To identify the impact of training in breastfeeding on knowledge, skills, and professional and hospital practices.
Data sourceThe systematic review search was carried out through the MEDLINE, Scopus, and LILACS databases. Reviews, studies with qualitative methodology, those without control group, those conducted in primary care, with specific populations, studies that had a belief and/or professional attitude as outcome, or those with focus on the post-discharge period were excluded. There was no limitation of period or language. The quality of the studies was assessed by the adapted criteria of Downs and Black.
Summary of dataThe literature search identified 276 articles, of which 37 were selected for reading, 26 were excluded, and six were included through reference search. In total, 17 intervention articles were included, three of them with good internal validity. The studies were performed between 1992 and 2010 in countries from five continents; four of them were conducted in Brazil. The training target populations were nursing practitioners, doctors, midwives, and home visitors. Many kinds of training courses were applied. Five interventions employed the theoretical and practical training of the Baby-Friendly Hospital Initiative. All kinds of training courses showed at least one positive result on knowledge, skills, and/or professional/hospital practices, most of them with statistical significance.
ConclusionsTraining of hospital health professionals has been effective in improving knowledge, skills, and practices.
Identificar a repercussão da capacitação em aleitamento materno sobre conhecimentos, habilidades e práticas profissionais e hospitalares.
Fontes dos dadosA busca da revisão sistemática foi efetuada nas bases MedLine, Scopus e Lilacs. Foram excluídos artigos de revisão, de metodologia qualitativa, estudos sem grupo controle, conduzidos na atenção primária, com clientelas específicas, cujos desfechos eram crença e/ou atitude profissional e trabalhos com foco no período pós-alta hospitalar. Não houve limitação quanto ao ano ou idioma, sendo realizada avaliação da qualidade dos artigos por critério adaptado de Downs & Black.
Síntese dos dadosNa busca de literatura foram encontrados 276 artigos e selecionados 37 para leitura integral, sendo excluídos 26 artigos e incluídos 6 mediante busca das referências. Foram incluídos 17 artigos de intervenção e três apresentaram boa validade interna. Os estudos foram conduzidos entre 1992 e 2010 em países de cinco continentes, sendo quatro no Brasil. O principal público-alvo das capacitações foram profissionais de enfermagem, médicos, parteiras e visitadores domiciliares. Os cursos de capacitação foram diversos, cinco intervenções empregando o treinamento teórico-prático da Iniciativa Hospital Amigo da Criança. Todas as formas de capacitação apresentaram algum resultado positivo sobre os conhecimentos, habilidades e/ou práticas profissionais e hospitalares, a maioria com significância estatística.
ConclusõesAs capacitações de profissionais de saúde que atuam em hospitais têm sido efetivas em aprimorar conhecimentos, habilidades e práticas.
The World Health Organization (WHO)1 and the Brazilian Ministry of Health2 recommend exclusive breastfeeding for six months and breastfeeding supplemented with other foods until 2 years of age or more.
However, health professionals’ lack of knowledge and skills on breastfeeding and unfavorable attitudes toward this practice3 can negatively influence the establishment and maintenance of breastfeeding,4 with lack of training representing one of the causes for the inefficiency of professional practice.5 The health professional's role is to reinterpret the scientific discourse with the clientele.6 Therefore, it is essential to have knowledge and clinical skills in breastfeeding counseling, to be able to guide and assist in breastfeeding management, when necessary.7,8
Several studies show the need for specific and periodic training in promoting, protecting, and supporting breastfeeding, aiding in the encouragement and support of breastfeeding policies and protocols in health institutions.7–9
High staff turnover – as well as lack of motivation, available resources, and time – are factors that hinder the training of the health care team.10
A review by Fairbank et al.11 on the effectiveness of professional training to promote the onset of breastfeeding found increased knowledge of the staff, but did not identify statistically significant changes regarding the onset of breastfeeding. Another review12 of interventions with professionals, with the duration of breastfeeding as the outcome, concluded that the evidence was still insufficient and recommended that studies report intermediate outcomes of interventions, such as professional knowledge and practices.
The Baby-Friendly Hospital Initiative (BFHI) is a strategy that starts with awareness, training, and mobilization of health care professionals working in hospitals with obstetric beds, aiming to establish rules and routines favorable to the practice of breastfeeding. It was launched in 1990 by the WHO and The United Nations Children's Fund (UNICEF) during a meeting where the Declaration of Innocenti was signed.13 At this meeting, global goals were proposed and the “Ten Steps to Successful Breastfeeding” were established.13
Step 2 of the BFHI refers to the training of staff to acquire the necessary knowledge and skills to implement the hospital norms and routines in breastfeeding and, thus, the BFHI course is both theoretical and practical.14
No reviews were found that focused on the influence of health professionals’ training in breastfeeding on their knowledge and practices. Considering the importance of professional training to improve hospital practices aiming to increase breastfeeding rates, the objective of this systematic review was to highlight the impact of training interventions on breastfeeding in health professionals working in hospitals regarding their professional knowledge, skills, and practices, as well as hospital practices.
