To build a model based on cardiometabolic indicators that allow the identification of overweight adolescents at higher risk of subclinical atherosclerotic disease (SAD).
MethodsCross-sectional study involving 161 adolescents with a body mass index ≥ +1 z-Score, aged 10 to 19 years. Carotid intima-media complex thickness (IMT) was evaluated using ultrasound to assess subclinical atherosclerotic disease. Cardiometabolic indicators evaluated included nutritional status, central adiposity, blood pressure, lipidic profile, glycemic profile, as well as age and sex. Data was presented using measures of central tendency and dispersion, as well as absolute and relative frequency. The relationship between IMT measurement (outcome variable) and other variables (independent variables) was assessed using Pearson or Spearman correlation, followed by multiple regression modeling with Gamma distribution to analyze predictors of IMT. Statistical analysis was performed using SPSS and R software, considering a significance level of 5 %.
ResultsIt was observed that 23.7 % had Carotid thickening, and the prevalence of abnormal fasting glucose was the lowest. Age and fasting glucose were identified as predictors of IMT increase, with IMT decreasing with age by approximately 1 % per year and increasing with glucose by around 0.24 % per mg/dL.
ConclusionThe adolescent at higher risk is younger with higher fasting glycemia levels.
The World Health Organization defines obesity as a chronic multifactorial condition characterized by excess body fat buildup.1 This condition's prevalence in children and adolescents is rising at an epidemic level, becoming a relevant public health issue. It is estimated that among Brazilian adolescents, roughly 11 and 4.1 million respectively have excess weight and obesity.2
Childhood obesity, besides impacting children and adolescents’ quality of life, makes way for the emergence of chronic diseases in this population, such as type 2 diabetes mellitus (DM2) and systemic arterial hypertension (SAH). It also compromises the functioning of the Sistema Único de Saúde (SUS), the Brazilian public health system, both by overload and by rising treatment costs. Data from 2022 shows that 18.9 % of adolescents serviced by SUS primary attention are overweight and 12.3 % have obesity.3
International and national policies are being implemented with the goal of reducing obesity and cardiovascular diseases (CVD) impact on public health. In Brazil, to hold childhood obesity growth and help with childhood health and nutrition, Ministério da Saúde (MS), the Brazilian government health department, published in 2021 the Estratégia de Prevenção e Atenção à Obesidade Infantil (PROTEJA), a strategy for prevention and care of childhood obesity. In the same year, it also published an instructive for SUS's primary attention workers aimed at servicing obese and overweight children and adolescents, which even included guidance on the right flux of these patients inside the country's health network, using cardiometabolic risk stratification.4
The presence of DM2, SAH, or even cardiometabolic risk factors, predisposes subclinical atherosclerosis development, which might have its origins in childhood, and lead to early mortality by CVD if no intervention is made.5 Studies suggest weight loss might revert to Subclinical Atherosclerotic Disease (SAD) in adolescents.6,7
Many articles that evaluated SAD presence in adolescents using carotid intima-media thickness (IMT) found excess weight as a prediction factor for Carotid thickening while other cardiometabolic factors added little information.8,9 Studies that evaluated only overweight adolescents found that insulin resistance, altered fasting blood glucose and elevated glycated hemoglobin are SAD predictors for this population.10–12 A single study made with excess weight Brazilian teenagers found no association between Carotid thickening and cardiometabolic risk factors.13
Understanding each risk factor's influence on the early and late stages of atherosclerosis disease, with respect of age and nutritional state, is key to CVD prevention,12 providing a more assertive approach. Based on these facts, the present study had as a goal to build a model from cardiometabolic indicators that allows for identifying from a group of overweight adolescents, which ones have a higher risk of developing SAD.
MethodsA cross-sectional study involving 161 patients with excess weight aged 10 to 19, all of whom were participants of two previous pieces of research: “Subclinical Atherosclerosis disease in school-aged adolescents: relation with PDAY score, Ultra sensible reactive C protein, and pulmonary function.” and “Impact of exergame in cardiorespiratory function on adolescents with excess weight: a randomized intervention study”. The following research were conducted respecting Helsinki Declaration principles and was approved by the ethics comity of the Universidade Estadual da Paraíba (UEPB).
