Therapeutic hypothermia reduces cerebral injury and improves the neurological outcome secondary to hypoxic ischemic encephalopathy in newborns. It has been indicated for asphyxiated full-term or near-term newborn infants with clinical signs of hypoxic-ischemic encephalopathy (HIE).
SourcesA search was performed for articles on therapeutic hypothermia in newborns with perinatal asphyxia in PubMed; the authors chose those considered most significant.
Summary of the findingsThere are two therapeutic hypothermia methods: selective head cooling and total body cooling. The target body temperature is 34.5°C for selective head cooling and 33.5°C for total body cooling. Temperatures lower than 32°C are less neuroprotective, and temperatures below 30°C are very dangerous, with severe complications. Therapeutic hypothermia must start within the first 6h after birth, as studies have shown that this represents the therapeutic window for the hypoxic-ischemic event. Therapy must be maintained for 72h, with very strict control of the newborn's body temperature. It has been shown that therapeutic hypothermia is effective in reducing neurologic impairment, especially in full-term or near-term newborns with moderate hypoxic-ischemic encephalopathy.
ConclusionTherapeutic hypothermia is a neuroprotective technique indicated for newborn infants with perinatal asphyxia and hypoxic-ischemic encephalopathy.
A hipotermia terapêutica reduz a lesão cerebral e melhora o desfecho neurológico de recém-nascidos após insulto hipóxico isquemico. Indicada para recém-nascidos a termo ou próximo do termo com evidência de asfixia perinatal e Encefalopatia Hipóxico Isquemica (EHI).
Fontes dos dadosFoi feita uma procura no PubMed por publicações sobre hipotermia terapêutica em recém-nascidos com asfixia perinatal e selecionadas aquelas julgadas mais relevantes pelos autores.
Síntese dos dadosHá duas técnicas de resfriamento corpórea: hipotermia seletiva da cabeça e hipotermia corpórea total. A temperatura de resfriamento deve ser 34,5°C para seletiva de cabeça e 33,5°C para corpórea total; temperaturas inferiores a 32°C são menos neuroprotetoras e abaixo de 30°C há efeitos adversos sistêmicos graves. Indica-se o início da hipotermia terapêutica até 6 horas após o nascimento, pois estudos evidenciaram que esta é a janela terapêutica da agressão hipóxico e isquêmica. A hipotermia deve ser mantida por 72horas com rigorosa monitorização da temperatura corporal do recém-nascido. A hipotermia tem sido efetiva em reduzir seqüelas neurológicas, principalmente em recém-nascidos de termo ou próximo do termo com encefalopatia hipóxico isquêmica moderada e em melhorar o prognóstico em longo prazo dos recém-nascidos com EHI.
ConclusãoA hipotermia terapêutica é uma técnica neuroprotetora indicada para recém-nascidos com asfixia perinatal.
More than a decade ago, experimental evidence, and subsequently, good-quality clinical trials initially appeared, suggesting that therapeutic hypothermia reduces brain damage and improves neurological outcome after neonatal hypoxic-ischemic injury.1–4 The best result in terms of therapeutic hypothermia prognosis seems to be in mild to moderate injuries, while the real benefit has been questioned for infants with severe encephalopathy. A multicenter study by the NICHD (National Institute of Child Health and Human Development) showed that cases persisting with severe hypoxic-ischemic encephalopathy (HIE) signs and altered neurological assessment at the discharge from the neonatology service after 72h of therapeutic hypothermia had higher mortality or morbidity in the follow-up at 18 months of life.5
The extent of cerebral injury following a hypoxic-ischemic insult basically depends on the balance between the causative mechanisms of irreversible injury, such neuronal necrosis or persistent inflammation, and endogenous protection (acute phase response, recovery, and neuronal repair). The neuroprotective strategy of therapeutic hypothermia involves the modulation of some irreversible injury mechanisms, such as inflammatory cascade inhibition, reduced production of reactive oxygen species, reduction in the metabolic rate with reduced oxygen consumption and carbon dioxide production, and an endogenous neuroprotective effect.6–9
The objective of this review is to understand the mechanism of action of therapeutic hypothermia, searching for evidence in the literature to establish the type of newborn that is a good candidate for this type of therapy, describing the protocol, possible complications, and supportive care for the management of newborns submitted to therapeutic hypothermia.
