To describe the management, to compare treatment at initial referral vs. during specialized follow-up, and to describe outcomes of children with functional constipation (FC) referred to a Brazilian tertiary care center.
MethodsRetrospective study, including children (4–18 years) with FC followed at a single center from 2006 to 2019. Demographics, treatments, time of follow-up, and outcomes were analyzed. The management of FC followed an institutional protocol.
Results104 patients were identified, 79 were eligible and included in the analysis: 59% male, mean age at referral was 6.4 years, and mean duration of symptoms was 4.4 years. There were significant changes in the therapy(ies) used at the time of referral compared to during follow-up, with a noticeable increase in the frequency of the use of polyethylene glycol, enemas, magnesium hydroxide, and bisacodyl; 5.1% received trans-anal irrigation, and 3.8% underwent surgery. Outcomes were favorable in more than half of the cases: 31% improved; 19.5% had complete resolution and 2.5% were transferred back to primary care. Symptoms remained unchanged in 30.4%, and no patients experienced worsening of symptoms. The mean duration of follow-up was 2.8 years. When comparing patients with favorable vs. unfavorable outcomes, the authors did not identify significant differences in gender, age, therapies used, duration of symptoms, or length of follow-up.
ConclusionsChildren with FC are often referred to specialized care not receiving optimal therapy. Many patients whose FC was labeled “refractory” may be treated successfully with a well-established plan of care, and do not truly present intractable constipation.
Constipation is among the most prevalent chronic health problems reported in the pediatric population globally.1 Functional constipation (FC) is by far the most common etiology: it is estimated that FC affects more than 10% of children worldwide.2,3 Rome IV criteria define FC in children (developmental age ≥ 4 years) in the presence of two or more of the following criteria, for at least one month: (1) two or fewer defecations per week in the toilet; (2) at least one episode of fecal incontinence per week; (3) retentive behavior; (4) painful or hard bowel movements; (5) detection of large fecal mass in the rectum; (6) stools of large diameter that may obstruct the toilet.4 There are also well-defined and overall similar criteria for FC diagnosis in children (toilet-trained and non-toilet-trained) younger than 4 years of age.5
Early diagnosis and management of FC with good control of symptoms within three months of onset, is considered a key factor for long-term prognosis6,7: it is estimated that it provides medication-free recovery within 6 months in around 80% of cases while delaying treatment is associated with a significantly lower laxative-free recover within that time range – less than one-third of patients.7,8
In 2014, the joint guideline from the North American and the European Societies for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN and ESPGHAN, respectively) defined “intractable constipation” as the persistence of constipation which fails to respond to at least 3 months of adequate optimal conventional treatment.8 Children with constipation and unsatisfactory response to first-line optimal therapy should be referred to specialized care,6 and evaluated for underlying medical conditions.8 This group of children carry a higher probability of having slow colonic transit and outlet obstruction,9 and may require escalation in therapy and specialized investigations, including anorectal manometry to assess for the presence of the rectoanal-inhibitory reflex (RAIR), colonic manometry, a 2- to 4-week trial of avoidance of cow's milk protein followed by a challenge if there is a response, and consideration for surgical treatment for antegrade enemas.8
In the long term, up to 25–50% of children with FC will not recover the ability to evacuate spontaneously without laxatives, still present retentive incontinence, and/or do not respond to maximum doses of laxatives or rectal therapy.6,8,10,11 Pediatric patients with FC who are referred to tertiary care possibly represent a severe end of the spectrum – it has been reported that only about half of children with refractory FC recover after 5 years of follow-up.8,12,13 In this context, the goals of the present study were to describe the management, to compare treatment at initial referral vs. during specialized follow-up, and to describe outcomes of children with functional constipation (FC) referred to a Brazilian tertiary care center.
MethodsStudy populationThis study was a retrospective cohort study assessing children followed at a Pediatric Gastroenterology clinic in a university-affiliated hospital (tertiary care), from June/2006 to April/2019. Children aged 4 to 18 years, with the diagnosis of FC according to the Rome IV Criteria4 were eligible. Patients who were found to have intractable constipation were investigated appropriately – and only patients whose constipation could not be fully explained by another medical condition, appropriately fulling the criteria for FC were included.
All methods were carried out following our institution's Research Ethical Board (REB) guidelines and regulations, after REB approval.
Data extraction and analysisPatients’ charts were reviewed, and data were extracted using a data-extraction form. Data collected included: age, gender, weight, height, body mass index (BMI), duration of symptoms, medications in use at referral, medications used during follow-up, response to treatment, and duration of follow-up.
