To study fructose malabsorption in children and adolescents with abdominal pain associated with functional gastrointestinal disorders. As an additional objective, the association between intestinal fructose malabsorption and food intake, including the estimated fructose consumption, weight, height, and lactulose fermentability were also studied.
MethodsThe study included 31 patients with abdominal pain (11 with functional dyspepsia, 10 with irritable bowel syndrome, and 10 with functional abdominal pain). The hydrogen breath test was used to investigate fructose malabsorption and lactulose fermentation in the intestinal lumen. Food consumption was assessed by food registry. Weight and height were measured.
ResultsFructose malabsorption was characterized in 21 (67.7%) patients (nine with irritable bowel syndrome, seven with functional abdominal pain, and five with functional dyspepsia). Intolerance after fructose administration was observed in six (28.6%) of the 21 patients with fructose malabsorption. Fructose malabsorption was associated with higher (p<0.05) hydrogen production after lactulose ingestion, higher (p<0.05) energy and carbohydrate consumption, and higher (p<0.05) body mass index z-score value for age. Median estimates of daily fructose intake by patients with and without fructose malabsorption were, respectively, 16.1 and 10.5g/day (p=0.087).
ConclusionFructose malabsorption is associated with increased lactulose fermentability in the intestinal lumen. Body mass index was higher in patients with fructose malabsorption.
Pesquisar a má absorção de frutose em crianças e adolescentes com dor abdominal associada com distúrbios funcionais gastrintestinais. Como objetivo adicional, estudou-se a relação entre a má absorção intestinal de frutose e a ingestão alimentar, inclusive a estimativa de consumo de frutose, peso e a estatura dos pacientes e a capacidade de fermentação de lactulose.
MétodosForam incluídos 31 pacientes com dor abdominal (11 com dispepsia funcional, 10 com síndrome do intestino irritável e 10 com dor abdominal funcional). O teste de hidrogênio no ar expirado foi usado para pesquisar a má absorção de frutose e a fermentação de lactulose na luz intestinal. O consumo alimentar foi avaliado por registro alimentar. Foram mensurados também o peso e a estatura dos pacientes.
ResultadosMá absorção de frutose foi caracterizada em 21 (67,7%) pacientes (nove com síndrome do intestino irritável, sete com dor abdominal funcional e cinco com dispepsia funcional). Intolerância após administração de frutose foi observada em seis (28,6%) dos 21 pacientes com má absorção de frutose. Má absorção de frutose associou-se com maior produção de hidrogênio após ingestão de lactulose (p<0,05), maior consumo de energia e carboidratos (p<0,05) e maior valor de escore z de IMC para a idade (p<0,05). As medianas da estimativa de ingestão diária de frutose pelos pacientes com e sem má absorção de frutose foram, respectivamente, 16,1 e 10,5g/dia (p=0,087).
ConclusãoMá absorção de frutose associa-se com maior capacidade de fermentação de lactulose na luz intestinal. O índice de massa corporal foi maior nos pacientes com má absorção de frutose.
Chronic abdominal pain occurs in approximately 10–20% of children and adolescents.1 Most patients have functional gastrointestinal disorders, resulting from the interaction of biopsychosocial factors.1,2 Among the factors involved in the etiology of abdominal pain associated with functional gastrointestinal disorders, individual personality traits, previous traumatic events, and coping capacity in adverse situations, in addition to visceral hypersensitivity, gastrointestinal motility abnormalities, and intestinal microbiota are noteworthy.1,2
Intestinal fructose malabsorption has been described in children3–10 and adults as a cause of abdominal pain or as a triggering factor for episodes of abdominal pain in patients with functional gastrointestinal disorders.11,12 Fructose is considered one of the most relevant fermentable carbohydrates (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols [FODMAPs]). The interest in the role of FODMAPs in functional gastrointestinal disorders has been increasingly highlighted in the literature.11,12
Unabsorbed fructose is fermented, resulting in the production of short-chain fatty acids and gases, such as hydrogen.3 The hydrogen produced in the fermentation is partially absorbed into the bloodstream and reaches the lungs, allowing its measurement in exhaled air. The diagnosis of fructose malabsorption can be made with the hydrogen breath test after administration of fructose. The result of this test depends on the fructose dose used.3–11 Lactulose can also be used in the breath test to evaluate the hydrogen production capacity and fermentation of the intestinal microbiota.13
Fructose is found as a monosaccharide in green vegetables, vegetables, fruit, and honey. It is also found in industrialized products, such as in high-fructose corn syrup. In the last 15 years, the consumption of fructose worldwide has increased concomitantly with the increase of the obesity epidemic.14,15 Excessive fructose consumption may contribute to the development of overweight and obesity, hypertension, and peripheral resistance to insulin.16
Although intestinal malabsorption of fructose may be a causal factor or associated with abdominal pain related to functional gastrointestinal disorders and its potential in influencing nutritional status, no studies that have evaluated fructose intake, intestinal fructose malabsorption, and nutritional status of children and adolescents with abdominal pain were retrieved in the literature.
