To review the epidemiology and update the scientific knowledge on the problems of development and behavior in childhood, and the recommendations for the role of the pediatrician in identifying and managing delays and disturbances in child development and mental health.
SourcesA search for relevant literature was performed in the PubMed and Scopus databases and publications of the National Scientific Council on the Developing Child.
Summary of the findingsWith the decline in the incidence of communicable diseases in children, problems with development, behavior, and emotional regulation are increasingly becoming a part of the work of pediatricians, yet many are not trained and feel uncomfortable about this extension of their role. The available screening tools for child development and behavior are reviewed, and a ‘school readiness’ checklist is presented, together with recommendations on how the pediatrician can incorporate developmental surveillance into routine practice, aware of the need for children to acquire social, emotional, and cognitive skills so that they can develop their full potential.
ConclusionsThe pediatrician's role in the future will include both physical and mental health, recognizing that social development, resilience, and emotional maturity are as important as physical growth and neuromotor skills in a child's life course.
Revisar a epidemiologia e atualizar os conhecimentos científicos sobre os problemas do desenvolvimento e do comportamento na infância, e das recomendações do papel do pediatra na identificação e conduta frente aos transtornos da saúde mental infantil.
Fontes de dadosPesquisamos a literatura relevante nas bases de dados PubMed e Scopus e em publicações do National Scientific Council on the Developing Child.
Síntese dos dadosCom o declínio na incidência de doenças transmissíveis em crianças, problemas do desenvolvimento, comportamento e regulação emocional fazem cada vez mais parte do trabalho do pediatra, mas muitos ainda não estão treinados e se sentem desconfortáveis com essa extensão do seu papel. Os instrumentos de triagem do desenvolvimento e comportamento foram revisados e uma lista de verificação da ‘prontidão escolar’ foi apresentada, juntamente com orientações sobre como o pediatra pode incorporar a vigilância da saúde mental em sua de rotina de atendimento, consciente da necessidade da aquisição das habilidades sociais, emocionais e cognitivas para que a criança possa desenvolver toda sua potencialidade.
ConclusõesO papel do pediatra no futuro irá abranger tanto a saúde física quanto a mental, reconhecendo que o desenvolvimento social, a resiliência e o amadurecimento emocional são tão importantes quanto o crescimento físico e habilidades neuromotoras no curso da vida de uma criança.
It is not an easy task being a pediatrician nowadays! But when was it easy? Pediatricians need to be constantly updated on how best to perform growth and development surveillance, the backbone of the specialty, but also on to handle chronic diseases in general, without losing the focus of their attention in relation to acute diseases within a context of sociodemographic and economic inequity.
When a child has problems in their cognitive, emotional, and/or behavioral development, and the question is raised on who or what may be responsible for the problem, most parents tend to blame the child and most professionals tend to blame the parents! However, most scientists in the area know that the problem lies in both, as well as in the genes, in the neurons, in the synapses, in the neurotransmitters, at school, in the neighborhood, and in public policies.1
The current literature indicates an increase in the so-called “new morbidities”, that is, changes in mental health, as a new challenge for pediatrics. But as early as 1957, Wolf and Smith published an article entitled “The role of the pediatrician in the mental health of children,” recognizing that the pediatrician is a key element in to monitor the child's physical, psychological, and emotional health.2 In 1967, Richmond, a North-American surgeon, defined child development as “a basic science for pediatrics”, emphasizing that “the study of cognitive and emotional, motor, and language acquisitions is what differentiates the pediatrician from all the other medical specialists”.3
After all, where does the pediatrician's mission begin and where does it end?
Epidemiology of mental health problems in childhood and adolescenceIn recent decades, a significant increase in the detection of behavioral, emotional, and developmental problems in children and adolescents has been reported worldwide,4–8 with a proportional increase also in the socioeconomically higher population groups, while maintaining the highest absolute prevalence in the poor populations.5,6,9 Some authors suggest that this situation is in a worsening trend, and this would only be the tip of the iceberg. The recognition of the children's obesity epidemic as a major risk for the physical and mental health of the young generation, is undeniable and “clearly” evident. However, the increase in mental health problems among the pediatric population is less “visible”, but equally threatening.
Changes in development, such as language and learning disorders, learning disabilities, attention deficit and hyperactivity disorder (ADHD), autism spectrum disorder (ASD), and other behavioral problems, are already among the five most frequent causes of limitation of usual activities in children due to chronic conditions in the United States, even more than asthma or respiratory diseases in general.5,6,10
Several factors are related to this increase in prevalence, such as changes in the diagnostic criteria and greater knowledge of the population and the medical community about these disorders, especially of Pediatricians. Another contribution came from the current knowledge on the multiple determinants of child development: both biological (such as genetic predisposition) and environmental factors, as well as early experiences, which influence the developing brain, including changes in the lifestyle of families, whether in urban or rural areas.7,11,12
The American Academy of Pediatrics (AAP)10 has tried to emphasize this problem, which is common in childhood, but often goes undetected and untreated. Recent estimates indicate that approximately 11–20% of the United States pediatric population will show, at any time of its development, emotional or behavioral problems, defined by the Diagnostic and Statistical Manual of Mental Disorders – 5th Edition (DSM-V) criteria. This high prevalence is already observed in children aged 2–5 years and, among adolescents, 37% and 39% will have been diagnosed with a behavioral or emotional disorder by the age of 16 years.