Mechanism of action of therapeutic hypothermiaHypothermia results in a reduction of cerebral metabolism by approximately 5% for each 1°C decrease in body temperature, which delays the onset of anoxic cell depolarization. The reduction in excitatory amino acids such as aspartate and glutamate, during the ischemic phase of therapeutic hypothermia, is due to the fact that they promote depolarization delay and intracellular calcium influx reduction. These effects have been demonstrated in different manners in experimental models of ischemia and reperfusion in rodents after cardiac arrest in young adult dogs, or during and immediately after hypoxic-ischemic injury in newborn pigs.8
Hypoxia-ischemia-reperfusion injury in the central nervous system activates a pro-inflammatory cascade of events characterized by leukocyte influx, including polymorphonuclear cells and monocytes, and microglial activation. Many of these inflammatory reactions are mediated by cytokines, especially neuronal apoptosis modulation. The cytokines with best-known actions in the CNS are: TNF-α, IL-1β, and IL-6. Part of the neuroprotective effect of hypothermia is due to proinflammatory pathway blockade.6,8
Cytokines are mediators of the systemic inflammatory response activation mechanism. In a situation of ischemia, enhanced endothelial activation occurs by monocyte activation, stimulating production of TNF-α, which promotes greater endothelial activation. The production of IL-6, IL-1β, IL-8, and PAF (platelet activating factor) occurs through several interactions.10 Furthermore, through the actions of soluble receptors, IL-6, IL-1β, and TNF-α increase the expression of adhesion molecules, especially intercellular adhesion molecule-1 (ICAM-1) in endothelial cells and in astrocytes, facilitating leukocyte infiltration and increasing leukocyte activation, with consequent promotion of systemic inflammatory response as the final result. Cytokines induce nitric oxide synthetase enzyme, which, together with TNF-α and IL-1β, promotes neurotoxic effects.8,9 Caspase activation may induce local inflammatory response involving energy consumption and increase in the number of apoptotic neurons, with the possibility of injury reversal, which is neuroprotective.6
In experimental models, prolonged hypothermia mechanism (72h) induced the reduction of necrosis and neuronal apoptosis.7,11 Cytochrome C suppression by mitochondria was demonstrated, as well as activation of caspase 3 in the cortex, thalamus, and hippocampus of rats with HIE that received hypothermia therapy for 72h.11
Therapeutic windowHypoxic-ischemic insult involves an ongoing injury process, where the severity of HIE depends on the duration and extent of this process. The central role of therapeutic hypothermia in neuroprotection involves the interruption or reduction of this process; essentially divided into acute or primary phase, in which some neural cells die and others recover, at least partially; the latent phase, with partially recovered oxidative metabolism, even with suppressed electroencephalographic activity9; and the secondary phase, which occurs after moderate to severe injury, initiating hours later, on average within 6 up to 15h, clinically manifested by the presence of seizures, cytotoxic edema, accumulation of excitatory amino acids, and failure of mitochondrial oxidative activity, which is the main factor associated with neuronal death.
It is important to act before the secondary phase, during the therapeutic window of opportunity when apoptotic neurons are able to recover. The degree of energy failure determines the type of neuronal damage (death) during the early and late stages, and the degree of trophic support influences angiogenesis and neurogenesis during the recovery phase of HIE.