MethodsA systematic review of the scientific literature was conducted through the Medical Literature Analysis and Retrieval System Online (MEDLINE), Scopus, and Latin American and Caribbean Health Sciences (LILACS) databases. The search was carried out in September 2014 and focused on the training of health professionals that worked in hospitals regarding breastfeeding support. The search strategy used in the MEDLINE and Scopus databases was: breast feeding and health professionals and (capacity or training or education) and (knowledge or professional practice) and (hospital or maternity hospital); and in LILACS: breastfeeding and health professional and (training or education) and (knowledge or skill or professional practice) and the equivalent words in Portuguese.
The study inclusion criteria were: original articles reporting on breastfeeding training and its impact on the professionals’ knowledge, skills, practice, and/or hospital practices. Qualitative methodology articles, studies lacking a comparison control group, review articles, studies carried out in the primary health care network, studies whose outcomes exclusively comprised the professional's belief and/or attitude, studies with specific populations such as preterm infants or HIV-positive mothers, and studies focusing on the impact of training on the duration of breastfeeding in the post-discharge period were excluded from the systematic review. There was no limitation on the publication year or language.
Abstract search was performed independently by two authors of this systematic review. At this phase, articles were excluded according to the study selection criteria. In case of discordance regarding the abstract, the authors opted to read the full text.
An additional search was performed, based on the reference lists of articles read in full, to increase sensitivity, thus identifying articles that were not retrieved through the electronic search. After reading them in full, a new exclusion was carried out according to the same study selection criteria. Disagreements were resolved by consensus or by consultation with a third reviewer.
Data were extracted using a standardized form and the final classification regarding inclusion in the review was also performed independently; the results were compared and disagreements resolved by consensus between the two reviewers, with referral to a third reviewer in cases of persistent doubts.
The articles were also independently assessed regarding their quality, through a scoring system with a maximum score of 20 points. The protocol for assessing the quality was adapted from Downs and Black,15 and consists of 20 questions: (1) Was the hypothesis/objective clearly described?; (2) Were the study outcomes clearly described in the Introduction or Methods section?; (3) Were the characteristics of the patients included in the study clearly described?; (4) Were the interventions of interest clearly described?; (5) Was the distribution of confounding factors in each group clearly described?; (6) Were the main findings of the study clearly described?; (7) Did the study provide estimates of random variability of data for the main outcomes?; (8) Are the characteristics of the lost patients clearly described?; (9) Were the 95% confidence intervals and/or p-values reported for associations with major outcomes, except when the p-value was<0.001?; (10) Were the subjects invited to participate in the study representative of the population from which they were recruited?; (11) Was there an attempt at blinding subjects submitted to the intervention?; (12) Were the statistical tests used to assess the significance of the associations with the main outcome measures adequate?; (13) Were the comparison groups maintained?; (14) Were the main outcome measures accurate (valid and reliable)?; (15) Were the groups to be compared obtained from the same population?; (16) Were the study subjects recruited in the same period of time?; (17) Were the subjects in the intervention group randomized?; (18) Was there adequate adjustment for confounding factors in the analysis from which the main findings were obtained?; (19) Were the losses to follow-up taken into account?; (20) Did the study have enough power to detect a significant clinical effect, in which the probability value for the difference due to chance is less than 5%?
Each question was scored with 0 (negative) or 1 (positive). Considering the score achieved by each study, the evaluated items were classified as poor (0–9 points), regular (10–14 points), or good (15–20 points). Articles with poor quality were excluded from the review because they were considered to have low internal validity.
Two tables were constructed, according to the outcome. The first shows articles whose assessed outcome were professional knowledge, skills, and/or practice, and the second shows articles whose outcome were hospital practices. Both professional and hospital practices in general were evaluated using the Ten Steps to Successful Breastfeeding as the parameter (Table 1). The articles investigating the two outcomes are shown in Tables 2 and 3.
Ten steps to successful breastfeeding.
| 1 | Have a written breastfeeding policy that is routinely communicated to all health care staff. |
| 2 | Train all health staff in skills necessary to implement this policy. |
| 3 | Inform all pregnant women about the benefits and management of breastfeeding. |
| 4 | Help mothers initiate breastfeeding within half an hour of birth. |
| 5 | Show mothers how to breastfeed and how to maintain lactation, even if they should be separated from their infants. |
| 6 | Give newborns no food or drink other than breastmilk, unless medically indicated. |
| 7 | Practice rooming in by allowing mothers and babies to remain together 24 hours a day. |
| 8 | Encourage breastfeeding on demand. |
| 9 | Give no artificial teats or pacifiers to breastfeeding infants. |
| 10 | Foster the establishment of breastfeeding support groups and refer mothers to them on discharge from the hospital. |
Studies on the impact of training of health professionals on their knowledge, skills, and practices.