In 2012, Martini et al.13 published a manual by the American Academy of Child and Adolescent Psychiatry, aiming to integrate the work of the pediatrician and the professional who specializes in children's mental health, as there is a high prevalence of these disorders in the United States and only about 20% of these children receive treatment. It is noteworthy that half of all mental illnesses in adults begin in adolescence; despite being a critical moment of childhood development, there is an average delay of 8–10 years between symptom onset and the beginning of adequate treatment.
A longitudinal study carried out in southern Brazil showed that approximately 13% of children aged 6 years had a diagnosis of mental disorder, according to the diagnostic criteria of DSM-IV; the most frequent ones were anxiety disorders (8.8%), followed by ADHD (2.6%), oppositional defiant/conduct disorder (2.6%), and depression (1.3%), demonstrating the early onset of mental illness and the need to initiate an intervention in childhood.14
Fleitlich and Goodman,15 in a study carried out in Rio de Janeiro with children and adolescents aged 7–14 years from different socioeconomic levels, found that the factors most strongly associated with probable psychiatric disorders in this population were poverty, maternal mental illness, and family violence. Another study, carried out in São Paulo, showed the difficulty for families of children with persistent mental disorders to have access to mental health services; the parents’ lack of knowledge about these disorders was one of the main barriers to treatment.16 It is also evident the shortage of mental health professionals (development and behavior pediatrician, neuropediatrician, and childhood and adolescence psychiatrist) and of services that assist children and adolescents with less severe mental health disorders, which comprise approximately 90% of cases, showing how crucial a better training of pediatricians in this area is.17
As a coping strategy, the Children and Adolescent Psychosocial Care Centers (Centro de Atenção Psicossocial Infantil-Juvenil [CAPSi]) were implemented in Brazil, consisting of a physician (psychiatrist, neurologist, or pediatrician specialized in mental health), a psychologist, an occupational therapist, a speech therapist, and a social worker, among others. The focus of the CAPSis, however, is on the most severe behavioral and emotional disorders.17–19
The future of pediatrics: knowledge of child development and mental healthThe World Health Organization (WHO) shows that the high frequency of cognitive and social–emotional development disorders is a worldwide problem. It is believed that the percentage of affected children in less affluent countries is even more severe, partly due to the obvious gap in scientific knowledge that is relevant for children at risk and their families.9,20
In 2011, the Grand Challenges in Global Mental Health Initiative (GCGMHI)21 defined the priorities in mental health for the next 10 years, emphasizing the importance of a longitudinal view of health, as many mental health disorders start in childhood and require a more ecological approach, based on the community and including family care in addition to the child care. To increase family access to interventions based on scientific evidence should be a priority, especially in low- and middle-income countries.
Despite the recognized importance of the pediatrician's role as the child's caregiver and advocate, why do many pediatricians currently refrain from advising the parents? We should expose the real needs of children to develop healthily, such as: establishment of appropriate routines and diet, sleep hygiene, sphincter control training, and especially the importance of a loving attitude of parents with sensory and “proactive” interaction, but also setting limits, including those regarding media exposure. The pediatrician is one of the first professionals that can intervene in these situations, screening families and children at risk, advising on appropriate parenting style, and referring them to specialized services when necessary.22–24
There are several reasons that make it difficult for pediatricians to feel responsible as the “first line” professional to raise the diagnostic suspicion (even if only on clinical grounds) of ADHD, ASD, learning disorders, food and sleep disorders, depression, substance abuse, or other behavioral changes. Among these barriers are the lack of confidence of the pediatricians on their capacity to diagnose and monitor these children; lack of time, in stressful day-to-day activities, to use validated screening tools; lack of tools that have been validated in Brazil and lack of practical and effective national manuals to guide them in this area; severe shortage of professionals and specialized services in child development (development and behavior pediatricians, childhood psychiatrists, and neurologists) to refer children with developmental and behavioral difficulties; lack of interaction between different healthcare, education, and social assistance professionals, which are directly linked to development and behavior; and finally, lack of remuneration and adjustment of working hours to perform this screening adequately.10,25 These difficulties frustrate and overwhelm the pediatrician; it is important to note that, for the adequate handling of developmental and behavioral problems, it is important to “think outside the box”, i.e., promote a paradigm shift.