Although exactly when the brain injury becomes irreversible has yet to be precisely established, there are consistent data indicating that the latency phase, also known as the early phase of recovery from transient restoration of cerebral oxidative metabolism, before the start of the secondary phase of energy failure, represents the best window for therapeutic intervention.8 Because this is an ongoing process, these phases are close, and therefore the transition to the moment of irreversible cell death is almost imperceptible.11,12
Since the first series of clinical cases of perinatal asphyxia, therapeutic hypothermia initiation has been indicated within 6h after birth, due to all the experimental evidence demonstrating that this represents the therapeutic window to inhibit or reduce the hypoxic-ischemic injury.11
Selection of newborn candidates for therapeutic hypothermiaIn the 2010 Consensus, the International Consensus on Cardiopulmonary Resuscitation (ILCOR) included the indication of therapeutic hypothermia for every newborn at term or near term who had developed moderate to severe HIE, using a specific protocol and follow-up coordinated by the regional reference care system.13
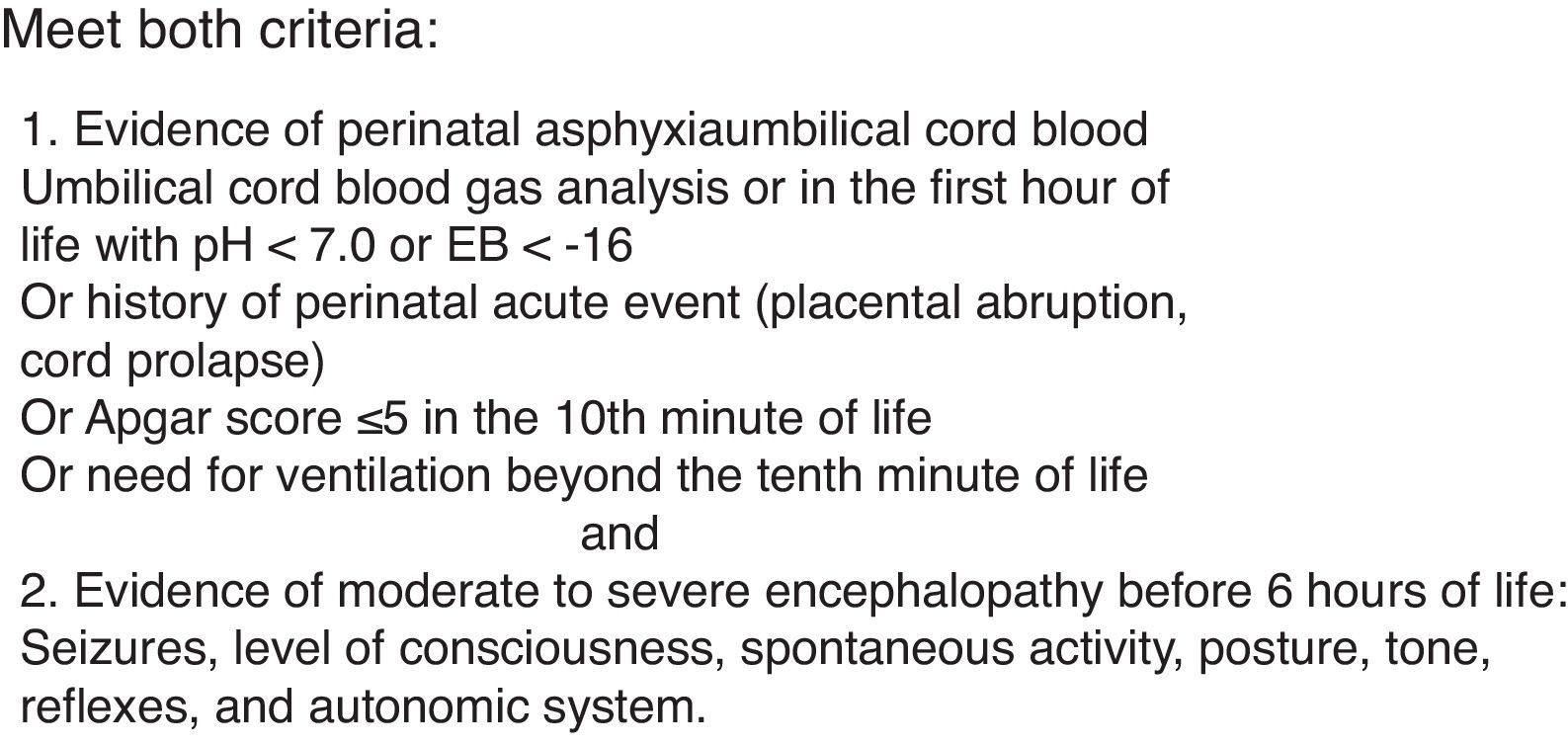
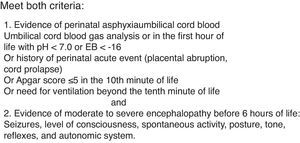
Overall, the indication of therapeutic hypothermia for newborns follows the recommendations found on the site of the Brazilian Society of Pediatrics and ILCOR13,14: newborns with gestational age>35 weeks, birth weight>1800g, who have fewer than 6h of life, and meet the following criteria.14
Evidence of perinatal asphyxia: umbilical cord blood gas analysis or in the first hour of life with pH <7.0 or base excess (EB) <−16 or history of perinatal acute event (placental abruption, cord prolapse), or Apgar score of 5 or less in the 10th minute of life, or need for mechanical ventilation beyond the 10th minute of life, or any of the following associated with evidence of moderate to severe encephalopathy before 6h of life: seizure, level of consciousness, spontaneous activity, posture, tone, reflexes, and autonomic system (Fig. 1).14
A Cochrane review reinforced the benefit of therapeutic hypothermia in full-term or late-preterm newborns with HIE, according to the above mentioned protocol. A total of 11 randomized controlled trials and 1505 infants with moderate to severe encephalopathy and evidence of intrapartum asphyxia were included in this review. Therapeutic hypothermia resulted in a statistically significant and clinically important reduction in the combined outcome of death or severe neurodevelopmental delay at 18 months of age.15
Patterns of brain injury on the magnetic resonance imaging (MRI) with different clinical presentations after the insult, and neurological outcome directly associated with neuroimaging findings and less with the immediate clinical findings, were observed in neonates with HIE.16 The need for sedation and analgesia in a newborn in the first hours after birth is one explanation for the difficulty in the clinical evaluation after HIE and decision to treat.17 In these situations, video-electroencephalogram (video-EEG) monitoring in every newborn with HIE, which is the gold standard for assessment of electrographic seizure, could be useful in the screening of newborn candidates for therapeutic hypothermia. The presence of electrographic seizures without clinical manifestation was determined by video EEG in approximately half of the newborns with HIE submitted to therapeutic hypothermia.17–19