Both of the cited research above had a goal to assess cardiometabolic health on middle and high school adolescents in Campina Grande, made in partnership with the city's Secretaria de Saúde, the city's health bureau, and conducted by researchers from Núcleo de Estudo, Pesquisa e Extensão (NEEPE), UEPB's Research, Study and Extension Center. NEEPE is also bound to the Public Health Post-Graduate Program of the same university and owns the databases used on both research pieces.
Studies designs can be verified in Ramos et al., 201614 and Ramos et al., 2023.15 In both studies, adolescents who showed conditions that may interfere with glucose or fat metabolism (diseases, medications, pregnancy/lactation) were excluded. Considering both works, NEEPE has a database with cardiometabolic health data about 683 adolescents. For the sake of the present study, those the authors choose to include the ones with excess weight and who made doppler ultrasonography (USG) of the carotid. From these 683 adolescents, were included in the database 161, 505 were excluded for not having excess weight and 17 for incomplete data, either for missing carotid USG or not completing all laboratory tests required for the risk assessment evaluation.
Sociodemographic, nutritional state, biochemical tests and USG data were collected inside schools and registered into a form. It's important to mention all variables were collected using the same methodology in both works.
Anthropometric data (weight, height and abdominal circumference) were collected twice (in duplicate), and the authors considered the average value between them. Weight was measured using a Tanita® digital scale with 0.1 kg precision and 150 kg max capacity. Height was assessed by a portable Avamed® stadiometer with 0.1 cm precision, and abdominal circumference was measured with a WSC® inextensible fiberglass measuring tape, same precision. All measures were made according to MS recommendations.16
For the nutritional state assessment, Body Mass Index (BMI) was calculated, and BMI Z-score was verified by age and sex using Anthroplus® software. The final classification of the nutritional state was made according to WHO: overweight (≥ z-score +1 e < z-score+2), obesity (≥ escore-z + 2).
To assess abdominal adiposity, the relation abdominal circumference (AC) / height was utilized, being considered altered if > 0.45 for girls and > 0.44 for boys.17
Blood pressure was measured using two OMRON® semi-automatic devices, models HEM 742® and HEM 705 CP, and according to recommendations from Brazilian Guidelines on Arterial Hypertension (2010; 2020). For each individual, blood pressure was measured twice, with a 1 min interval between, and the mean value was used.18
Blood for laboratory tests was collected inside schools, with subjects fasting for 12 h. Lipids (total cholesterol, HDL, and triglycerides) and fasting glucose were measured by automatic colorimetric method on a Siemens® ADVIA XT; A1c glycated hemoglobin by High-Performance Liquid Chromatography (HPLC) on a TOSOH MEDICS® G7, using the “Gold standard” method, certified by the National Glycohemoglobin Standardization Program (NGSP). LDL value was calculated using Friedewald formula and non-HDL cholesterol, using the following formula: total cholesterol – HDL.19 The TyG index was obtained using the Neperian logarithm of the product between fasting blood glucose and triglycerides (Ln [Tg 40 (mg/dL) × Fasting blood glucose (mg/dL)/2].20
IMT measurements were made by a single trained examiner, unaware of previously collected data until the moment of the procedures, which were made using two portable USG devices, one General Electric® model LogicE and one Samsung®/Medison® model MySonoU5, both in B mode, using high definition 7–12 MHz linear transductor, according to Mannheim consensus21. Longitudinal images of the common carotid artery were taken at roughly 1 cm from the bifurcation, the image in which the double line pattern was best delimited on the artery posterior wall was selected, and subsequently, five measurements on each side were obtained and registered, finally being considered the mean value of the maximum measured from each side.
All data was analyzed using statistical software: SPSS version 22.0 and R version 4.3.0. In the first phase, a descriptive analysis was made by means of measures of central tendencies and dispersion, the results being organized into graphs and tables. The studied variables distribution was verified using the Kolmogorov-Smirnov test.