The AAP10–12,25–27 has made a great effort to introduce mental healthcare in pediatrics, by publishing several articles and manuals on the subject, emphasizing the importance of continuing education and proposing innovations to the curriculum of the undergraduate course in medicine and pediatric residency. For a shift in paradigm to really occur it is necessary to change skills, knowledge, and attitudes; to acquire expertise that overlap those of professionals in children's mental healthcare area, by raising diagnostic suspicion early, as well as promoting a healthy lifestyle, providing behavioral guidelines, and decreasing mental problems by strengthening the resilience of the children and their families.11 In other words, pediatricians need to be familiar with the normal variations of child development to differentiate them from the cognitive, behavioral, and/or emotional alterations, and they should always consider the context in which the child lives, bearing in mind that children demonstrate their mental health problems in peculiar ways, often quite differently from adolescents and adults.28
A recent study carried out in the United States with children and adolescents aged 2–21 years, found that although the primary care physician monitored alone four in ten children with ADHD and one-third of those with other mental health problems, they prescribed more psychostimulants and alpha-agonists than child psychiatrists. The shortage of child development experts may have contributed to a higher proportion of ADHD diagnoses, rather than a diagnosis of anxiety and mood disorders. The study emphasizes the importance of collaborative work between pediatricians, developmental and behavioral pediatricians, psychiatrists, and childhood neurologists, by applying updated knowledge for adequate pediatric training.29
Neuroscience update and behavioral scienceMental health is the basis for achieving all the other skills of human development.28 Worldwide, there are clear indications that the increase in early detection of child development alterations and consequent early onset of stimulation, are key priorities, initially for the well-being of children and their families, but later for the whole community, since “the future of any society depends on its ability to adopt strategies for better development of the next generation.”4
Studies in neuroscience, molecular biology, epigenetics, and social and behavioral sciences have shown that humans develop according to our genetic programming, but with great influence of early life experiences; this interaction between biological and environmental factors is the basis for mental health. Early experiences shape the architecture of the brain and modify its processes, transiently or permanently.4,28,30 It is well known that the brain is more plastic during intrauterine life and early childhood, being much more vulnerable to risks, as well as more “pliable” through appropriate stimuli.4,24,28,30–32 However, the brain is not infinitely plastic and the earlier and more prolonged the negative experiences, the more resistant the brain becomes to interventions.4 The impact of experiences is not only expressed in early childhood development, but is also closely linked with future school learning, physical health throughout life, economic productivity, and citizenship formation.31
The experiences that influence child development are multiple, and it must be reinforced that the affectionate and protective relationship between the child and parents, caregivers, relatives and teachers is crucial for an adequate socio-emotional and cognitive development.4 Conversely, prolonged stress caused by extreme poverty, wars, exposure to violence, sexual abuse, parental mental illness (especially maternal depression and drug use by parents), among other causes, associated with lack of protective interaction with adults, can lead to excessive and prolonged activation of the child's stress response system. This activation includes persistent increase in stress hormones, which in turn, decrease the connectivity of specific brain areas, such as the prefrontal cortex and the limbic system (amygdala and hippocampus), impairing both cognitive development and learning of social skills.4,24,31–33
To provide stimulating environments, not only in the neuromotor and cognitive aspects, but also in the socio-emotional development, at home, daycare, or early childhood education schools, is one of the greatest responsibilities of society.34 From the economic standpoint, it has been shown that early investments in social skills and mental health (such as in the capacity of attention, persistence, motivation and self-control) have a high cost–benefit ratio due to the impact on the future productivity of the country, enhancing the cognitive development of adolescents and adults, as demonstrated by better school performance and decrease in adolescent crime and pregnancy rates, especially among the socioeconomically disadvantaged population.35–37
Among these stimuli, it is important to focus on executive functions, highlighting the working memory, impulse control, ability to plan and maintain one's attention on certain activity, and mental flexibility. Humans are not born with these skills, but only with the potential to learn them, and this learning depends on the experiences from birth to adolescence. Executive functions are extremely important, both for cognitive and social/emotional acquisitions.
The rudimentary executive skills can be observed as early as at the end of the first year of life, but they become more evident after the third year, when the child can already follow a two-step command, make simple choices, and maintain their attention on a particular activity for a certain period of time, among others. Executive functions, however, develop and strengthen until early adulthood, and are associated with educational and professional success, but also with social, emotional, and moral development. Social and imaginative playing and positive child–adult relationships lead children to develop their executive skills and better achieve their independence.34,35
Unstructured playing (not directed by an adult) is a fundamental aspect of the physical, cognitive, social, and emotional processes in childhood; pediatricians need to previously advise the families of their young patients about this subject.27 With changes in lifestyle; the entry of women into the labor market without the concomitant increase in the father's help in the home; the rush to adapt the child to the rhythm of adults; social and school pressures as in early childhood, for the final result based on knowledge (reading and logical reasoning); and the mass marketing of extracurricular products make parents believe that the more children have structured activities, the better the development.