The objective of this study was to evaluate fructose malabsorption and intolerance in children and adolescents with abdominal pain associated with functional gastrointestinal disorders. As an additional objective, the authors also assessed the association between intestinal fructose malabsorption and food intake, including the estimated fructose consumption, the weight and height of the patients, and the lactulose fermentation capacity through the breath test.
MethodsStudy design and sampleThis was a series of cases involving consecutively treated pediatric patients with functional abdominal pain associated with functional gastrointestinal disorders. The study was carried out at the Pediatric Gastroenterology Outpatient Clinic of Universidade Federal de São Paulo – Escola Paulista de Medicina. Upon admission, the informed consent form was signed. The project was evaluated and approved by the Research Ethics Committee of Universidade Federal de São Paulo – Hospital São Paulo.
Data were collected before 2016. All consecutively treated children and adolescents with functional abdominal pain aged 4–14 years were included. Patients with previous abdominal surgery, hiatal hernia, diabetes mellitus, hyper or hypothyroidism, previous treatment for Helicobacter pylori, and recent use of medications such as beta-adrenergics, beta-blockers, prokinetics, anticholinergics, and antisecretory drugs were not included. Furthermore, patients who had been treated with antibiotics for less than 30 days were not included.
Clinical evaluation and abdominal pain classificationAll patients were evaluated following a standardized assessment by a pediatric gastroenterologist (ACFS). Information regarding episode duration and the abdominal pain location and their association with bowel movements were obtained. Data on bowel habits (frequency of evacuations, stool shape and consistency, pain or difficulty during evacuation, and occurrence of fecal retention or incontinence behavior) were also obtained.
The collected data were used to classify patients17 into the functional dyspepsia, irritable bowel syndrome, and functional abdominal pain groups, according to the Rome III criteria.2 During the medical assessment, special attention was paid to the investigation of evidence of anatomical alteration, inflammatory processes, and metabolic or neoplastic symptoms indicating that the symptoms were not functional.2 When necessary, additional examinations were requested according to the individual needs of each patient. Individuals who did not have a clinical picture compatible with functional dyspepsia, irritable bowel syndrome, or functional abdominal pain were not included in the study.
Hydrogen breath test in exhaled airHydrogen breath tests in exhaled air with fructose and lactulose were performed at one-week intervals. Recommendations on the diet for the day before the tests included avoiding the consumption of foods containing lactose and fructose, in addition to those rich in dietary fiber and fats. The test was performed after a 12-h fasting and oral cavity hygienization with 0.05% chlorhexidine. Samples of exhaled air were collected using the GaSample system (Quintron Instrument Co. Inc. –Menomonee Falls, Wisconsin, USA).
Samples were immediately analyzed on a gas chromatograph – Quintron Microlyser, Model 12i (Quintron Instrument Co. Inc. – Menomonee Falls, Wisconsin, USA). Calibration was performed at the start of the test and repeated at the sample analysis intervals using standard gas containing 92ppm of hydrogen (White Martins – São Paulo, Brazil).18,19
An exhaled breath sample was first collected in fasting status. Subsequently, 1g of fructose/kg/weight (maximum 50g) or 10g of lactulose diluted in 150mL of water was administered orally. This procedure was supervised by one of the investigators (RKFO) to confirm complete carbohydrate intake.3 After the substrate ingestion, exhaled air samples were collected every 15min in the first hour and every 30min in the subsequent two hours. The symptoms (abdominal distension, nausea, vomiting, excessive flatulence, and diarrhea) that occurred during the breath test with fructose were recorded, as well as in the subsequent 24h, according to information obtained by telephone contact.19
Fructose malabsorptionFructose malabsorption was characterized as an increase in hydrogen concentration ≥20ppm in relation to baseline in any of the exhaled air samples collected after fructose administration.3
Fructose intoleranceFructose intolerance was characterized as the occurrence of gastrointestinal symptoms in patients with fructose malabsorption, such as abdominal pain, flatulence, abdominal distension, diarrhea, nausea, and vomiting during the 24h after fructose ingestion.3,19
Food ingestionThe three-day food registry was used to assess food intake. The children's mothers or guardians were instructed to write down all the foods the patients consumed for three consecutive days (two weekdays and one day of the weekend). The annotations consisted of a description of the meals and the foods consumed, quantified in household measures.20,21
The data obtained in the 72-h food record were analyzed using the Nut Win v. 2.5 computer software (Nutrition Support System developed by the Health Informatics Center of Universidade Federal de São Paulo – Escola Paulista de Medicina, São Paulo, Brazil). The diet's fructose content was estimated based on the United States Department of Agriculture (USDA) Food Tables.22
Weight and height measurementsWeight and height were measured as suggested by Jelliffe.23 A digital scale (Filizola Industrial Scales – São Paulo, Brazil) with a capacity of 150kg and a sensitivity of 100g was used to measure weight, and a fixed vertical anthropometer measuring up to 190cm and sensitivity of 0.1cm was used to measure height. Anthropometric indicators were calculated using the Anthro Plus software (World Health Organization – Geneva, Switzerland). Weight and height were expressed as height-for-age and body mass index (BMI)-for-age z-scores.