To evaluate the prevalence of cardiometabolic risk factors, variables were categorized as adequate or inadequate, being considered inadequate if meeting the following: IMT above or in the 95 percentile22; total cholesterol > 170; LDL-c.>110; HDL-c, < 45; non-HDL-c >145; Triglycerides > 11019; fasting glucose (according to age group) > 86 mg/dL (10–11 years), > 93.5 (12–18 years) and > 99 mg/dL (older than 18 years)23; HbA1c ≥ a 5.7 %24; TyG index (valor ≥ 4, 70 for boys and ≥ 4, 75 for girls20; TG/HDL ratio > 325; PAS e PAD above or in the 95 percentile18, To evaluate carotid thickening (IMT above or in the 95 percentile) and the cardiometabolic risk factors, Pearson's chi-squared test was performed.
Correlation between the dependent or outcome variable (IMT) and the independent or predictor variables (age, sex, fasting glucose, A1c glycated hemoglobin, triglycerides, total cholesterol, LDL-c, HDL-c, non-HDL-c, TG) was assessed using either Pearson or Spearman correlation test, depending on each the variable's distribution.
Finally, to analyze predictor factors (independent variables) of IMT, a multiple regression model was built with Gamma distribution, belonging to the Generalized Linear Models (GLM) class. A backward procedure was made to select the variables, embedding initially all variables. Afterward, step-by-step (Stepwise), variables that had more probability of possessing no association with the outcome variable were removed. In the final model, only variables that showed a p-value < 0.20 were considered. All analyses were made with the help from R statistical software.
To measure multicollinearity, the correlation structure of predictor variables was analyzed. The variance inflation factors (VIFs) of the model's regression coefficient were used.
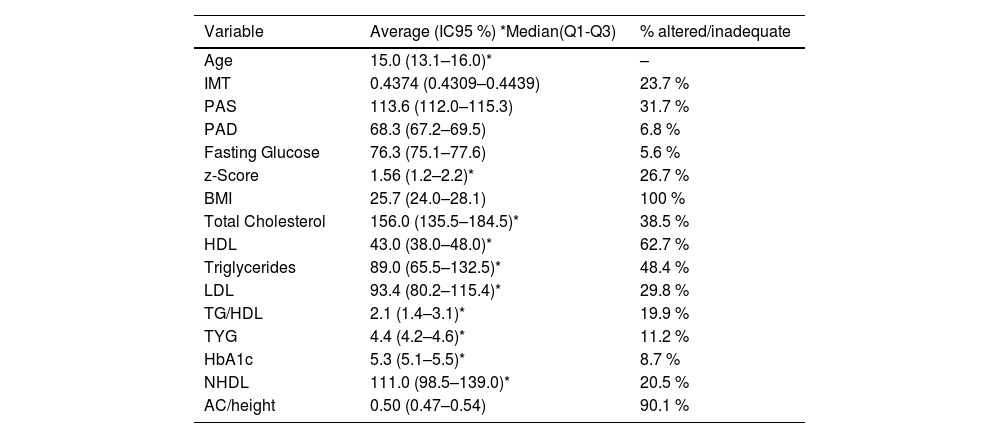
ResultsFrom all 161 adolescents evaluated, 62.1 % were female. Variables of age, nutritional state, and cardiometabolic risk indicators are shown in Table 1.
Central tendency values and dispersion of the variables age, cardiometabolic risk indicators and IMT of 161 excess weight public school adolescents in Campina Grande.