Response to therapy was defined according to the presence of three criteria (all must be present): (1) frequency of evacuation – greater than or equal to three times a week; (2) stool consistency – soft, corresponding to types 3 to 5 in the “Bristol stool scale”14; and (3) absence of retentive fecal incontinence.
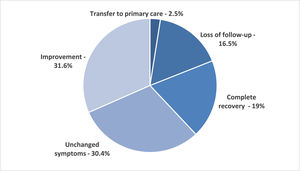
For descriptive analysis, outcomes were categorized as it follows: (1) Worsening – if any symptom had become more severe than at initial assessment; (2) Unchanged symptoms – no significant variation as compared to the initial assessment; (3) Improvement – relative response, with no retentive fecal incontinence, but without fulfilling the other above-mentioned criteria of response, and patient remained on therapy and followed at tertiary care; (4) Transfer to primary care – response to treatment, with significant improvement allowing follow-up to be transferred back to primary care; (5) Complete recovery – response to treatment, followed by resolution symptoms allowing weaning of laxatives, with no relapse and no further need for any type of follow up for this specific complaint; (6) Loss of follow-up.
Statistical comparisons were analyzed using Fisher´s exact test (categorical variables) and the Mann-Whitney U-test (continuous variables). Statistical tests were 2-sided, with a p-value < 0.05 considered statistically significant. Analyses were performed using Excel for Windows and software R 3.2.6 (R Core Team).
Institutional protocol for management of FCInternal guidelines for the management of FC follows a strict therapeutic plan based on the involvement of the family establishing a close partnership with the medical team, shared actions and medical decisions, and well-defined pre-established goals: (1) discussion with the family on the feasibility of acquisition and use of the medication; (2) disimpaction; (3) maintenance therapy using high doses of oral laxatives; (4) use of dietary fiber based on wheat (bran and grains); (5) progressive and slow “replacement” of the laxative by dietary fiber if possible; (6) strict compliance, initially with biweekly follow-up visits and/or telephone or virtual follow-up, as needed.
Selected patients are treated with trans-anal irrigation (TAI)15 following a predefined bowel management program: three rectal irrigations were performed daily for 3 consecutive days using a Foley catheter with an inflated balloon, while the patient remained (when feasible) in a genupectoral position to maximize the distance reached by the irrigation. The irrigations were done according to a previously described regimen,16 in which the first irrigation of the day contained sodium phosphate (66 mL diluted in 1 liter of saline solution for children aged 4–12 years, and 133 mL diluted in 1 liter of saline solution for children 12 years or older), while the afternoon and the nocturnal irrigations consisted of saline alone (1 l for all age groups).
Surgical treatment with a Malone Antegrade Continence Enema (MACE) is used for the management of intractable FC - as recognized by the 2014 NASPGHAN and ESPGHAN guidelines.8 Patients are only considered surgical candidates after optimal treatment and exclusion of organic diseases – including celiac screening, TSH/T4, and evaluation for Hirschsprung's disease (anorectal manometry and/or rectal biopsy), anatomical malformations (barium enema), and spinal malformations (MRI). Our center experience comparing clinical management or appendicostomy for patients with Refractory functional constipation has been previously published.17
Despite recognizing that biofeedback might be an effective tool for the management of FC resistant to medical treatment in children, especially retentive fecal incontinence,18 this modality of treatment is unfortunately not available for the management of pediatric FC at our institution.
ResultsIn the study period, 104 patients were referred to the study's Pediatric Gastroenterology clinic having the label of “refractory functional constipation”. Twenty-three patients were excluded from the study's analysis due to incomplete data, thus, data from 79 patients were analyzed: 59% were male, and the mean age at first visit was 6.4 years, with a mean duration of symptoms of 4.4 years. Mean z-scores for weight-for-age age and height-for-age were -0.29 and -0.37, respectively – most patients had a normal BMI, while 7 patients were overweight and 2 were obese.
All patients had received some therapy before the referral, however, surprisingly, on the occasion of the first visit, 31.6% (25/79) of patients were not using any medical therapy. One patient was referred after MACE. At referral, the most common therapies in use were polyethylene glycol (PEG), enemas, and lactulose - used in 27.8%, 24%, and 22.7% of cases, respectively. PEG with or without electrolytes given orally, recommended as the first-line treatment for children,8 was by far the most common laxative used during follow-up – in 91.1% (72/79) of patients. There was a noticeable change in the pattern of therapies, with a statistically significant increase in the frequency of use of PEG, enemas, magnesium hydroxide, and bisacodyl. Many of the patients required more than a single agent. As expected, the number of patients requiring combined therapies was significantly higher during tertiary care follow-up, as compared to at the time of referral: 11% were using two agents and 21.5%, three or more at referral, vs. 19.1% and 48.1%, respectively during follow up. The detailed relative distribution of therapy in use at the time of referral and during tertiary care follow-up and inferential analyses are summarized in Table 1.