Very often, the precious interaction time between children and their parents (caregivers) is used to organize special activities and transportation of children from one activity to another. Despite the fact that playing (and having some free time for the adolescent) is essential for learning and mental health, children are increasingly overloaded with directed activities, at the expense of creative and active activities, often developing signs of stress, anxiety, and somatizations.27
Unfortunately, many educational institutions in Brazil that provide services to infants and preschoolers prioritize the training of cognitive abilities, reducing the time and investment in socio-emotional skills. And when the child loses the focus of attention, their emotional and behavioral control, and cannot make choices or follow the adult's instructions, these behaviors are interpreted as being voluntary. This is evidenced by the increasing expulsion of children attending preschools.38
Moreover, many children can only attend preschool after the age of 4 and that age is not early enough to protect children living in hazardous environments. Ideally, mothers who are most vulnerable should receive support at the start of the pregnancy.31,32
A devastating aspect for child development, particularly for the acquisition of executive functions, is neglect, defined as the lack of attention, responsiveness, and protection from caregivers that is sufficient and adequate to the child's age and needs. Neglect is clearly the most common form of abuse and can be expressed as physical or attention neglect, psychological neglect, and neglect of health or education. They often occur concurrently, and young children victims of severe and chronic neglect have worse development than victims of other types of abuse. This type of neglect leads to several alterations in growth (decrease of the brain and body growth) and motor, cognitive, language, and learning development, as well as a higher prevalence of mental disorders such as anxiety, depression, personality disorder, low self-esteem, and difficulty when interacting with peers.39
Conversely, medical literature has shown promising intervention models, reducing the negative impact of neglect, that is, improving cognitive, attention, and memory functions and reducing behavioral and emotional difficulties. These interventions need to include the family (as parental mental health problems are often associated), be long-lasting, and start as early as possible, as well as use methods with scientific evidence of efficacy. The question that remains is: how can we, as pediatricians, ensure that all children receive the care they need? Unquestionably, we need to change our ways to identify neglect and advocate on behalf of children, even if it means stepping out of the traditional boundaries of medical care.39
But science also shows aspects that favor development, such as resilience, which is understood as a positive adaptive response to adversities. Resilience is not only a personal or immutable characteristic, but also rather the result of the interaction of multiple protective environmental factors and a highly responsive biological system. Therefore, it can be strengthened through positive interactions of reciprocity between the child and the caregiver. It is important to remember that not all stress is harmful to children, and learning to deal with routine obstacles of life, the so-called positive stresses, allows for the development of executive functions and self-control skills.35
As an example of resilience promotion, children need adults to believe unconditionally in their potential to become compassionate, generous and creative individuals. The Positive Youth Development Movement40 suggests fundamental milestones, called “The 7 Cs: the essential building blocks of resilience”.
Competence: When we notice what young people are doing right and give them opportunities to develop important skills, they feel competent. We undermine competence when we do not allow young people to recover themselves after a fall.
Confidence: Young people need confidence to be able to navigate the world, think outside the box, and recover from challenges.
Connection: Connections with other people, schools, and communities offer young people the security that allows them to stand on their own and develop creative solutions.
Character: Young people need a clear sense of right and wrong and a commitment to integrity.
Contribution: Young people who contribute to the well-being of others will receive gratitude rather than condemnation. They will learn that contributing feels good and may, therefore, more easily turn to others and do so without shame.
Coping: Young people who possess a variety of healthy coping strategies will be less likely to turn to dangerous quick fixes when stressed.
Control: Young people who understand privileges and respect are earned through demonstrated responsibility will learn to make wise choices and feel a sense of control.
Pediatricians have now more access to information about major cognitive and socio-emotional development disorders, such as intellectual impairment, ADHD, ASD, learning disorders, anxiety, and mood disorders. There are two aspects that should be included in the routine pediatric follow-up, and will be briefly assessed: the difficult child and that with sleep disorder.
One of the most frequent complaints in pediatric offices is the difficulty that parents, caregivers, and teachers have dealing with children with difficult temperaments, without neurodevelopmental alterations. They can show low threshold for frustration with challenging, stubborn, pushy, restless behavior. They are easily irritable or even aggressive, but can also be very timid, fearful, or oversensitive, with several sensory difficulties, especially regarding food, clothing, and sounds. They are often intense in their feelings or behavior, requiring much attention from adults and often causing family, school, and peer conflicts. These children tend to put adults in check and leave them confused, frustrated and insecure about the child's intentionality and their parental capacity to care for them.
Undoubtedly, as the first recommendation for parents, pediatricians should show empathy and praise the concern of the family, in addition to explaining the parents’ misperception in relation to the child's negative intent. The limits and the rules must be direct, coherent, and consistent; as such, they must be true for all (father, mother, and caregivers) and be routinely used.
The pediatric intervention should support the parents and make it clear that they, as the adults in this relationship, are responsible to maintain the calm, safety, and predetermined rules, establishing them and clarifying the child about the limits and consequences of breaking them. As previously mentioned, it is paramount that parents understand and accept that experiencing the positive stress of frustration and consequently learning to constructively deal with this situation is essential to strengthen their child's resilience. The negative reinforcement, such as physical or moral punishments, do not bring results, often worsening the situation.35,41
It is very important that, depending on the severity, frequency and the consequences of inappropriate behavior, pediatricians differentiate a child with difficult temperament from one with neuropsychiatric disorders [ADHD, ODD (oppositional defiant disorder), GAD (generalized anxiety disorder), among others], who requires adequate diagnostic assessment and treatment.
As for sleep disorder, it has a high occurrence, being present in 25% of children and adolescents. Among those with intellectual impairment, developmental disorders (ADHD and ASD), or other psychiatric disorders, the percentage varies between 50% and 80%. Parenting can profoundly influence the child's sleep pattern, i.e., lack of routine, difficulty to set up limits, and giving too much attention to children reluctant to fall asleep, greatly increase the chance of establishing behavioral insomnia, which, unlike what is thought, can persist into adulthood. Furthermore, the parents’ knowledge, attitudes, and emotional state often determine if they consider the child sleep pattern to be a problem or not.42
It is important to remember that it is the pediatrician's role to ask questions about this pattern during consultation, considering that parents often do not report problems with sleep, as they think it is “normal” for children to have a sleep rhythm compatible with that of an adult and are unaware that insufficient sleep in childhood can cause stunting and impaired concentration and learning.