| Variable | Average (IC95 %) *Median(Q1-Q3) | % altered/inadequate |
|---|---|---|
| Age | 15.0 (13.1–16.0)* | – |
| IMT | 0.4374 (0.4309–0.4439) | 23.7 % |
| PAS | 113.6 (112.0–115.3) | 31.7 % |
| PAD | 68.3 (67.2–69.5) | 6.8 % |
| Fasting Glucose | 76.3 (75.1–77.6) | 5.6 % |
| z-Score | 1.56 (1.2–2.2)* | 26.7 % |
| BMI | 25.7 (24.0–28.1) | 100 % |
| Total Cholesterol | 156.0 (135.5–184.5)* | 38.5 % |
| HDL | 43.0 (38.0–48.0)* | 62.7 % |
| Triglycerides | 89.0 (65.5–132.5)* | 48.4 % |
| LDL | 93.4 (80.2–115.4)* | 29.8 % |
| TG/HDL | 2.1 (1.4–3.1)* | 19.9 % |
| TYG | 4.4 (4.2–4.6)* | 11.2 % |
| HbA1c | 5.3 (5.1–5.5)* | 8.7 % |
| NHDL | 111.0 (98.5–139.0)* | 20.5 % |
| AC/height | 0.50 (0.47–0.54) | 90.1 % |
Carotid thickening was observed in 23.7 % of assessed adolescents, and the most frequent cardiometabolic risk indicator was low HDL (62.7 %), followed by elevated triglycerides (48.4 %). Altered fasting glucose was the less frequent indicator (5.6 %) (Table 1).
A chi-squared test to find if associations between IMT measurements and cardiometabolic indicators were to be found, and only high fasting glucose showed an association with IMT (p = 0.013, RP = 2,7) (non-tabled data).
