To evaluate the resting energy expenditure, growth, and quantity of energy and macronutrients intake in a group of preterm newborns.
MethodsThe cohort study was performed with appropriate and small for gestational age preterm infants (birth weight lower than 1500g or gestational age<32 weeks). Resting energy expenditure was measured using indirect calorimetry on the 7th, 14th, 21st, and 28th days of life, and at discharge. Length, head circumference and body weight were assessed weekly. Nutritional therapy was calculated during the hospital stay and the information for each type of food was recorded in software that calculates the total amount of energy and macronutrients.
Results61 preterm infants were followed; 43 appropriate and 18 small for gestational age infants. There was no statistical difference for resting energy expenditure between the groups, and it increased from the first to the fourth week of life (appropriate: 26.3% and small: 21.8%). Energy intake in the first two weeks of life was well below the energy requirement.
ConclusionConsidering that the results demonstrate high energy expenditure during the first weeks of life, there is an evident need to provide the best quality of nutrition for each child in the first weeks of life so that preterm infants with or without intrauterine growth restriction can achieve their maximum potential for growth and development.
Avaliar o gasto energético de repouso, o crescimento e a quantidade ofertada de energia e macronutrientes em um grupo de recém-nascidos pré-termo.
MétodoFoi feito estudo de coorte com recém-nascidos pré-termo adequados e pequenos para a idade gestacional (peso de nascimento inferior a 1.500 gramas ou idade gestacional < 32 semanas). O gasto energético foi avaliado com a calorimetria indireta nos dias 7°, 14°, 21°, 28° dias de vida e alta hospitalar. Medidas do comprimento, perímetro cefálico e peso corporal foram avaliadas semanalmente. A terapia nutricional foi calculada durante a internação do recém-nascido e as informações de cada tipo de alimentação foram registradas em um software que calcula a quantidade total de energia e macronutrientes.
ResultadosForam acompanhados 61 recém-nascidos, sendo 43 adequados e 18 pequenos para idade gestacional. O gasto energético de repouso não apresentou diferença estatística entre os grupos e aumentou entre a primeira e quarta semana de vida (adequados: 26,3% e pequenos: 21,8%). O aporte energético nas duas primeiras semanas de vida mostrou-se bem abaixo do requerimento energético mensurado pela calorimetria.
ConclusãoConsiderando os resultados que demonstram um gasto energético alto ao longo das primeiras semanas de vida, fica evidente a necessidade de fornecer ao recém-nascido pré-termo um melhor aporte energético já nas primeiras semanas de vida, para que os neonatos com ou sem restrição intrauterina possam atingir o seu potencial máximo de crescimento e desenvolvimento.
The period between conception and the first two years of life is considered essential for the healthy development of the child, and changes in the physiological mechanisms in this early period of life can increase the risk of chronic noncommunicable diseases in adult life.1–3
The preterm newborn, in addition to organ immaturity and little energy and nutrient reserve, is exposed to a highly unfavorable environment with nutrient limitations4 at birth, which may result in extrauterine growth restriction.
Adequate nutritional support is essential for all preterm infants, especially those born with very low birth weight and intrauterine growth restriction, due to the higher risk for postnatal mortality and morbidity.5 Nutrient supply shortly after birth should be started as early as possible, because of the high prevalence of growth restriction in the period of neonatal intensive care unit (NICU) hospitalization.6–9
Knowledge regarding energy requirements and adequate nutritional substrates favors the best nutritional planning offered to neonates during the most critical postnatal phase, and can prevent extrauterine growth restriction and excess body fat accumulation in preterm newborns.10
The aim of this study was to longitudinally evaluate the resting energy expenditure, growth, and amount of energy and macronutrients offered in a group of appropriate and small for gestational age preterm infants.
MethodsA cohort study was carried out with preterm infants that were appropriate and small for gestational age at birth, admitted to the Neonatal Intensive Care Unit of Instituto Nacional em Saúde da Mulher, da Criança e do Adolescente Fernandes Figueira/Fiocruz.
Preterm newborns with birth weight <1500g or gestational age <32 weeks who were born and admitted to the hospital NICU were eligible for the assessment of resting energy expenditure.