Comparison between treatment at referral and tertiary care follow-up.
NS, non-significant. Fisher's exact test was performed. Excluded one patient who had undergone surgery prior to referral.
Fifty-five percent of patients required rectal therapy (enemas). Treatment with TAI was reserved to a selected group of patients (5.1%) – after adequate training of family (and patients), this treatment was well tolerated, and no complications were reported. Three patients underwent surgical treatment (MACE) – representing 3.8% of patients (3/78* - as one patient was treated surgically before referral).
The mean duration of follow-up was 2.8 years. Outcomes following the pre-defined categories were overall favorable in 53.1% of patients: 31.6% experienced improvement of symptoms while remained on treatment and tertiary care follow up; 19% had complete recovery and were weaned off therapy, and 2.5% were transferred back to primary care still requiring some follow-up and treatment for their constipation. In 30.4% of cases, symptoms remained unchanged despite optimal therapy. None of the patients experience worsening symptoms. There was a 16.5% (13/79) rate of loss of follow-up. The distribution of outcomes according to categories is summarized in Fig. 1.
Outcomes by category at the end of the follow-up period at tertiary care level.
Mean duration of follow-up was 2.8 years. Response to therapy was defined by the presence of all three criteria: (1) frequency of evacuation greater than or equal to three times a week; (2) soft stool consistency corresponding to types 3–5 in the “Bristol stool scale”; and (3) absence of retentive fecal incontinence. Definitions: Transfer to primary care – response to treatment, with significant improvement and concerns for severity allowing follow-up to be transferred back to the primary care level; Improvement – relative response, with no retentive fecal incontinence, but without fulling the other criteria of response to treatment as defined above, and patient remained on follow-up at tertiary care; Complete recovery – response to treatment, followed by resolution symptoms allowing weaning of laxatives, with no relapse and no further need for follow up for this specific complaint; and Unchanged symptoms – no significant variation in symptoms severity. Worsening was defined if symptoms became more severe than at the initial assessment, but there were no observations in this category.
When patients with favorable outcomes (improvement, recovery, or transfer to primary care) were compared to those whose symptoms remained unchanged, the authors did not find any statistically significant difference between the gender (p = 0.43), age at referral (p = 0.46), duration of symptoms before to referral (p = 0.42) or length follow-up at tertiary care (p = 0.40). The mean length of follow-up for these groups of patients was 2.6 and 3.1 years, respectively, while the median was 2.1 years in both groups. The comparative data according to the category of outcomes is summarized in Table 2.
Comparison between patients with favorable vs. unfavorable outcomes.
Fisher´s exact test or chi-square for categorical variables,
Mann-Whitney U test for continuous variables)
Favorable outcomes = improvement, recovery or transfer to primary care
Unfavorable = patients whose symptoms remained unchanged
Patients who lost follow-up (13) not included in the analysis.
After initiating follow up at the study's center and treatment following established institutional guiding principles for the management of FC, the authors found that slightly over half of the patients previously labeled as having “refractory functional constipation” and referred to tertiary care for that reason, had a favorable outcome over a follow-up period of 2.8 years. The authors noticed however that an impressive percentage of these patients (more than 30%) was not using any medical therapy for the management of constipation at the time of the first visit with a specialist. All the patients referred to the study's institution had previously received some form of therapy, over a mean duration of more than 4 years of symptoms. The present study's data raises the concern that possibly many of these children did not truly present refractory constipation and might have not received optimal treatment or been compliant to treatment. On the other hand, perhaps some of these children should have been referred earlier, as the duration of symptoms was relatively long, and children with intractable constipation should be referred to specialized care for investigation and further management. It has been previously reported that among patients who are seen by a pediatric gastroenterologist with the chief complaint of constipation, approximately 50% will improve allowing laxatives to be weaned off after 6–12 months, while 40% will remain symptomatic while using laxatives, and 10% will remain well only while taking laxatives, however over longer periods of follow up, the recovery rates increase to 50 and 80% after 5 and 10 years, respectively.8
In the present study's population, there was a discrete male predominance, and gender was not found to be a factor determinant of outcome. In a review of the literature, no consensus has been found regarding a specific gender predominance in pediatric constipation.19–21 Obesity has been associated with poor response to therapy and has also been implicated as a risk factor for constipation.22 But in the present study, only two participants were obese, not allowing this association to be further explored. The duration symptoms before referral to specialized care was relatively long, which may have contributed to the challenge managing these patients. However, when comparing patients with favorable vs. unfavorable outcomes the authors did not find a statistically significant difference in the duration of symptoms or age of patients at referral.
