |||
| Yes | 123 (32.7) | 29.2 (1.6) | 31.3 (9.7) |
| No | 253 (67.3) | 26.3 (1.2) | 11.1 (6.7) |
| p-value | <0.001c | <0.001c | |
| Neckcircumferencea | |||
| Increased | 76 (20.2) | 29.9 (29.0; 31.0) | 32.7 (25.3; 39.3) |
| Adequate | 300 (79.8) | 26.5 (25.5; 27.5) | 10.5 (6.2; 19.8) |
| p-value | – | <0.001d | |
| Androidfatb | |||
| ≥p85 | 73 (19.4) | 29.5 (28.5; 30.9) | 35.9 (32.2; 43.3) |
| 303 (80.6) | 26.5 (25.5; 27.7) | 10.5 (6.3; 18.6) | |
| p-value | <0.001d | – | |
| Maternal excess weight | |||
| Yes | 168 (57.3) | 27.8 (2.0) | 18.3 (8.4; 30.8) |
| No | 125 (42.7) | 26.5 (1.8) | 11.0 (6.2; 19.9) |
| p-value | <0.001c | <0.001d | |
| Total cholesterol | |||
| ≥170mg/dL | 86 (22.9) | 27.5 (1.9) | 20.5 (7.5; 29.4) |
| <170mg/dL | 289 (77.1) | 27.2 (1.9) | 12.8 (7.1; 24.1) |
| p-value | 0.278 | 0.011d | |
| HDL-c | |||
| ≤45mg/dL | 131 (34.9) | 27.6 (2.1) | 18.4 (8.0; 32.1) |
| >45mg/dL | 244 (65.1) | 27.1 (1.8) | 12.9 (6.9; 23.0) |
| p-value | 0.006c | 0.005d | |
| LDL-c | |||
| ≥110mg/dL | 58 (15.5) | 27.7 (1.9) | 22.0 (12.8) |
| <110mg/dL | 316 (84.5) | 27.2 (1.9) | 16.8 (12.0) |
| p-value | 0.064 | 0.003c | |
| Triglycerides | |||
| ≥75mg/dL | 176 (46.9) | 27.7 (2.1) | 19.9 (8.2; 30.7) |
| <75mg/dL | 199 (53.1) | 26.9 (1.7) | 10.6 (6.5; 19.8) |
| p-value | <0.001c | <0.001d | |
| HOMA-IR | |||
| ≥3.16 | 9 (2.4) | 30.1 (1.1) | 35.6 (13.2) |
| <3.16 | 362 (97.6) | 27.2 (1.9) | 17.3 (11.9) |
| p-value | <0.001c | <0.001c | |
| Blood pressure | |||
| Increased | 25 (6.7) | 29.1 (1.8) | 29.0 (13.6) |
| Adequate | 350 (93.3) | 27.1 (1.9) | 16.9 (11.8) |
| p-value | <0.001c | <0.001c | |
HDL-c, high density lipoprotein; LDL-c, low density lipoprotein; HOMA-IR, homeostatic model assessment for insulin resistance.
Data presented as mean (standard deviation) or median (interquartile range).
In the general sample, the NC and the percentage of android fat showed median values of 27.0cm and 14.9%, respectively. Higher percentages of android fat were observed in female children, those from private schools, with excess weight, undesirable lipid profiles, insulin resistance, high blood pressure, and maternal excess weight. The same results were found for the highest NC values, except for school type, total cholesterol, and LDL-c concentrations (Table 1).
In the final multiple linear regression model, a positive association was observed between NC and android fat percentage. An increase of 1cm in NC was associated with a 2.94% increase in android fat, when adjusted for gender, school type, total cholesterol, HDL-c, HOMA-IR, and maternal BMI (Table 2).
Association between the neck circumference (independent variable) and the percentage of android fat (dependent variable) in children. Viçosa, MG, 2015.
| Variable | β (95% CI) | p-value |
|---|---|---|
| Neck circumference (cm) | 2.94 (2.41; 3.47) | <0.001 |
| Female gender | 5.31 (3.33; 7.29) | <0.001 |
| Private school | 2.95 (0.75; 5.15) | 0.009 |
| Total cholesterol (mg/dL) | 0.08 (0.04; 0.11) | <0.001 |
| HDL-c (mg/dL) | −0.16 (−0.27; −0.05) | 0.004 |
| HOMA-IR | 3.05 (1.78; 4.33) | <0.001 |
| Maternal BMI (kg/m2) | 0.29 (0.10; 0.47) | 0.002 |
Multiple linear regression; 95% CI, 95% confidence interval; HDL-c, high density lipoprotein; HOMA-IR, homeostatic model assessment for insulin resistance; BMI, body mass index.
Adjustment by gender, school type, serum concentrations of total cholesterol, HDL-c, HOMA-IR, and maternal BMI.
The analysis of the ROC curve showed that NC was able to identify excess android fat in girls (AUC: 0.909, 95% CI: 0.859, 0.945) and boys (AUC: 0.938, 95% CI: 0.892, 0.968). The proposed cutoff points for female (28.3cm) and male individuals (28.6cm) showed satisfactory S values (female: 76.1%, male: 85.2%), Sp (female: 92.7%, male: 87.6%) and predictive values (female: PPV, 76.1%; NPV, 92.7%; male: PPV, 56.4%; NPV, 97.1%; Fig. 1).
Areas under the receiver operating characteristic (ROC) curve (AUC) and cutoff points for neck circumference with the best sensitivity, specificity, and predictive values for excess android fat, according to gender. Viçosa, MG, 2015.