| Author (year of publication), place and year of performance | Quality score | Study setting, population, and sample size | Study design | Exposure variable | Outcome and method of assessment | Results |
|---|---|---|---|---|---|---|
| Westphal et al.16 (1995) Santos/SP/Brazil 1992–1993 | Fair (13/20) | • 8 public or philanthropic hospitals: intervention group – 4; control group – 4 • 12 trained professionals: 3 per hospital of intervention group | • Randomized clinical trial (hospital randomization) | • Theoretical and practical training: Course (Wellstart-SLC) lasting 14 days, 133h, of which 1/3 is practical training | • Professionals1 knowledge: pre- and post-test (comparison through scores) | • Knowledge - Improvement in the intervention group knowledge scores: 20.27 (±7.41)→26.92 (±2.10). (control group not assessed) |
| McIntyre17 (1996) Australia 1994–1995 | Fair (12/20) | • Southern metropolitan region of Adelaide • 65 health professionals | • Before and after type | • 2 workshops on advantages and management of BF, during 2 months • Each workshop was repeated at 3 different occasions | • Professionals’ knowledge: questionnaires were self-administered before the 1st workshop and after the 2nd (comparison through scores) | • Knowledge - Improved professionals’ knowledge score: 73.7 (±12.8)→88.5 (±7.4)a |
| Rea et al.7 (1999) São Paulo/SP/Brazil 1996 | Good (15/20) | • 1 public maternity hospital • 60 health professionals: 20 in the intervention group and 40 in the control group | • Randomized clinical trial | • Theoretical and practical training: WHO/UNICEF 40-h Counseling Course, with 8h of practice | • Professionals’ knowledge and skills: pre-test, post-test soon after training (comparison through scores) | Experimental group vs. control group: • Knowledge - Pre-test: 6.23 vs. 6.06 - Post-test: 8.35 vs. 5.54a • Post-course clinical and counseling skills - Clinical history: 5.2 vs. 3.8a - BF assessment: 9.9 vs. 8.6a - Nonverbal communication: 22.2 vs. 17.7a - Listening and learning: 19.4 vs. 12.2a -Confidence and support: 36.0 vs. 24.3a |
| Hernández-Garduño & de la Rosa-Ruiz18 (2000) Mexico 1996–1997 | Fair (12/20) | • 1 general hospital • 140 nursing professionals (among 152 eligible) | • Before and after type | • Theoretical and practical training in breastfeeding: 18h, with 1/3 of practice | • Knowledge: self-administered questionnaire before and soon after the course (comparison through scores, from 0 to 10 points) | • Knowledge 107 professionals from mother-child assistance services 5.3 (±1.4)→7.6 (±0.9)a 33 from other services: 5.6 (±1.4)→8.0 (±0.6)a |
| Cattaneo & Buzzetti19 (2001) Italy 1996–1998 | Good (16/20) | • 8 eligible hospitals Group 1: 4 hospitals with 377 trained professionals (of 536 eligible): from 10/1996 to 02/1997 Group 2: 3 hospitals (1 loss) with 194 trained professionals (of 237 eligible) from 10/1997 to 02/1998 • 2669 mother-child binomials (with L>2000g, with no admission at the ICU) | • Quasi-experimental (with before and after component) | • Multiplier training in 24-h courses (18h+2h counseling+4 clinical practice) that trained groups 1 and 2 through the 18-h BFHI course | • Professionals’ knowledge: self-administered questionnaire at baseline (06/1996) and after each training course (comparison through scores) | • Knowledge Baseline→post-training of group 1→post-training of group 2: - Group 1: 0.41→0.66→0.72 - Group 2: 0.53→0.53→0.75 (p-value not mentioned) |
| Owoaje et al.20 (2002) Nigeria 1997 | Fair (13/20) | • 1 tertiary hospital, 2 secondary hospitals, and 13 basic units with obstetric care) • 298 nurses (of 305 eligible professionals) working for at least 6 months: 113 trained and 185 in the control group | • Quasi-experimental (with previous intervention) | • Theoretical and practical training: WHO/UNICEF BFHI 18-h course | • Knowledge and professional practices: self-administered questionnaire (comparison of knowledge on EBF through proportions and scores (0–20 points); about problems and management of problems in breastfeeding through proportions | • Knowledge Experimental vs. control: On the advantages of EBF - knowledge scores of (11 items): 11.9 (±1.84) vs. 10.7 (±2.4) - difference only for diarrhea reduction: 97.3% vs. 87.0%a 2. On causes and management of BF problems. - effect of pre-dairy,a sore nipples,a insufficient milk,a breast engorgement,a mastitis,a management of neonatal jaundice • Professional practices Experimental vs. control - Step 4 (BF start): 91.2% vs. 81.6%a - Step 5 (expression by hand): 75.2% vs. 65.4% - Step 6 (not using pre-dairy): 73.5% vs. 54.6%a - Step 7 (rooming in): 94.7% vs. 94.1% - Step 10 (post-discharge support): 59.3% vs. 41.1%a |