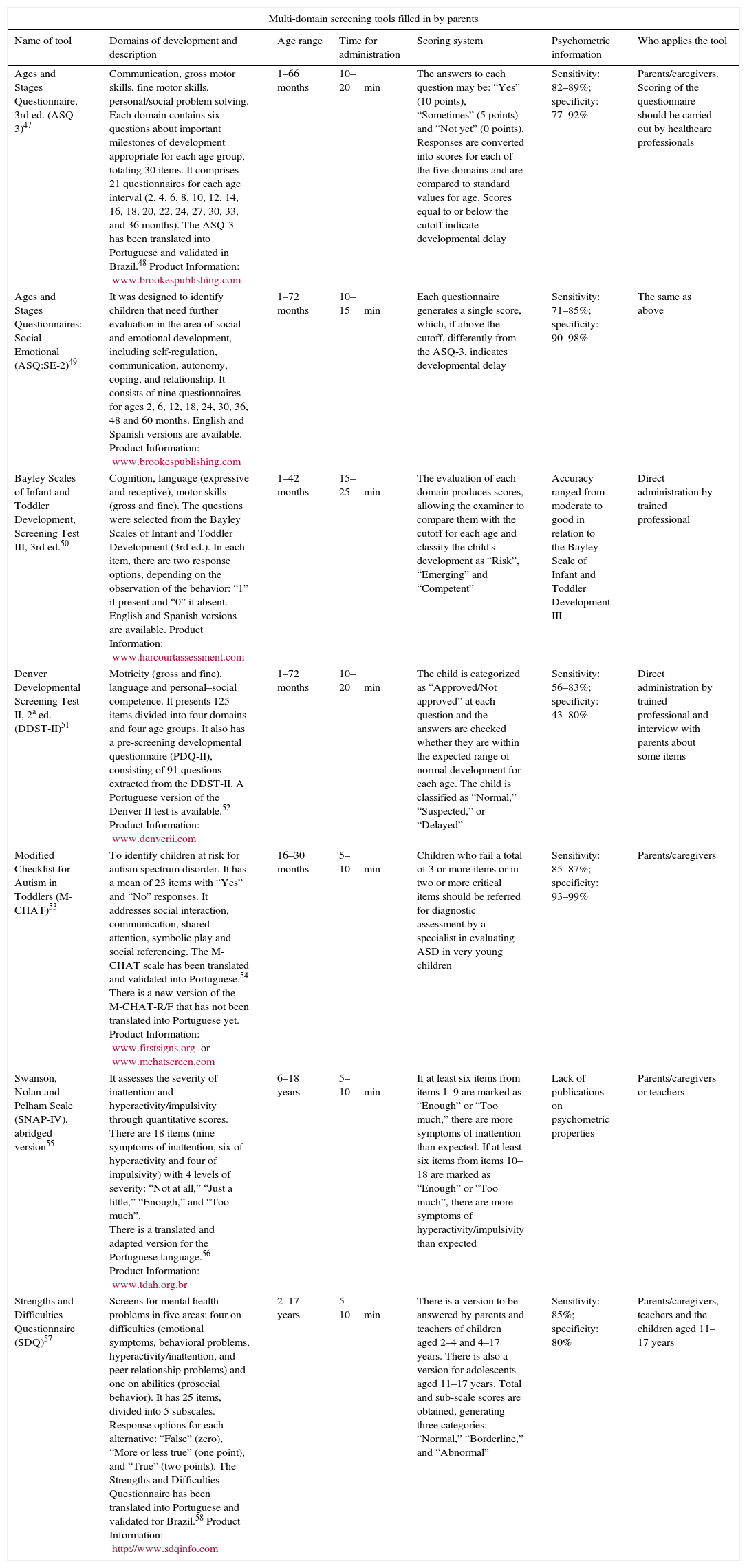
The following section describes the development and mental health screening/evaluation tools most often used in Brazil.
Child development screening tools most often used in BrazilDespite the recognized importance of detecting developmental and behavioral disorders in children as early as possible, this practice is not yet part of the routine of most pediatric consultations. Several international entities such as the AAP, the Society for Developmental and Behavioral Pediatrics, the American Academy of Child and Adolescent Psychiatry, the School Children Mental Health in Europe (SCMHE) Project, and the World Health Organization (WHO), among others, have tried to reduce these barriers through the production of documents for the continuing education of pediatricians.10,13,25,43,44 These difficulties are similar to those observed in the implementation of the use of screening tools used in child development monitoring, suggested by the AAP (2006).10 One of the lessons learned during this process was that the use of screening tests should be routine in pediatric practice and need to cover the neuromotor, cognitive, and socioemotional developments.