Statistical analysisContinuous variables were shown as mean and standard deviation or median and 25th and 75th percentiles, depending on variable distribution according to the Shapiro–Wilks test. Categorical variables were shown as percentages. The tests used were presented together with the results, considering a level of significance of 5%. The SigmaStat module of Sigma Plot 11.0 (Systat Software, CA, USA) was used.
ResultsThirty-one patients with a mean age of 9.2 years were included, of whom 14 were males. All laboratory tests performed to investigate the etiology of abdominal pain were normal. Upper digestive endoscopy was performed in six patients, and no alterations were identified in any of them.
According to Rome III criteria, 11 patients had functional dyspepsia, 10 had irritable bowel syndrome, and 10 had functional abdominal pain.
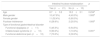
The hydrogen breath test after fructose administration showed that 21 (67.7%) of the 31 patients had fructose malabsorption. The fructose dose administered in the breath test was similar (p=0.807) in patients with (31.0±8.3g) and without (30.2±8.5g) fructose malabsorption. No difference was observed regarding age and gender in patients with and without fructose malabsorption (Table 1). In the 24h following the administration of fructose for the breath test, symptoms (fructose intolerance) were observed in six (28.6%) of the 21 patients with and in two (20.0%) of the 10 patients without fructose malabsorption (p=1.000).
Age, gender, fructose intolerance, and type of functional gastrointestinal disorder according to the presence of intestinal fructose malabsorption.
| Intestinal fructose malabsorption | p | ||
|---|---|---|---|
| Yes (n=21) | No (n=10) | ||
| Age | 8.7±3.2 | 10.2±3.1 | 0.234a |
| Male gender | 10 (47.6%) | 4 (40.0%) | 1.000b |
| Female gender | 11 (52.4%) | 6 (60.0%) | |
| Fructose intolerance | 6 (28.6%) | 2 (20.0%) | 1.000b |
| Type of functional gastrointestinal disorder | |||
| Functional dyspepsia (n=11) | 5 (45.5%) | 6 (54.5%) | |
| Irritable bowel syndrome (n=10) | 9 (90.0%) | 1 (10.0%) | 0.091c |
| Functional abdominal pain (n=10) | 7 (70.0%) | 3 (30.0%) | |
The symptoms observed in patients with fructose malabsorption and intolerance were: diarrhea (one), abdominal pain (two), and abdominal pain associated with nausea, vomiting, abdominal distension, and/or diarrhea (three). In patients without fructose malabsorption, abdominal pain was observed in two (20%) patients.
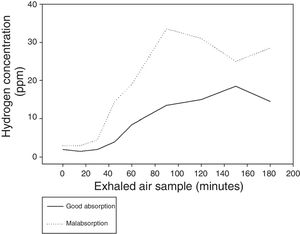
Fig. 1 shows the median hydrogen concentration in the exhaled air in the several samples of the lactulose breath test according to the presence or absence of fructose malabsorption. Table 2 demonstrates that hydrogen production after lactulose administration, an indicator of intestinal fermentation, was higher in patients with fructose malabsorption both in the first hour (hydrogen production presumably in the small intestine) and in the second and third hours of the test (production of hydrogen presumably in the colon).