| Martens9 (2000) Canada 1998 | Fair (13/20) | • 2 small hospitals in rural areas. • Intervention Group: 1 hospital, 15 of 24 eligible nursing professionals • Control Group: 1 hospital, 16 of 19 eligible nursing professionals • Breastfed babies: 26 in the intervention hospital and 23 in the control hospital | • Quasi-experimental | • Training lasting 1.5h with nurses during work hours and optional tutorial • Focus on knowledge of the management of BF and BFHI policy | • Adherence to BFHI principles: Self-administered questionnaire before the intervention and after 8 months (comparison of proportions) | • Professional practices Intervention hospital: - Step 1: Information on norms: 15%→87%a - Step 3: discuss benefits of BF: 60%→73% - Step 4: offer help to start BF within the 1st hour: 75%→87% - Step 5: record latching/position: 45%→67% - Step 5: guide expression by hand: 40%→73%a - Step 6: does not encourage use of supplements: 30%→67%a - Step 8: does not limit BF on demand: 5%→7% - Step 9: does not recommend use of bottle: 30%→67%a - Step 10: guides post-discharge BF support: 5%→67%a |
| Moran et al.24 (2000) United Kingdom 1999 | Fair (10/20) | • 4 hospitals: 3 experimental and 1 control • 13 obstetric nurses evaluated before the course and 15 after the course | • Quasi-experimental | • Training of WHO/UNICEF management in maternal BF: 20h | • Professionals’ skills: analyzed through pre-validated BeSST (Breastfeeding Support Skills Tool) tool using video clips. Questionnaires were self-administered (comparison of scores) | • Skills Experimental vs. control: - Skill scores in the management of BF support: 29.9 vs. 19.8a |
| Zakarija-Grković & Burmaz21 (2010) Croatia 2007–2009 | Fair (12/20) | • 5 large hospitals. • 308 professionals trained of 424 eligible (72.6%) | • Before and after type | • Theoretical and practical training: WHO/UNICEF BFHI course: 20h | • Professional knowledge and practices: Questionnaires were self-administered before the training (n=223) and after 3 months (n=213) (comparison of hit ratios) | • Knowledge Definition of EBF,a time of first BF,a role of prolactin,a signs of inadequate positioning for BF,a hospital support practices,a signs of inadequate latching, barriers to BF. • Professional practices - Recommendation on duration of EBFa and BF,a management of insufficient milk productiona and mastitis,a adherence to ICMBMS,a BF recommendation after C-section, BF management when the baby refuses to suck |
| Wissett et al.22 (2000) United Kingdom Year not mentioned | Fair (12/20) | • 1 hospital • 22 professionals: nurses and home visitors (pre-test: 22 and post-test: 18) | • Before and after type | • Training in WHO/UNICEF Maternal Breastfeeding management: 20h | • Knowledge: self-administered questionnaire before and 8 weeks after the course (comparison through median scores, maximum: 30) | • Knowledge - Median overall score: 17→24a |
| Bernaix et al.23 (2010) United States Year not mentioned | Fair (13/20) | • 12 hospitals • Intervention Group: 9 hospitals, 203 nurses (of 297 eligible ones) • Control Group: 4 hospitals (with 1 loss), 34 nurses (of 64 eligible) | • Quasi-experimental | • Ten modules of self-teaching material to be studied for 4–6 weeks before the post-test | • Knowledge: Self-administered questionnaire with 50 items (comparison of proportions and mean scores) | • Knowledge Experimental vs. control: 64%→78%avs. 61%→62% 31.9→39.2avs. 30.5→31.7 |
BF, breastfeeding; EBF, exclusive breastfeeding; BFHI, Baby Friendly Hospital Initiative; WHO/UNICEF, World Health Organization/The United Nations Children's Fund; ARF, acute respiratory failure; ICMBMS, The International Code of Marketing of Breastmilk Substitutes.
Studies on the impact of training of health professionals on hospital practices.
| Author (year of publication), place and year of performance, quality score | Quality score | Study setting, population, and sample size | Study design | Exposure variable | Outcome and method of assessment | Results on hospital practices |
|---|---|---|---|---|---|---|
| Westphal et al. 16 (1995) Santos/SP/Brazil 1992–1993 | Fair (13/20) | • 8 public and philanthropic hospitals: intervention group – 4; control group – 4 • 12 professionals trained: 3 per hospital intervention | • Randomized clinical trial (hospital randomization) | • Theoretical and practical training: Course (Wellstart-SLC) lasting 14 days, 133h, with 1/3 practical training | • Adherence to BFHI Steps 1–10: interviews with managers, health professionals, pregnant women, and mothers before and six months after training | • Differences in institutional scores by hospital pairs (experimental or control): Pair 1: 0.6 vs. 0.9; Pair 2: 1.6 vs. −0.7 Pair 3: 1.9 vs. 0.2; Pair 4: 0.5 vs. 0.2 • Institutional changes: significant advance in Steps 1, 2, 10 (p-value not stated) |
| Prasad & Costello25 (1995) India 1992–1993 | Fair (13/20) | • 1 public hospital in the countryside • Hospital Administrators, 8 physicians, 1 ward sister, 9 nurses • Mother-child binomials with normal delivery and healthy babies (172 at baseline, 195 soon after the intervention, and 101 six months later) | • Before and after type (with comparison between exposed and non-exposed six months post-intervention) | • ≥ 5 individual or group sessions with health education doctors on Steps 4 and 6 | • Changes in hospital practices related to Steps 4 and 6: Mothers interviewed at home two weeks after delivery (at baseline, soon after the intervention and six months post-intervention) | Baseline→soon after the intervention→6 months post-intervention Mothers exposed to health education: 0%→100%→36% - Step 4: BF within the 1st hour of life: 3%→60%→14% - Step 6: use of supplements: 96%→43%→77% (both significant advances, but p-value is not mentioned) Six months post-intervention: - Step 6: use of supplements: 42% (of exposed, n=36) vs. 97% (of non-exposed, n=65) a |