Amplitude-integrated electroencephalogram (aEEG) has been used in a few studies to decide whether a newborn with encephalopathy is a candidate for therapeutic hypothermia.20,21 In neonates with mild HIE, a study with a small sample size showed to be more effective in identifying which patients with encephalopathy would develop severe neurological diseases.22
The use of aEEG is relevant considering that the time to decide whether a newborn is a candidate for therapeutic hypothermia is limited, and any mistakes regarding the start of such a promising treatment should be avoided; nevertheless, the aEEG is not routinely used to select candidates for this type of therapy.13–15,23
Results and prognosis after therapeutic hypothermiaHypothermia has been effective in reducing neurological sequelae, particularly in newborns with moderate HIE, and in improving the long-term prognosis of newborns with HIE. Meta-analysis studies have shown that the use of therapeutic hypothermia decreases mortality and improves prognosis regarding the neurodevelopment of infants with HIE.1,4,5
There is evidence from three large randomized trials and two small clinical trials demonstrating that induced hypothermia (33.5–34.5°C), when started within the 6-h window after the birth of full-term asphyxiated newborns, is beneficial in reducing mortality and neurodevelopmental delay assessed by the Bayley scale in the follow-up at 18 months of life.20,21,24–26 The results are better if there are well-organized protocols for hypothermia indication and induction, as well as adequate rewarming.1,24
In the context of the newborn candidate for therapeutic hypothermia, it has been observed that maternal hyperthermia is associated with high incidence of perinatal respiratory depression, neonatal seizures, cerebral palsy, and higher neonatal mortality, confirming the deleterious effect of hyperthermia. It is possible that in situations of maternal chorioamnionitis and fetal inflammatory response syndrome in utero, the result of therapeutic hypothermia is limited. In the presence of infection/inflammation in a randomized clinical trial of therapeutic hypothermia after encephalopathy secondary to bacterial meningitis, the choice of therapeutic hypothermia was ineffective.27 MRI data obtained after therapeutic hypothermia in a small prospective study of newborns whose mothers had histological chorioamnionitis demonstrated that hypothermia was less effective in this infectious condition.28
Hyperthermia after neonatal HIE is associated with higher mortality and adverse neurological outcome at 18–22 months of age and at 6–7 years of age, with lower intelligence scores and an up to 3.5-fold higher incidence of moderate to severe cerebral palsy in newborn infants with higher temperatures in the first days after birth.29,30 Therefore, high temperature after the hypoxic ischemic insult represents an additional risk factor for adverse outcomes and, avoiding hyperthermia is as important as therapeutic hypothermia in these cases.
The results of therapeutic hypothermia are strongly influenced by the severity of HIE. Several experimental and clinical studies have concluded that the neuroprotective action of therapeutic hypothermia is less effective in severe HIE, partly because the latency period is even shorter, with higher energy failure and accelerated neuronal necrosis of cortical gray matter, basal ganglia, thalamus, and serious damage to the white matter, associated with cerebral palsy at varying levels.1 A meta-analysis showed that therapeutic hypothermia was significantly protective for the outcome death and disability in cases of HIE, with better results in moderate than in severe cases. The challenge is to able to individualize the decision to initiate therapeutic hypothermia in severe cases, especially since the establishment of encephalopathy severity is difficult, imprecise, and subjective when based only on clinical evaluation.4