AUC, area under the curve; 95% CI, 95% confidence interval; S, sensitivity; Sp, specificity; PPV, positive predictive value; NPV, negative predictive value.
To date, this is the first Brazilian study carried out with a representative sample of children that demonstrated the ability of NC to identify excess android fat. Moreover, NC showed a direct association with android fat, regardless of gender, school type, serum total cholesterol, HDL-c, HOMA-IR, and maternal BMI. It should be noted that the proposed cutoff values showed satisfactory S, Sp, and predictive values, making it possible to use NC in epidemiological studies, cardiometabolic risk screenings, and ambulatory care.
The use of NC in adults has been extensively studied, with a direct association being observed with visceral adipose tissue and HOMA-IR in obese individuals.16 Furthermore, a population-based study with Brazilian adults has shown that NC can be used to identify metabolic syndrome and insulin resistance.17
In this sense, the use of the NC in the pediatric population becomes important, and most studies in this population have compared it with doubly indirect methods used to estimate adiposity, such as BMI,18 waist circumference,19 and waist-to-height ratio.20
In individuals aged 9–13 years from Greece, NC was directly associated with serum triglycerides and insulin levels, HOMA-IR, and blood pressure; and inversely to serum levels of HDL-c, quantitative insulin sensitivity check index (QUICKI), and fasting glucose-insulin ratio (FGIR). The same study demonstrated that other anthropometric measures used in children and adolescents, such as BMI Z-score, waist and hip circumference, waist-to-height ratio, and waist-to-hip ratio, showed associations with cardiometabolic risk markers similar to NC.21
NC is considered an alternative to identify central adiposity, as it has some advantages in relation to waist circumference: good inter- and intraobserver agreement; not influenced by the time of measurement (pre-prandial and post-prandial periods); and easier to measure, since it does not require the person being assessed to wear light clothing, and thus is more socially acceptable.19 However, there is no international consensus on cutoffs to be used in children.
There are NC cutoffs that have been proposed based on ROC18 curves and percentiles22 for children and adolescents according to gender and age in different locations. However, most of them are cutoff points capable of determining overweight/obesity through BMI.18,22 Therefore, the present study proposed NC cutoff points that can be used to identify excess android fat through DXA, which is capable of estimating central adiposity, a method considered as reference.23
In a cross-sectional study with Brazilian adolescents from Campinas, in the state of São Paulo, the NC cutoffs that were suggested to determine insulin resistance were 32.0 and 30.3cm, for prepubertal girls and boys, respectively.19 The cutoff points proposed in a cross-sectional study carried out by Nafiu et al.18 to identify excess weight in American children aged 8 and 9 years were 29.0 and 30.5cm (boys), 27.9 and 29.3cm (girls), respectively, being close to the values found in the present study. Therefore, it is recommended to validate the cutoff points proposed in this study for other populations, aiming to identify excess central adiposity and other cardiometabolic risk factors.
Studies that address the presence of excess central adiposity in the pediatric population are of great relevance, since the anthropometric measures that estimate central adiposity showed a greater association with the cardiometabolic risk, in relation to the BMI in children.24 The fat in the android region comprises the visceral adipose tissue, which is more lipolytic compared to the peripheral regions. A greater hepatic release of LDL-c, triglycerides, and other fatty acids in the portal circulation, stimulation of hepatic gluconeogenesis, and hepatic insulin uptake inhibition can be observed, causing hyperinsulinemia and insulin resistance.25
Considering the high prevalence of excess weight, undesirable lipid profile, and sedentary behavior in this sample and other similar studies,26,27 it becomes necessary to attain an early diagnosis of excess central adiposity in children. It is known that all these alterations can persist in adult life, in addition to being related to the atherogenic process and cardiac damage, which may begin as early as during childhood.28,29 Moreover, the evaluation of the maternal nutritional status is important to identify the excess central adiposity in children, as the mothers and their children share genetic, environmental (food availability at home), and behavioral (dietary and lifestyle habits) factors.30
The positive aspects of this study are the fact that the anthropometric evaluation was performed by a single researcher, which contributed to reduce measurement bias; and the fact that the sample consisted exclusively of children, which minimizes the possible hormonal influences of adolescence on body composition. The ROC curve analysis was not stratified by age because of the physiological similarity between 8- and 9-year-old children. Although DXA is unable to differentiate between types of adipose tissue, the fat in the android region assessed through this test is strongly correlated to visceral adipose tissue in children. Regarding limitations, note the lack of reference values to classify android fat in children, which compelled the authors to use the 85th percentile of the sample according to gender. Considering this, the authors suggest studies that propose cutoff points for android fat and NC in all pediatric age groups, aiming to establish an international consensus in the future.
In conclusion, NC is a measurement capable of identifying excess android fat in Brazilian children. The proposed cutoff points can be used in population studies, screening, and outpatient care, provided they are validated for the pediatric population to which they will be applied. Thus, NC can be part of the evaluation routine of children's health status, as it is a simple and low-cost measure, helping in the early identification of excess central adiposity.
FundingThis study was funded by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) (process no.: 478910/2013-4).
Conflicts of interestThe authors declare no conflicts of interest.
The authors would like to thank the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) for their financial support, Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) for the study grant, Quibasa/BioClin for the donation of biochemical kits, and the children and their parents for their participation in the study.
Please cite this article as: Filgueiras MS, Albuquerque FM, Castro AP, Rocha NP, Milagres LC, Novaes JF. Neck circumference cutoff points to identify excess android fat. J Pediatr (Rio J). 2020;96:356–63.