| Taddei et al.26 (2000) Santos/SP 1992–1993 | Fair (14/20) | • 8 public or philanthropic hospitals: intervention group – 4; control group – 4 • 12 trained professionals: 3 per intervention hospital • Mother-child binomials: 494 of 609 eligible (pre-training) and 469 of 555 eligible (post-training) | • Randomized clinical trial (hospital randomization) | • Theoretical and practical training: 14-day, 133-h course (Wellstart-SLC course), with 1/3 practice | • Changes in hospital practices regarding Steps 4, 5, and 7: interview to mothers during home visits (one and six months after delivery) | • Before/after, exposedvs.non-exposed: - Step 4: BF in the delivery room: 2%→23%a×2%→8%a - BF within the first 6h: 41%→53%a×48%→50% - Step 5: BF support at the hospital: 48%→64%avs. 58%→61% - Step 5: BF support at the hospital: 29%→49%avs. 35%→36% - Step 7: rooming in: 8%→6% vs. 20% →13%a |
| Cattaneo & Buzzetti19 (2001) Italy 1996–1998 | Good (16/20) | • 8 eligible hospitals Group 1: 4 hospitals with 377 trained professionals (of 536 eligible) from 10/1996 to 02/1997 Group 2: 3 hospitals (1 loss) with 194 trained professionals (of 237 eligible) from 10/1997 to 02/1998 • 2669 Mother-child binomials with BW>2000g, without ICU admission | • Quasi-experimental (with before and after component) | • Multiplier training in 24-h courses (18h+2h counseling+4 clinical practice) that trained groups 1 and 2 using the BFHI 18-h course | • Adherence BFHI Ten Steps: Self-administered questionnaire by professionals (steps 1 and 2), interview to mothers pre and post-evaluation (Steps 4–10) Baseline→post-training | • Before/after – overall result: - Mean adherence to the Steps: 2.4→7.7 steps (p-value not mentioned) • Before/after – group 1 and group 2: - EBF at discharge: 41%→77% and 23%→72% (p-value not mentioned) - Step 4: BF within the 1st hour: 12%→22%a and 37%→60%a - Step 5: latching/positioning: 67%→88%a and 77%→93%a - Step 5: expression by hand: 60%→75%a and 43%→72%a - Step 6: use of supplements: 35%→17%a and 8%→8% - Step 7: rooming in: 72%→89%a and 36%→77%a - Step 8: BF on demand: 83%→97%a and 97%→99% - Step 9: use of bottle: 58%→14%a and 70%→26%a - Step 9: use of pacifier: 56%→19%a and 63%→52%a • Less advancement in Steps 1, 2, and 10 (p-value not mentioned) |
| Durand et al. 27 (2003) France 1997–2000 | Fair (11/20) | • 1 tertiary maternity hospital • All 73 professionals from the staff • Mother-child binomials without ICU admission: 50 before the training program and 50 after (with 71.4% of response rate) | • Before and after type | • Three-day theoretical and practical training on the benefits and management of breastfeeding (10 professionals per class) from 1998 to 2000 | • Changes in hospital practices related to Steps 4–7, 9, 10: assessment of newborns’ records and self-administered questionnaire, given to mothers at the time of hospital discharge | • According to medical record: - Step 4: BF within the 1st hour: 7.9%→21% - Step 6: use of supplements: 82%→63% - Step 7: mother-child separation>4h: 52%→13%a - Step 9: formula only in cup: 0%→13.1%a - Step 9: use of bottle: 82%→26%a - EBF at discharge: 14%→28% • According to the questionnaire: - Step 5: teach positioning for breastfeeding: 41.7%→69.2%a - Step 10: post-discharge support resources: 8.3%→57.7%a |
| Labarere et al. 28 (2003) France 1997–2000 | Fair (14/20) | • 1 tertiary maternity • All 73 professionals of the staff • Mother-child binomials without ICU admission: 323 (pre-training) and 324 (post-training) | • Before and after type | • Three-day theoretical and practical training on benefits and management of breastfeeding (10 professionals per class) from 1998 to 2000 | • Changes in hospital practices regarding Steps 4–7, and 9: assessment of maternal medical records before and after training retrospectively by nurse not involved in assistance | EBF at discharge: 15.8%→35.2%a - Step 4: BF within the 1st hour of life: 9.2%→16.9%a - Step 6: use of supplements: 77.6%→54.0%a - Step 7: rooming in: 56.6%→72.6%a - Step 9: formula in the cup: 0.4%→23.8%a use of bottle: 77.2%→14.1%a |