All patients undergoing hypothermia therapy should be followed longitudinally to establish the long-term outcome.5,13 Moreover, for the hypothermia to be effective, a high level of neonatal intensive care support is required; not all centers are capable of performing therapeutic hypothermia.
Protocol: establishing safety and efficacyRandomized clinical trials have employed two body cooling techniques in order to inhibit, reduce, and improve brain lesion evolution and neurological sequelae resulting from HIE: selective head hypothermia20 with temperatures reduced to 34.5°C, and total body hypothermia with temperature reduced to 33.5°C4,24; both techniques recommend the maintenance of hypothermia for 72h. According to ILCOR, both techniques are appropriate, and the rewarming phase must be slow and gradual, conducted over a 4-h period with an increase of 0.5°C per hour until the temperature reaches 36.5°C; this process aims to prevent complications caused by rapid rewarming.1,13,15
Selective head cooling is performed with a helmet, and total body cooling with a thermal mattress in which the infant is placed, with a servo control apparatus to regulate the mattress temperature higher or lower according to the patient's temperature.21,24 The use of ice packs is not the best method because the monitoring of thermal control is precarious, although a randomized study employed this technique in moderate HIE, recommending it as an alternative if started within 6h after the event and until the newborn is able to be transferred to a referral center to undergo therapeutic hypothermia.31
The temperature must remain above 33°C during the entire hypothermia period; temperatures below 32°C are less neuroprotective, and very severe systemic adverse effects and increased mortality have been observed with temperatures below 30°C.1,13,15 To ensure the effectiveness and safety of total body cooling, the esophageal or rectal temperature should be maintained at 33.5°C, and for selective head cooling, at 34.5°C; the temperature must be continuously monitored in both situations.13 A recent multicenter study demonstrated no benefit and suggested deleterious effects with a total body cooling protocol over a longer period of time (120h) or lower esophageal temperature (32°C) or both; the study was interrupted before the estimated sample size was achieved.32
All protocols of studies on neuroprotection after HIE with therapeutic hypothermia had similar inclusion criteria (gestational age>35–36 weeks, significant acidosis or severe depression at birth, moderate to severe encephalopathy with or without aEEG). In the majority, the exclusion criteria were age older than 6h of life, chromosomal abnormalities, and major congenital malformations or severe intrauterine growth restriction.3,20,21,24–26
Although a recent study consecutively compared 83 cases of therapeutic hypothermia, including 34 newborns submitted to selective head cooling and 49 to total body cooling, the findings of brain damage based upon MRI were more severe and frequent in the selective head cooling group, suggesting greater neuroprotection in newborns who were submitted to the total body cooling technique33; however, other studies suggest the same benefit with both techniques.1