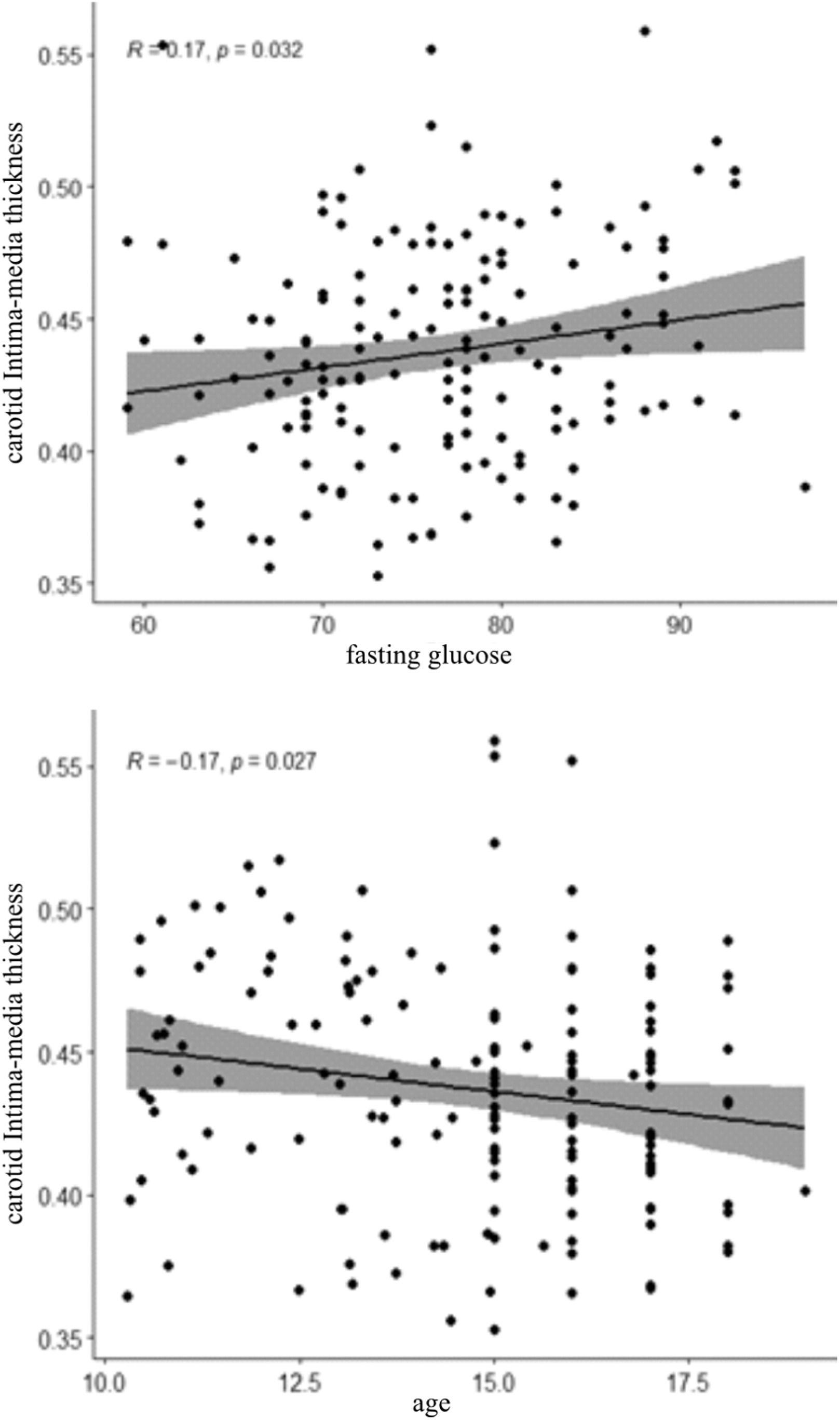
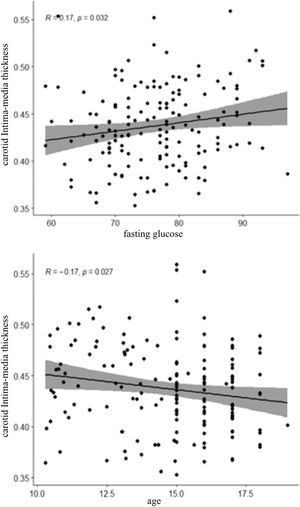
A positive correlation between IMT and fasting glucose was observed (r = 0.17; p = 0.032), and a negative correlation with age (r = - 0.17; p = 0.027) (Figure 1).
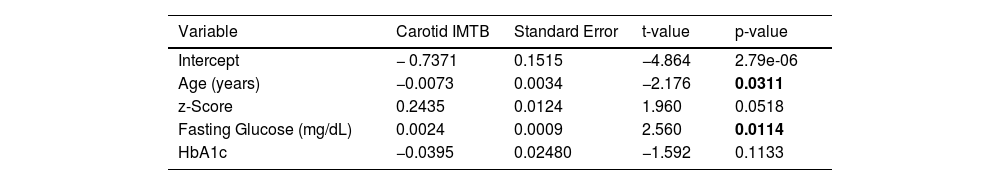
Fasting glucose (p = 0,011) and adolescents’ age (p = 0,031) were predictor factors for carotid IMT (Table 2).
The multiple regression model with gamma function shows that with higher fasting glucose in younger adolescents, higher carotid intima-media thickness (Table 2). It is estimated that the average IMT decreases by about 1 % each year and increases by about 0.24 % for each mg/dL of glucose increase.
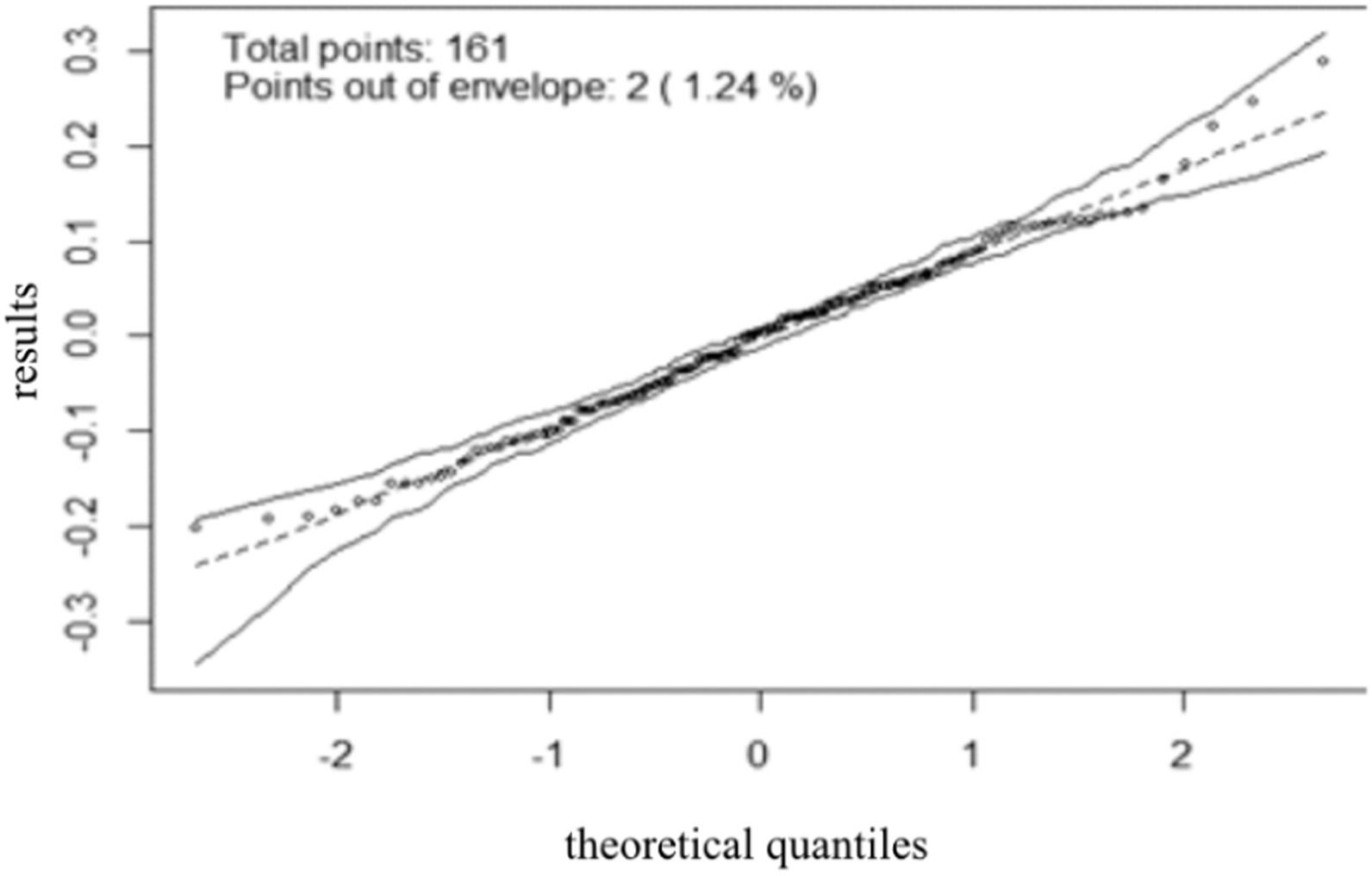
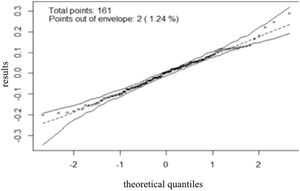
The model's residual behavior, adjusted for the data, can be observed in a graph (Figure 2). In that sense, it could be concluded that the model adjusted well to the data, as residue followed a normal behavior. In other words, the residue fell inside specified simulation envelope boundaries.
DiscussionThe present study found age and fasting glucose to be predictor factors for carotid IMT, and using a regression model, found that the higher the fasting glucose in younger adolescents, the higher the IMT.
The inverse relation observed between IMT and age could be explained by insulin resistance that happens during puberty, caused by increased sexual hormone production. Through puberty in healthy adolescents, there is a significant reduction in insulin resistance that starts in Tanner's 2nd stage, peaking in the 3rd stage, at roughly 13 years old, and finally recovering at the 5th stage26. In addition, studies show a relation between insulin resistance and increased IMT in children and adolescents:
Sanches et al.(2012),27 studying an intervention work with 66 post-puberty obese adolescents, found that insulin resistance compromises IMT reduction, which might lead to early atherosclerosis development among this group.
Asghari et al. (2018)12 analyzed 378 excess-weight subjects, children and adolescents, and showed that, in boys, an increase in one standard deviation on fasting glucose or HOMA- IR was related to an increase from 0.351 mm to 0.350 mm in IMT, respectively. They found no association in girls, however.