| Martens9 (2000) Canada 1998 | Fair (13/20) | 2 small hospitals in rural areas • Intervention Group: 1 hospital, 15 of 24 eligible nursing professionals • Control Group: 1 hospital, 16 of 19 eligible nursing professionals • Breastfed babies: 26 in the intervention hospital and 23 in the control | • Quasi-experimental | • 1.5-h training with nurses during working hours+optional tutorial • Focus on knowledge of BF management and BFHI policy | • Adherence to BFHI and Steps 1, 2, 6, 7, 9, and 10 by the hospital: Self-administered questionnaire by professionals before the intervention and 8 months after. • EBF during hospital stay: assessment of newborn's medical record (intervention: 13 pre and 13 post; control: 14 pre and 9 post) | • According to the questionnaire: Intervention hospital: - Step 1: written norm: 40%→87%a - Step 2: skills in BF management: 35%→60% - Step 6: non-use of supplement: 45%→87%a - Step 7: rooming in: 90%→100% - Step 9: non-use of bottle: 30%→67%a - Step 9: non-use of pacifier: 50%→67% - Step 10: encourage support groups: 5%→47%a • According to medical records: experimental vs. control-Adherence to BFHI: 24.4%→31.9%a×20.2%→22.5% - EBF during hospital stay: 31%→54%a×43%→0%a |
| Coutinho et al.29 (2005) Pernambuco 1998 (previous cohort) and 2001 | Fair (13/20) | • 2 hospitals from SUS • 42 professionals trained (90% of midwives and nurse aids) • 334 mother-child binomials of 364 eligible ones (2001) compared to 364 (1998). Urban area, single birth, with BW ≥2500g, healthy | • Before and after type (historical control) | • Theoretical and practical training:18-h WHO/UNICEF-BFHI course+2h of breastfeeding counseling and educational material | • Adherence to Steps 4 to 9 of BFHI: interview with mothers in the first 48h and 10 days after delivery. | historical control→experimental group - Step 4: Skin-to-skin contact: 25.8%→37.2%a Help with BF at birth: 5.8%→6.0% - Step 5: latching/positioning: 9.6%→21.0%a - Step 6: EBF within the 1st 48h: 21.2%→70.0%a - Step 9: use of pacifier: 47.2%→24.3%a (other steps – results not shown) |
| Zakarija-Grković et al.30 (2012) Croatia 2008 – 2010 | Good (16/20) | • 1 tertiary hospital • Trained 80% of the 271 staff professionals • Mother-child binomials (388 pre-training and 385 post) with BW>2500g, without ICU admission, single births (interviewed 94.2% of eligible) | • Before and after type | • Theoretical and practical training: 20-h WHO/UNICEF-BFHI course: one class in May 2008 and another in February 2009 | • Adherence to Steps 3 to 9 of BFHI: assessment of newborn's medical record; interview with mothers pre and post-training | • According to the medical record: - EBF within 48h: 6.0%→11.7%a • According to the interviews: - Step 3: recommendations on child feeding: 10.8%→9.9% - Step 4: held the baby at the 1st contact for>60min: 0.8%→3.2%a - Step 4: baby sucked at the 1st contact: 8.6%→4.2% - Step 5: help with latching/positioning: 70.3%→69.0% - Step 5: was shown expression by hand: 44.1%→44.8% - Step 6: use of supplements: 81.1%→79.4% - Step 7: rooming in: 0.3%→5.1%a - Step 8: BF on demand: 21.1→29.3%a - Step 8: duration on demand: 17.5%→28.6%a - Step 9: use of bottle: 79.0%→77.8% - Step 9: use of pacifier: 0.3%→0% |
BF, breastfeeding; EBF, exclusive breastfeeding; BFHI Baby-Friendly Hospital Initiative; BW, birth weight.
The columns of the tables show: the article's first author, year of publication, the place and year the study was performed; quality score obtained; the study setting, population, and sample size (or the number of participants when the article does not specify the sample size); the study design (studies in which there was a randomization process were considered randomized controlled trials; studies with external control group but without randomization were considered quasi-experimental studies, and those with internal control group were considered “before and after” interventions); the exposure; the assessed outcome and the evaluation method; and, finally, the observed results. Each line shows an article, which are shown by year of the study (Tables 2 and 3).
The effect of training with the Ten Steps to Successful Breastfeeding14 on the hospital practices was summarized in the last paragraph of the results, considering the effect as positive when the changes were significant or when 100% of compliance with the Step was achieved.
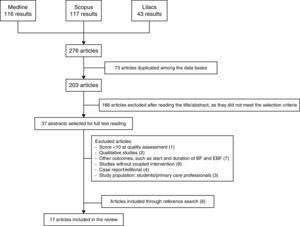
ResultsA total of 116 articles were found in the MEDLINE database, 117 in the Scopus database, and 43 in the LILACS database, from which 37 articles considered relevant for the subject were selected for full reading. After exclusion of the qualitative studies, those that did not address the outcomes discussed in this review, studies whose study population did not consist of health professionals working in a hospital network, studies without a coupled intervention, and those with quality score <10 points, 11 articles remained. Six articles were included by reviewing the references of the studies read in full, totaling 17 articles included in the review (Fig. 1).
Of the 17 articles, nine addressed professional knowledge,7,16–23 two professional skills,7,24 three professional practices,9,20,21 and nine hospital practices.9,16,19,25–30
The studies addressed interventions that were classified as randomized controlled trials (3),7,16,26 quasi-experimental studies (5),9,19,20,23,24 and the “before and after” type, which used an internal control group (9)17,18,21,22,25,27–30 (Tables 2 and 3). Results related to breastfeeding duration after hospital discharge were not included in this review.