Hydrogen production (ppm per minute) according to the area under the curve in the breath test with lactulose, according to the presence of fructose malabsorption.
| Breath test period | Intestinal fructose malabsorption | pc | |
|---|---|---|---|
| Yes (n=20)a | No (n=9)a | ||
| Fasting up to 60min (ppm/min)b | 503 (315; 866) | 202 (139; 272) | <0.001 |
| 60–180min (ppm/min)b | 3450 (2640; 4005) | 1290.0 (1102; 1935) | <0.001 |
| Total (fasting up to 180min) (ppm/min)b | 4159 (2940; 5066) | 1560 (1267; 2033) | <0.001 |
Estimates of food intake and height-for-age and BMI-for-age z-scores are shown in Table 3, according to the occurrence or not of intestinal fructose malabsorption. Energy and carbohydrate intake were higher in patients with fructose malabsorption. Fructose consumption was higher in the group of patients with fructose malabsorption; however, the statistical analysis did not reach significance (p=0.087).
Estimated fructose and macronutrient intake and height-for-age and BMI-for-age z-scores according to the presence of intestinal fructose malabsorption.
| Intestinal fructose malabsorption | p | ||
|---|---|---|---|
| Yes (n=21) | No (n=10) | ||
| Food registry | |||
| Fructose (g/day) | 16.1 (9.0; 27.6) | 10.5 (1.8; 16.8) | 0.087a |
| Fructose (g/kg/weight/day) | 0.58 (0.25; 0.78) | 0.28 (0.05; 0.69) | 0.091a |
| Energy (kcal/day) | 1723 (1441; 2159) | 1397 (1314; 1644) | 0.049a |
| Carbohydrates (g/day) | 258.0±65.3 | 200.0±41.7 | 0.016b |
| Carbohydrates (g/kg/weight/day) | 8.7±2.9 | 7.1±2.4 | 0.128b |
| Proteins (g/day) | 63.8±17.7 | 54.2±14.0 | 0.147b |
| Proteins (g/kg/weight/day) | 2.2±0.8 | 1.9±0.5 | 0.292b |
| Lipids (g/day) | 56.8±21.1 | 50.0±8.4 | 0.334b |
| Food fiber (g/day) | 15.3±6.4 | 12.4±2.9 | 0.193b |
| z-score | |||
| Height for age | +0.07±0.9 | −0.21±1.1 | 0.469b |
| BMI for age | +0.74±1.3 | −0.42±1.5 | 0.036b |
BMI, body mass index (kg/m2).
Table 3 shows that the height-for-age z-score was similar in patients with and without fructose malabsorption. The BMI-for-age z-score values were higher in the group with fructose malabsorption, with a statistically significant difference.
DiscussionIn the present study, fructose malabsorption was observed in 21 (67.7%) of 31 patients with abdominal pain, being more frequent in children with irritable bowel syndrome. Fructose intolerance occurred in six (28.6%) of the 21 patients with intestinal fructose malabsorption. Children and adolescents with fructose malabsorption had an intestinal microbiota with higher fermentation capacity, characterized by higher hydrogen production in the breath test with lactulose (Table 2) and higher BMI z-score values (Table 3).
Most publications show varied prevalence of intestinal fructose malabsorption in children with abdominal pain, ranging from 13% to 60%.3–10 The analysis of these articles allows speculating that part of this variability is a consequence of different techniques to perform the test in relation to the fructose dose and cutoff points used to characterize fructose malabsorption. In this context, fructose malabsorption has been considered a possible cause of abdominal pain or a triggering factor for abdominal pain episodes in patients with functional gastrointestinal disorders.11 However, the therapeutic role of a low-fructose diet in patients with abdominal pain associated with intestinal fructose malabsorption are preliminary and contradictory.3,6,9,24,25 From the clinical standpoint, the ideal situation is to establish the causal association between fructose malabsorption and the abdominal pain symptom. Theoretically, to achieve this objective, it would be necessary to obtain a favorable clinical response during the fructose elimination diet and observe the symptom recurrence after its reintroduction in the diet.
However, no article in the literature has followed such a clinical investigation procedure to associate intestinal fructose malabsorption with gastrointestinal clinical manifestations. The inclusion of a control group in the present study would allow the characterization of fructose malabsorption as a factor associated with abdominal pain; however, it would not allow establishing a causal association between fructose malabsorption and abdominal pain.
It should be noted that the present study was the only one that estimated the habitual consumption of fructose in the diet of patients with abdominal pain. The median estimate of fructose consumption in the group with intestinal fructose malabsorption (16.1g) was higher than in patients without malabsorption (10.5g); however, the difference was not statistically significant (p=0.087). This result contradicts the expectation that patients with abdominal pain secondary to fructose malabsorption could reduce the consumption of fructose as a defense mechanism to decrease the intensity of the abdominal pain.