When comparing the treatment in use at the time of referral vs. during tertiary care management, the authors could see a clear change in the line of treatment: notably, there was a 3.2-fold increase in the use of PEG, which is currently considered the first choice of therapy according to NASPGHAN-ESPGHAN guidelines, as it was shown to be most effective pharmacologic treatment.8 One main issue that the authors face in treating patients with PEG in Brazil relates to financial aspects – this medication is not currently covered by the Brazilian public health care system, and the treatment may be relatively costly when treating patients with unfavorable socioeconomic status, especially when higher doses are needed.
Lactulose, also often used in the study's cohort of patients, is considered an acceptable alternative for the treatment of pediatric constipation (according to the same NASPGHAN-ESPGHAN guidelines)8 and it is included in the list of medications distributed by the public health system. However, in reality, this medication is not always reliably provided. Slightly under one-fourth of the study's cohort received lactulose as the long-term therapy for constipation. In ‘our reality, the choice between PEG and lactulose, in many instances rely on family and patients’ preferences, as the cost is comparable/ similar, and even though the authors try to offer a prescription for lactulose coverage by the public health care system, it is often the case that there is a shortage of the medication and patients are unable to get the medication free of cost.
Magnesium Hydroxide (“milk of magnesia”) is among the most used oral laxatives for the treatment of pediatric constipation,8,23 but it is less effective than PEG and lactulose, and therefore, not considered a first-choice medication.8 Although it is also not covered by the public health care system in Brazil, its monthly cost is significantly lower than the cost of PEG or lactulose. At our center, we consider the use of magnesium hydroxide as an acceptable adjuvant therapy – the reason why more than one-third of patients received it during long-term follow-up – but the authors do not recommend its use as a single agent to treat pediatric constipation.
Another significant difference noticeable in the management of constipation at our center as compared to management at referral was that the authors often used Bisacodyl as adjuvant therapy. For decades, the premise was to avoid stimulant laxatives, such as bisacodyl, senna, and sodium picosulfate, in the management of pediatric constipation – the standard therapy being osmotic laxatives, such as PEG, lactulose and magnesium hydroxide.8,24 However, for many years, the use of bisacodyl in the adult population has been supported by data on its effectiveness and safety,25,26 and recent data have demonstrated that also bisacodyl seems to be effective, well-tolerated, and not associated with complications or development of tolerance to the medication also the pediatric population, and therefore, it should be considered as adjuvant therapy for the management of children functional constipation refractory to conventional therapy.27
When other forms of medical treatment are exhausted, TAI is a non-surgical alternative: it is overall well-tolerated and safe approach in children with long-term functional constipation and retentive fecal incontinence, which should be considered in selected cases, and may spare these patients from needing surgery.15,28
The authors reported a 16.5% lost follow-up, which is not neglectable, however, it is also not unexpected in a retrospective study of a chronic condition. There is no consensus around what is an acceptable loss of follow-up rate in a retrospective study, and often authors will include loss of follow up as an exclusion criterion – we decided to include those patients and report the rate, aswe believe it is an important finding to be disclosed. In clinical trials, where study conditions are better controlled, it is generally accepted that a loss under 5% leads to little bias, while a loss greater than 20% poses threats to the study validity.29,30
Some of the limitations of the present study include the well-known limitation intrinsic to retrospective observational studies, the need to exclude patients from analyses because of missing data and loss of follow-up – which can introduce bias in case of imbalance, the lack of a description on the duration of treatment, and frequency of use of the stimulant laxatives.
In conclusion, our study highlight that most of the patients improved using mainly standard pharmacological measures, suggesting that the main issue before referral might have been a failure in the overall approach, rather than a therapeutic failure per se. Over half of children and adolescents referred to the study's tertiary care center for functional constipation labeled as having “refractory constipation” had favorable outcomes even after lingering symptoms for a relatively long time (years): approximately one-third of patients improved but still required some form of follow up for constipation, while close to one-fifth of patients recovered completely and were weaned off laxatives. There was a relatively high rate of loss of follow-up, reflecting the challenges of compliance faced in the management of this chronic condition. It seems that many children with FC labeled “refractory” at primary care may be treated successfully with a well-established plan of care, and do not truly present intractable constipation.
CRediT authorship contribution statementGiovanna Roberta Camargo de Campos: Data curation, Conceptualization, Formal analysis, Writing – original draft. Natascha Silva Sandy: Formal analysis, Writing – original draft, Writing – review & editing. Elizete Aparecida Lomazi: Formal analysis, Writing – review & editing. Maria Angela Bellomo-Brandao: Supervision, Formal analysis, Writing – review & editing.