The studies were carried out between 1992 and 2010 in several countries: four in Brazil,7,16,26,29 one in Mexico,18 one in the United States,23 one in Canada,9 two in the United Kingdom,22,24 two in France,27,28 one in Italy,19 two in Croatia,21,30 one in Nigeria,20 one in India,25 and one in Australia.17 The setting of these studies was varied: large and small hospitals, of low and high risk, public and philanthropic institutions, in urban and rural areas. The main target audience of these courses was nursing professionals/staff, physicians, and home visitors.
The training courses were diverse: theoretical and practical BFHI training14 lasting 18–24h was employed in five studies,19–21,29,30 while two22,24 used a breastfeeding management course,31 and the WHO counseling32 course lasting 40h was used in one study.7
Two studies used a Wellstart-SLC (Santos Lactation Center)33 course lasting 133h,16,26 two applied 3 day courses on the benefits and management of breastfeeding,27,28 one applied an 18-h theoretical–practical course on maternal breastfeeding,18 one study applied a night workshop,17 one used a 1.5-h training complemented by tutorial material,9 one used material for self-learning,23 and one study used a methodology comprising five discussion sessions with each professional.25
The outcome defined by nine studies was the professionals’ knowledge of breastfeeding, two studies investigated the capacity of professionals in counseling and management of breastfeeding, three investigated professional practice, and nine investigated hospital practices, usually regarding adherence to the BFHI steps.
As for the evaluation method, twelve studies evaluated the effect of training through interviews or questionnaires that were self-administered by health professionals, six evaluated through an interview or a questionnaire that was self-administered by the mothers, one reported the observation of the maternity areas, and three performed a retrospective evaluation through the analysis of maternal and/or neonatal medical records. Regarding the type of analysis, most studies performed only comparative analyses using statistical significance tests7,9,16–18,20–23,25–27,29 and three used multiple logistic regression analysis.19,28,30
Regarding the quality assessment, three studies were classified as having good internal validity,7,19,30 whereas 14 were classified as fair.9,16–18,20–29
In the nine studies that investigated knowledge, the intervention showed positive results. Five studies measured gain of knowledge through general scores, and one by specifying the factors that achieved improvement. In two studies,21,24 the professionals were trained through the theoretical and practical training of BFHI14 with a duration of 20h, one with a duration of 18h,20 one through the WHO counseling course32 lasting 40h,7 one intervention trained multipliers using the Wellstart-SLC16 133-h course,33 one applied the 18-h theoretical and practical course on breastfeeding,18 one study used workshops applied during the night shift,17 and one provided material for self-learning.23 A superior effect was not identified in interventions with longer duration.
Only two studies investigated the effect of training through breastfeeding counseling31 and management32 courses on the professional skills, with one study discriminating the gains in listening and learning, and building confidence and giving support,7 and another demonstrating the achieved advances through mean scores.24 Three studies had professional practices as outcome,9,20,21 with gains being observed only in part of the practices (Table 2). Nine studies9,16,19,25–30 evaluated the changes in hospital practices, obtaining advances in most of them (Table 3).
As for the results of training on hospital changes related to the Ten Steps,14 the object of nine studies, Step 3 was the least assessed, by only two investigations, with no effect.16,30 Steps 1, 2, and 8 were also scarcely investigated, by only three studies,9,16,19 with positive changes being achieved in two-thirds of interventions for Steps 1 and 8 and in one-third for Step 2. Step 10, assessed in four interventions,9,16,19,27 showed advances in three. Step 5, assessed in six studies,16,19,27,29,30 reached positive changes in two-thirds of the interventions. The training had a positive effect on five of the seven interventions that assessed Step 79,16,19,26–28,30 and Step 9.9,16,19,27–30 Steps 416,19,20,25,27–30 and 69,16,19,25,27–30 were the most often assessed, in eight studies each, showing favorable changes in 75% (Step 4) and 62.5% (Step 6) of the interventions (Table 3).
DiscussionThe studies included in this review showed positive effects of training on the assessed outcomes: professional knowledge, skills, and practices, as well as hospital practices.
The studies were carried out in different contexts, in developed and developing countries on five continents (America, Europe, Africa, Asia, and Oceania). This diversity seems to indicate that in diverse scenarios, the courses used were at least partially effective, despite economic, ethnic, and cultural differences.
All training methods employed, regardless of the model, duration, and target audience, showed increase in the knowledge and skills of health professionals in breastfeeding, with no dose-response effect observed in this systematic review for the number of class-hours and the obtained effect. Benefits for professional and hospital practices were also observed; however, the interventions did not always achieve changes regarding the “Ten Steps to Successful Breastfeeding”.