Many tools assess the neuromotor and social–emotional development as independent constructs, identifying alterations in the development of expressive and receptive language, gross and fine motor skills, problem-solving ability, and cognition separately. However, to evaluate the behavior and emotional development, it is necessary to include more subtle skills, such as emotional regulation, inhibitory control, attention/concentration, ability to interact verbally and nonverbally, and mood.
The AAP45 recommends that development monitoring should be continuous and carried out in all health promotion consultations. This process, in addition to the careful observation of the development history and context, includes listening to parents, as they are usually the first to recognize possible signs of developmental delay, and any reported concerns must always be taken into account. However, the lack of concern does not necessarily mean that the child's development is processing adequately. If any alterations are observed, a screening test must be performed.
The AAP45 also recommends that the screening for developmental delay should be performed in all children through standardized tools, at 9, 18, 24, or 30 months, regardless of the identification or not of a delay during development monitoring. The administration of a specific screening tool for autism should be performed in all children between 18 and 24 months; if the results are suggestive of ASD, the child should be referred for diagnostic evaluation by a specialist in the area.46Table 1 shows the screening tools most frequently used in the clinical assessment of children's development in Brazil.47–58
Screening tools used for child development assessment in Brazil.
| Multi-domain screening tools filled in by parents | ||||||
|---|---|---|---|---|---|---|
| Name of tool | Domains of development and description | Age range | Time for administration | Scoring system | Psychometric information | Who applies the tool |
| Ages and Stages Questionnaire, 3rd ed. (ASQ-3)47 | Communication, gross motor skills, fine motor skills, personal/social problem solving. Each domain contains six questions about important milestones of development appropriate for each age group, totaling 30 items. It comprises 21 questionnaires for each age interval (2, 4, 6, 8, 10, 12, 14, 16, 18, 20, 22, 24, 27, 30, 33, and 36 months). The ASQ-3 has been translated into Portuguese and validated in Brazil.48 Product Information: www.brookespublishing.com | 1–66 months | 10–20min | The answers to each question may be: “Yes” (10 points), “Sometimes” (5 points) and “Not yet” (0 points). Responses are converted into scores for each of the five domains and are compared to standard values for age. Scores equal to or below the cutoff indicate developmental delay | Sensitivity: 82–89%; specificity: 77–92% | Parents/caregivers. Scoring of the questionnaire should be carried out by healthcare professionals |
| Ages and Stages Questionnaires: Social–Emotional (ASQ:SE-2)49 | It was designed to identify children that need further evaluation in the area of social and emotional development, including self-regulation, communication, autonomy, coping, and relationship. It consists of nine questionnaires for ages 2, 6, 12, 18, 24, 30, 36, 48 and 60 months. English and Spanish versions are available. Product Information: www.brookespublishing.com | 1–72 months | 10–15min | Each questionnaire generates a single score, which, if above the cutoff, differently from the ASQ-3, indicates developmental delay | Sensitivity: 71–85%; specificity: 90–98% | The same as above |
| Bayley Scales of Infant and Toddler Development, Screening Test III, 3rd ed.50 | Cognition, language (expressive and receptive), motor skills (gross and fine). The questions were selected from the Bayley Scales of Infant and Toddler Development (3rd ed.). In each item, there are two response options, depending on the observation of the behavior: “1” if present and “0” if absent. English and Spanish versions are available. Product Information: www.harcourtassessment.com | 1–42 months | 15–25min | The evaluation of each domain produces scores, allowing the examiner to compare them with the cutoff for each age and classify the child's development as “Risk”, “Emerging” and “Competent” | Accuracy ranged from moderate to good in relation to the Bayley Scale of Infant and Toddler Development III | Direct administration by trained professional |
| Denver Developmental Screening Test II, 2a ed. (DDST-II)51 | Motricity (gross and fine), language and personal–social competence. It presents 125 items divided into four domains and four age groups. It also has a pre-screening developmental questionnaire (PDQ-II), consisting of 91 questions extracted from the DDST-II. A Portuguese version of the Denver II test is available.52 Product Information: www.denverii.com | 1–72 months | 10–20min | The child is categorized as “Approved/Not approved” at each question and the answers are checked whether they are within the expected range of normal development for each age. The child is classified as “Normal,” “Suspected,” or “Delayed” | Sensitivity: 56–83%; specificity: 43–80% | Direct administration by trained professional and interview with parents about some items |