It is noteworthy that only a portion of the patients had gastrointestinal symptoms during the breath test with fructose overload. The diet evaluation also showed higher consumption of energy and carbohydrates by patients with fructose malabsorption. The anthropometric evaluation showed that BMI values were higher in the group with intestinal fructose malabsorption. Thus, it is possible to speculate that the higher consumption of energy and carbohydrates, among which fructose, could lead to greater weight gain and body fat accumulation in the long term.26
The present results, which showed a higher BMI value in patients with fructose malabsorption, is different from those observed in a recent study27 that investigated the metabolic effect of fructose intake in 24 children, of whom 14 were obese. Of these, nine had non-alcoholic fatty liver disease and greater intestinal fructose absorption than obese patients without hepatic impairment and children with normal weight, in addition to a higher increase in glycemia, insulinemia, and serum uric acid levels after fructose ingestion. The authors concluded that obese children with liver disease absorb and metabolize fructose more effectively.27 In another study, a moderate positive correlation was observed in adult African-American individuals between intestinal fructose absorption and liver fat content.28 It should be emphasized that a direct association has not yet been definitively between fructose ingestion and overweight and other metabolic abnormalities in humans.29
In addition to fructose, other FODMAPs that are not absorbed may be involved in the genesis of gastrointestinal symptoms observed in functional gastrointestinal disorders.11,12 The interaction between gastrointestinal symptoms and intestinal microbiota has been clearly demonstrated in a study of 33 North-American children with irritable bowel syndrome. In a clinical trial, the patients received a typical American cross-over diet and low FODMAP diet.30 The clinical trial showed that, during the low-FODMAP diet, gastrointestinal symptoms were significantly reduced. Additionally, it was observed that patients with a better response had, on admission, an intestinal microbiota with greater saccharolytic capacity (Bacteroides, Ruminococcaceae, Faecalibacterium prausnitzii).30
Fructose absorption capacity was not evaluated in the patients enrolled in that clinical trial.30 The present results demonstrated that children with abdominal pain and fructose malabsorption also presented higher hydrogen production as an indicator of intestinal fermentation, both in the initial phase and in the presumably colonic periods of the breath test with lactulose (Fig. 1 and Table 2). These results indicate that the intestinal microbiota has a greater fermentation capacity and may be involved in the onset of gastrointestinal symptoms, as demonstrated by Chumpitazi et al.30 In this context, the present results clearly showed that individuals with fructose malabsorption had greater lactulose fermentation in the intestinal lumen. Therefore, it is possible to speculate that the unabsorbed fructose and its fermentation products stimulate the growth of bacteria with greater fermentation capacity.
The present study, similar to others on the subject, has several limitations. The patients included in the study comprise a convenience sample that complied with the care demand during the data collection period. Hence, the sample size was not previously estimated. The power (0.474) obtained when comparing fructose malabsorption in patients with functional dyspepsia, irritable bowel syndrome, and abdominal pain (Table 1, p=0.091) was lower than the recommended. In turn, considering the difference observed in the proportion of fructose malabsorption in functional dyspepsia (5/11) in relation to the other two groups combined (16/20), it can be estimated that it would be necessary to study approximately 40 patients in each group to demonstrate statistical significance. Moreover, it should be noted that the sample allowed the authors to find significant differences, with statistical significance, between the groups with and without intestinal fructose malabsorption. Therefore, the present results contributed to a better understanding of the association between fructose consumption and intestinal absorption, functional gastrointestinal disorders, and nutritional status.
Thus, it was concluded that intestinal fructose malabsorption was associated with greater intestinal fermentability, measured using the breath test with lactulose. Fructose malabsorption was associated with higher energy and carbohydrate consumption, which theoretically may explain, at least in part, the higher BMI-for-age values. However, future studies are necessary to evaluate the association between fructose ingestion and intestinal malabsorption, abdominal pain, overweight, and other changes in the metabolic profile.
FundingCPNq – Conselho Nacional de Desenvolvimento Científico e Tecnológico.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Ozaki RK, Speridião PG, Soares AC, Morais MB. Intestinal fructose malabsorption is associated with increased lactulose fermentation in the intestinal lumen. J Pediatr (Rio J). 2018;94:609–15.
Study carried out at Universidade Federal de São Paulo (UNIFESP), Escola Paulista de Medicina (EPM), Disciplina de Gastroenterologia Pediátrica, São Paulo, SP, Brazil.