Steps 1–3, 8, and 10 were the least investigated. Among them, Step 2 (train the entire health staff) and Step 3 (inform pregnant women) showed fewer positive results. Possibly, the lower performance in Step 2 is due to training programs that did not include all professional categories, in addition to staff turnover, which impairs the permanence of trained staff.34
As for Step 3, the prenatal clinic is very often located outside the hospital complex, and the professionals that provide prenatal care are not the same as those working in the maternity hospital. This hinders their involvement with the BFHI and the investigation of adherence to this Step.35 It is worth mentioning the importance of providing information to pregnant women about the benefits and management of breastfeeding, as most women define their intention to breastfeed during pregnancy,36 which influences the onset and duration of breastfeeding.37 In a study that nationally re-evaluated adherence to the Ten Steps in 167 Brazilian BFHI accredited between 1992 and 2000, Araujo and Schmitz10 also found lower adherence to Steps 2 and 3.
Step 1 (written norm) and Step 8 (stimulus to breastfeeding on demand) obtained positive results in two-thirds of the interventions, indicating that the training programs may be useful for the disclosing of the institution's breastfeeding policy and for the encouragement of breastfeeding on demand. In Brazil, in Sao Paulo38 and Rio de Janeiro,35 little restriction was observed regarding the free interval between feedings in public and private hospitals, showing good adherence to this procedure.
The training also showed to be effective in promoting improvements in the practice of Step 10 (post-discharge support) in three-quarters of the interventions, which is a relevant result, considering the difficulties found in carrying out this step in different Brazilian scenarios.29,35
Steps 4–7, and 9, which are basically hospital-related, were more often investigated; the training programs showed positive effects in most studies. Regarding Step 4 (help initiate postpartum breastfeeding), one of the major barriers to breastfeeding at birth has been cesarean delivery,39 which is on the rise in the Brazilian context;40 it is important that professionals are able to stimulate skin-to-skin contact and early suction even in babies born through C-section.
Regarding Step 5 (management of breastfeeding), adequate management of breastfeeding depends not only on theoretical training, but also the acquisition of skills by the health professional that assists mothers. Most of the training programs studied in this review were both theoretical and practical, which may have contributed to the positive results achieved by 75% of the interventions. Advances in 62.5% of the interventions regarding the Step 6 (not offer the newborn other foods or drinks rather than breast milk) suggest that, despite its difficult adherence due to the pressures of infant formula industry marketing, hospital routines have advanced significantly.10,35,41
The positive results observed in more than 70% of the studies investigating Step 7 (rooming in) indicates evolution in the structure and routine of hospitals, because rooming in depends not only on professional training.26 Regarding Step 9 (not using artificial nipples or pacifiers), the use of pacifiers and bottles may prevent the adequate dynamic of sucking the nipple-areola region and reduce the frequency of feedings and, thus, the reduction observed in the use of these artifacts in more than 70% of the studies that investigated them is extremely beneficial.
A study conducted in the United States42 demonstrated that Steps 4, 6, and 9 were associated with longer duration of breastfeeding and that mothers exposed to at least six hospital practices recommended by the BFHI had a 13-fold higher chance of maintaining breastfeeding, compared to mothers who did not have contact with any of the practices. The observed dose-response effect indicates the importance of training programs aimed at target audiences, such as healthcare professionals from various professional categories and working in the different areas assisting pregnant women, mothers, and babies, so that hospital practices coalesce, resulting in a synergistic effect on the duration of breastfeeding.
Regarding the limitations found in this systematic review, the authors emphasize the differences in the training programs used in different studies regarding the duration, type, and target audience, making it difficult to identify the most effective methods, duration, and content to generate changes in knowledge, skills, and professional and hospital practices. The lack of a homogeneous method of study analysis, which would facilitate the comparison of results, hindered the calculation of summary measures by meta-analysis.
Another limitation found was the absence of a homogeneous analysis method among the studies, which would facilitate comparison of the results. The studies had different epidemiological designs, and the absence of experimental studies indicates a higher risk of bias and uncontrolled confounding variables. The evaluation of the articles through the quality score showed fair quality in most articles, but only three showed good internal validity. The retrospective data collection (from records) was also a limiting factor in some studies,27,28 caused by the possibility of information bias due to error or the absence in the data recording. Most studies did not mention the representativeness of the sample that was selected and submitted to evaluation. Most poorly summarized and described their results, hindering the presentation of result interpretation and uniformity.
The short period between interventions and evaluations used in most studies did not allow verifying whether changes in professional knowledge, skills, and practices, as well as in hospital practices, can persist in the long term after the interventions.21,30 Factors such as staff turnover and policy changes could interfere with the results of evaluations carried out after longer post-training intervals. To maintain the impact of these training programs, it is necessary to reapply them periodically.7
Information on the context of the interventions, on the available data for evaluation, and on the cost-effectiveness of the employed training programs was sparse or absent, which reduces the possibility of reproducing the research along similar lines to those undertaken in other settings. This information could be of great value for health facility managers and for future studies.
Despite these limitations, the results of this review demonstrate that the training of health professionals in breastfeeding promotion brings improvements in knowledge, skills, and practices, even when the training does not follow the WHO/UNICEF standards.
As for adherence to the Ten Steps, the evidence found in the review was less consistent. It must be recalled that these practices depend not only on professional training, but also on administrative management support for institutional changes.21
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: de Jesus PC, de Oliveira MI, Fonseca SC. Impact of health professional training in breastfeeding on their knowledge, skills, and hospital practices: a systematic review. J Pediatr (Rio J). 2016;92:436–50.