In the absence of adequate conditions, ventilation, and hemodynamic support, as well as constant temperature monitoring at every stage, cooling, and rewarming, therapeutic hypothermia for neonatal HIE has shown unfavorable results and is not recommended, as it increases mortality in these conditions.34 Procedural safety requires months of multidisciplinary team training, with emphasis on understanding the multisystemic involvement related to perinatal asphyxia, associated with potential systemic complications of this treatment modality.35
The possible adverse effects of hypothermia therapy should be carefully monitored, such as hypotension and prolonged QT interval, thrombocytopenia, and clotting disorders in general (altered prothrombin time – PT and activated partial thromboplastin time – aPTT), skin burns and scleredema, and metabolic and electrolytic disorders.35
It is important to recognize that some events are not directly related to therapeutic hypothermia but rather to multiorgan dysfunction, which characterizes hypoxic ischemic syndrome and overlaps with the adverse effects of neonatal therapeutic hypothermia. One example is persistent pulmonary hypertension (PPH), directly associated with perinatal asphyxia and, conversely, hyperthermia can cause hemoconcentration, hyperviscosity, and pulmonary vasoconstriction.10,35 A meta-analysis of four randomized clinical trials showed no hypoglycemia in the group submitted to therapeutic hypothermia.1
These adverse events are more associated with lower temperatures than those recommended in the protocols, thus the importance of careful monitoring. Adequate knowledge of how hypothermia affects all organ systems of asphyxiated newborns that are already severely ill is critical to prevent and avoid the complications of exaggerated cooling.35
The pharmacokinetics of some drugs is altered by cooling. In an observational study, newborns with HIE treated with hypothermia and receiving normal morphine infusions had significantly higher serum concentrations of the latter when compared to the group with normal temperature. Therefore, the rate of morphine infusion must be lower than that usually recommended during therapeutic hypothermia.36
All the evidence suggests that the neuroprotective response is time-dependent (therapeutic window) and that effectiveness depends on initiating the protocol in up to 6h. In practice, it is necessary to consider at this time, that the crib should be already off and the thermometer should be inserted (if it is transesophageal, a chest X-ray is obtained to assess whether it is well placed; i.e., middle-third of the esophagus). By continually assessing body temperature, even before using the total body hypothermia mattress, the physicians ensure the safety and care quality of the protocol. After 72h, the rewarming phase should be carefully monitored, as fluctuations in cerebral blood flow are associated with brain hemorrhage after fast rewarming. Near-infrared spectroscopy (NIRS) is an effective tool to monitor brain perfusion changes in newborns with HIE submitted to therapeutic hypothermia.37
ConclusionTherapeutic hypothermia significantly reduces morbidity and mortality for many asphyxiated newborns. However, some still die or survive with sequelae at varying levels in outpatient follow-up, demonstrating the need for association with other neuroprotective strategies. The safety and effectiveness of protocols performed in reference centers must be continuously assessed. In this review, evidence is provided that supports the benefit of therapeutic hypothermia in infants with moderate encephalopathy. A future goal will be finding ways to improve therapy effectiveness.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Silveira RC, Procianoy RS. Hypothermia therapy for newborns with hypoxic ischemic encephalopathy. J Pediatr (Rio J). 2015;S91:78–83.