| Modified Checklist for Autism in Toddlers (M-CHAT)53 | To identify children at risk for autism spectrum disorder. It has a mean of 23 items with “Yes” and “No” responses. It addresses social interaction, communication, shared attention, symbolic play and social referencing. The M-CHAT scale has been translated and validated into Portuguese.54 There is a new version of the M-CHAT-R/F that has not been translated into Portuguese yet. Product Information: www.firstsigns.org or www.mchatscreen.com | 16–30 months | 5–10min | Children who fail a total of 3 or more items or in two or more critical items should be referred for diagnostic assessment by a specialist in evaluating ASD in very young children | Sensitivity: 85–87%; specificity: 93–99% | Parents/caregivers |
| Swanson, Nolan and Pelham Scale (SNAP-IV), abridged version55 | It assesses the severity of inattention and hyperactivity/impulsivity through quantitative scores. There are 18 items (nine symptoms of inattention, six of hyperactivity and four of impulsivity) with 4 levels of severity: “Not at all,” “Just a little,” “Enough,” and “Too much”. There is a translated and adapted version for the Portuguese language.56 Product Information: www.tdah.org.br | 6–18 years | 5–10min | If at least six items from items 1–9 are marked as “Enough” or “Too much,” there are more symptoms of inattention than expected. If at least six items from items 10–18 are marked as “Enough” or “Too much”, there are more symptoms of hyperactivity/impulsivity than expected | Lack of publications on psychometric properties | Parents/caregivers or teachers |
| Strengths and Difficulties Questionnaire (SDQ)57 | Screens for mental health problems in five areas: four on difficulties (emotional symptoms, behavioral problems, hyperactivity/inattention, and peer relationship problems) and one on abilities (prosocial behavior). It has 25 items, divided into 5 subscales. Response options for each alternative: “False” (zero), “More or less true” (one point), and “True” (two points). The Strengths and Difficulties Questionnaire has been translated into Portuguese and validated for Brazil.58 Product Information: http://www.sdqinfo.com | 2–17 years | 5–10min | There is a version to be answered by parents and teachers of children aged 2–4 and 4–17 years. There is also a version for adolescents aged 11–17 years. Total and sub-scale scores are obtained, generating three categories: “Normal,” “Borderline,” and “Abnormal” | Sensitivity: 85%; specificity: 80% | Parents/caregivers, teachers and the children aged 11–17 years |
It is important to bear in mind the dynamic nature of child development, as this process does not occur in a linear fashion, but is characterized by peak, stationary and, sometimes, regression phases. However, many children with developmental disorders are not identified early and the problems are perceived later due to poor school performance, being a lost opportunity for establishing an early intervention.
Required skills for school readinessThe study of child development has shown that children's early experiences can greatly affect their learning and school performance. The three areas of skills required for children to demonstrate school readiness are: intellectual ability, motivation to learn, and good social–emotional development. However, in order to develop these skills, it is vital that children receive the necessary external support. This support depends on the state of physical and mental health and well-being of families, but it can be influenced, and the pediatrician has an important role in supporting families to identify children with difficulties during the developing of these core competencies.59
School readiness is a complex construct consisting of several characteristics of the child, including physical health and well-being, social competence, emotional maturity, and language and communication capacity, as well as cognitive skills. Each of these aspects includes several skills: (a) physical well-being includes motor development, health and growth status, and presence or absence of physical disabilities; (b) social and emotional development includes the ability to take turns or reciprocity, cooperation, empathy, and ability to express their emotions; (c) among the characteristics that influence learning are enthusiasm, curiosity, temperament, culture, and values; (d) the development of language and fine motor skills includes adequate development of the ability to listen and understand, to speak with appropriate vocabulary, as well as the initial reading, writing and drawing skills; and (e) the general and cognitive skills, including the letter/sound association, spatial relationships, and numerical concepts.60
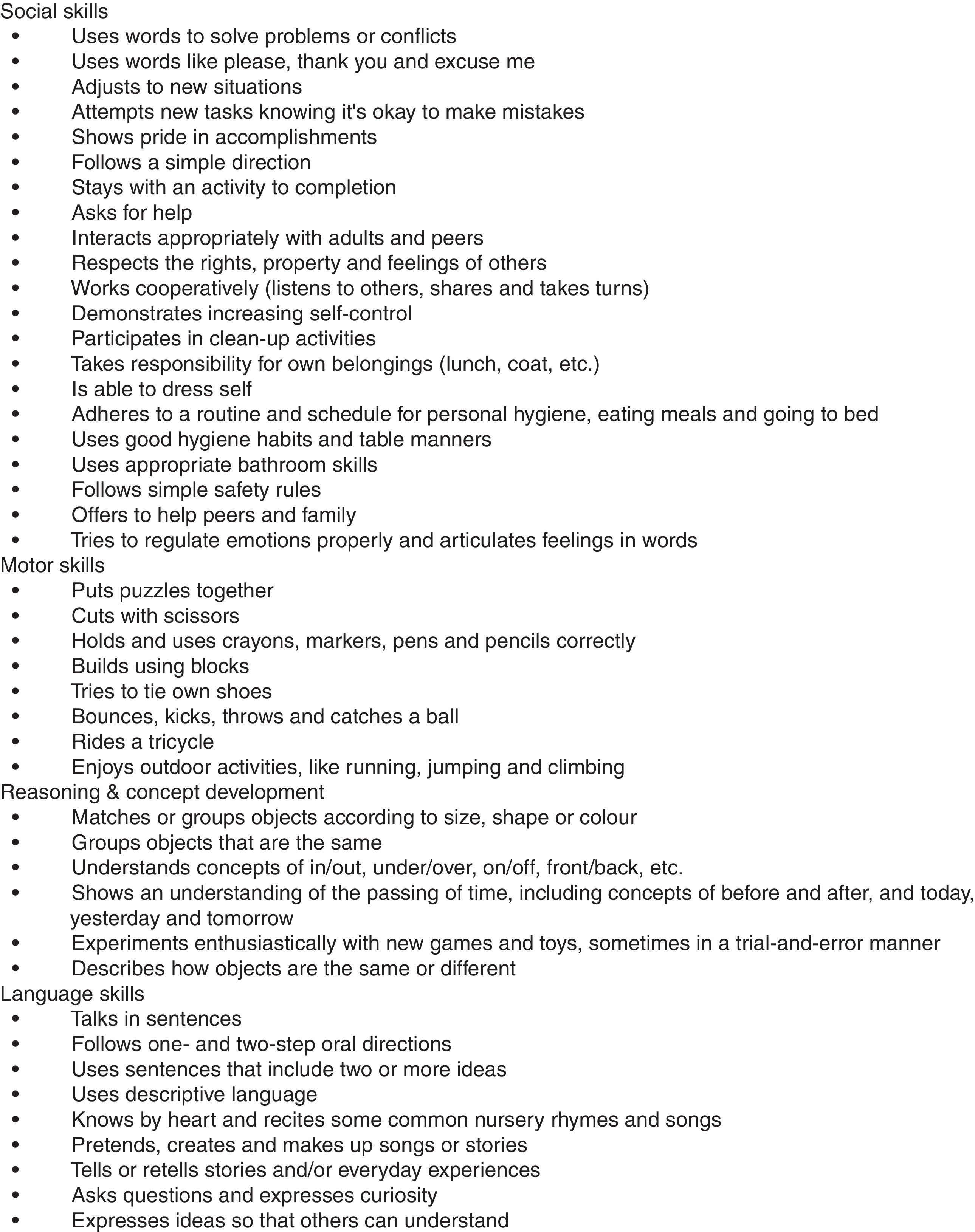