In the ERICA study28 37,504 adolescents aged 15 to 17 were studied to assess metabolic syndrome prevalence as well as its components, and altered fasting glucose was found to be the less prevalent factor, ratifying the present study's findings. Despite being less prevalent, its presence should be noted, since the present study found that fasting glucose was a predictor factor for larger IMT among the studied population, reinforcing other studies' findings related to glucose homeostasis alterations and carotid thickening.10,11
The present study observed that for an increase of 1 mg/dL in fasting glucose, measurements of the carotid intima-media thickness increases by 0.24 %. Similar finding was observed on a Spanish study regarding 427 with moderate cardiovascular risk in the Framingham score, in which a positive correlation was also observed between IMT and fasting glucose.29
Studies comprising of excess weight adults without diabetes (both overweight and obese) showed that even when fasting glucose is within normality, there was an association with IMT as well interventricular sept thickening. Zupo et al. showed a fasting glucose of 90 mg/dL was an independent factor for higher IMT thickening.30
Changes in glucose metabolism may precede the diagnosis of diabetes by 4 and up to 12 years. In earlier stages, insulin resistance can be compensated with insulin hyperproduction, but when the pancreatic reserve is depleted, there will be hyperglycemia and the diagnosis of metabolic disease. From this moment on, cardiovascular modifications that are adaptive to insulin resistance and cell oxidative stress damage are no longer reversible.19
It is important to highlight the use of fasting glycemia as an indicator of glucose metabolism. It may have its limitations, since some situations such as acute or chronic illnesses, the use of medication, among others, can alter its value. However, these interferences can be minimized by excluding individuals with the aforementioned conditions, as was done in the present study.
In addition, it is important to reevaluate what is considered an adequate glucose level among children and adolescents. A prospective study made with children and adolescents aged 06 to 18, showed that a fasting glucose level > 100 mg/dL was related to a higher diabetes risk among adolescents, and the higher the glucose level, the higher the risk, 93.5 mg/dL being considered as an ideal value to predict diabetes among this population.23
Had it been used glucose reference levels advocated by the Brazilian Diabetes Society in the present study, not a single adolescent of the sample would appear to have altered fasting glucose level, however, using values advocated by Yang et al. (2019),23 5.6 % of the sample showed this factor altered. Considering the cut-off-point recommended by Yang et al. (2019),23 it was found that subjects with altered glucose levels have 3x times more chance of carotid thickening (non-tabled data).
Present work brings innovative findings, like fasting glucose as a predictor for carotid thickening, and in addition to also bringing the importance of discussing adequate cut-off-points for adolescents, since at least for lipidic-profile assessment there is already a specific cut-off- point for this age group.19 This is a highly relevant fact for the sake of public health since it can help in the identification of obese adolescent susceptible to a higher risk of developing cardiometabolic diseases, especially subclinical atherosclerosis, providing guidance on the flux of these patients through health assistance networks.
Some limitations must be considered in this study, as the cross-sectional design does not allow for causality evaluation; and not assessing pre-puberty didn't allow for the classification of the subjects into pre-puberty, puberty and post-puberty, phases with great insulin resistance variation.
Yet, it is important to emphasize that few studies regarded with which are the IMT predictor factors among excess-weight adolescents, identified only one in Brazil, consisting of an evaluation of 71 overweight/obese adolescents, but it did not find an association between IMT growth and cardiometabolic factors.13
Based on the findings, it is important to develop more prospective studies focusing on both relative and absolute risk of having cardiometabolic risk factors among excess weight adolescents, with special attention to altered fasting glucose, re-evaluating even the level currently assumed to be adequate for it.
Funding institutionsUniversidade Estadual da Paraíba, Conselho Nacional de Desenvolvimento Científico e Tecnológico.
CRediT authorship contribution statementCamila M. Medeiros: Conceptualization, Data curation, Investigation, Methodology, Writing – original draft, Writing – review & editing. Carla C.M. Medeiros: Conceptualization, Methodology, Supervision, Funding acquisition. Ricardo A. Olinda: Formal analysis, Data curation. Rodrigo P.T. Vianna: Methodology, Writing – review & editing. Monica O.S. Simões: Writing – review & editing, Investigation, Data curation. Marília M. Medeiros: . Danielle F. de Carvalho: Conceptualization, Methodology, Supervision, Funding acquisition, Writing – review & editing.
Institution linked to the article: Universidade Estadual da Paraíba.