The checklist shown in Fig. 1 from the original School Readiness Checklist61 is an example of a comprehensive guide of the necessary skills that demonstrate the child is prepared to start formal education, i.e., to enter the first year of elementary school. There are several school readiness checklists, representing the different types of skills that children need to acquire as a prerequisite to benefit from school learning. All items are essentially normative, i.e., they allow the comparison of each child at age 5 with another “typical” child of the same age. However, these checklists should not be considered as screening tests or used as cutoffs for inclusion or exclusion from school, but should be understood as guidelines to help parents understand the scope of the complex skills needed for school readiness, and remind them that the child's success in school is not just a matter of memorizing the alphabet or being able to count to 100! “Readiness” is also a term related to the culture and family environment, and available resources for children in their communities.62
Although the family environment in which the child lives is the strongest predictor of school readiness, attending day care centers, nurseries, or high-quality preschools, can compensate for the lack of opportunity to learn and develop at home. Early education programs should improve physical, intellectual and social skills of the child, contributing to overall development and readiness for school.59 Many children begin their school career already with limitations in their social–emotional, physical, and cognitive development,62 which may have been negatively influenced by the lack of support and knowledge of parents about the importance of stimulation in the early years of life. The monitoring of high-risk groups, such as low birth weight and/or preterm babies, is particularly important, as studies show that early intervention may prevent developmental delay and decrease school absenteeism.63
The child's socio-emotional skills can directly affect the relationship between the peers and between children and adults, as well as individual learning and the dynamics in the classroom. Underdeveloped interpersonal skills lead to conflicts with teachers and peers, resulting in school failure and, possibly, social exclusion.64
Cognitive skills are also important predictors of educational success. A meta-analysis of six longitudinal studies in the United States, United Kingdom, and Canada concluded that early mathematical skills (logic) had the greatest predictive power in subsequent educational success, followed by reading skills (language) and maintaining attention.65
Many pediatricians do not consider that their role includes assessment and monitoring of emotional or behavioral problems. However, these problems are associated with delayed motor and language development, as well as lack of skills to participate in games and group play, even considering cultural and demographic differences. A study by Montes et al.66 in children with behavioral problems found school readiness developmental delay of 0.6–1.0 standard deviations in several development tests when compared with children without behavior problems, and that parents of children with behavior problems were five times more likely to report that their child was not ready for school.
ConclusionsThe questions raised earlier in this article can be answered with the understanding that pediatricians can and must help in the overall development and school readiness of children by promoting a good parent/baby relationship; good physical and nutritional health; sleep, food, and media exposure routines; highlighting the importance of play; providing anticipatory guidance to parents; and identifying children and families at risk. That requires integrating the systematic monitoring of development and behavior to our regular practices. It is also necessary to be aware of psychosocial risks, such as family violence, maternal depression, and substance abuse, and to increase the contact with school, community, and family support services.
Finally, a pediatrician's work is complete when the family understands that nothing is more important for children than maintaining reciprocity and affection interactions, helping children understand what is expected from them and trying to understand their expectations; positively reinforcing their successes of everyday life (it does not mean giving gifts!) through praise and affection; reading, playing and singing together as daily family activities; and especially, offering them stability and affectionate care.
Conflicts of interestThe authors declare no conflicts of interest.
The authors would like to thank Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) for the productivity grant to Marilia Lima (process n. 307633/2013-6).
Please cite this article as: Eickmann SH, Emond AM, Lima M. Evaluation of child development: beyond the neuromotor aspect. J Pediatr (Rio J). 2016;92(3 Suppl 1):S71–83.