Infants who were breathing spontaneously in ambient air and who had no congenital malformation, infectious diseases, genetic syndromes, or Rh isoimmunization were included. Those with grade III and IV intraventricular hemorrhage (IVH) or necrotizing enterocolitis during the study were excluded.
The newborns participating in the study were evaluated once a week on the 7th, 14th, 21st, and 28th days of life, and immediately prior to hospital discharge.
Resting energy expenditure was measured by indirect calorimetry (Deltatrac II® Metabolic Monitor; Datex-Ohmeda, Finland) using the open-circuit principle, allowing measurement of oxygen consumption and carbon dioxide production using a continuous flow generator. The individual's energy production is calculated from the energetic equivalents of the consumed oxygen and produced carbon dioxide, using the Weir equation.11
For better comfort, to benefit sleep and reduce movement by the newborns, they were placed in the prone position before the examination. This test was performed with newborns in an incubator in the thermoneutral zone, for better temperature monitoring. Heart rate and oxygen saturation were monitored throughout the examination.
All resting energy expenditure assessments were performed at the neonatal unit one hour after feeding. After reaching the steady state, 60minute-by-minute measurements of VO2, VCO2, and energy expenditure were made, and mean values and standard deviations were calculated at the end.12,13
The equipment was calibrated before the start of the study with the alcohol burn test, according to the manufacturer's specifications. Before each examination, the calorimeter was heated for 30min and then calibrated with a known mixture of gases containing 5% carbon dioxide (CO2) and 95% oxygen (O2).
To calculate the energy requirement, an average of 60kcal/kg/day was added to the resting energy expenditure, obtained by indirect calorimetry. This addition is due to the energy requirement for newborn activity, thermoregulation, thermic effect of food, fecal loss, and energy stock, as recommended by the American Academy of Pediatrics.14
Growth was assessed weekly through the measurements of length, head circumference, and body weight. The newborn's weight was measured daily using a scale (Filizola®, SP, Brazil) with an accuracy of 5 grams. Length was measured using a pediatric stadiometer fitted to the incubator, with a precision of 0.1cm, where the child was placed on a flat surface, on the fixed part of the stadiometer with the head in the Frankfurt plane, with extended knees and the feet flexed at a 90° angle, placed on the movable part of the stadiometer. Head circumference was measured using an inextensible metric tape with a precision of 0.1cm, positioned on the most prominent posterior portion of the skull (occiput) and on the frontal part of the head (glabella).
The gestational age at birth was considered according to the first trimester gestational ultrasound (USG), the date of the last menstrual period (LMP), and in the absence of these data, the value calculated by the method of Ballard et al. in 199115 was considered, in this order. The newborns’ disease severity degree was calculated through SNAPPE II (Score for Neonatal Acute Physiology with Perinatal Extension-II), and values greater than 20 were considered to identify more severe newborns.
To classify the nutritional status of newborns at birth, the 2013 Fenton and Kim curve16 was used. For the classification of weight-for-gestational age Z-score, newborns with Z-score <−1.28 standard deviations were considered small for gestational age, and appropriate for gestational age those with Z-score between ≥−1.28 and <1.28 standard deviations (corresponding to the percentiles between 10 and 90).
The nutritional therapy was calculated during the newborn's entire hospital stay using the daily record filled out by the nursing team (document that indicates the diet infused in the newborn daily) and the information of each type of feeding (parenteral, enteral, and oral). This information was recorded in software that calculates the total amount of energy and macronutrients.
The use of human milk in the assessed unit was high and, therefore, the energy and macronutrient composition of the human milk offered at the unit was calculated using the spectrophotometric technique using the infrared analysis technique (Milko-ScanMinor 104®, Foss, Denmark). A 7-mL sample of the human milk offered to the newborn was required for this measurement.
The enteral diet and/or oral formula specific for preterm newborns was calculated based on the information on the product label, following the instructions regarding volume and dilution.
The nutritional supply was calculated by the fluid (mL/kg/day), energy (kcal/kg/day), protein (g/kg/day), lipid (g/kg/day), and carbohydrate (g/kg/day) rates.
Statistical analysisThe data were entered in specific spreadsheets and later analyzed using SPSS software (SPSS Inc. Released 2007. SPSS for Windows, Version 16.0. Chicago, USA).
The evolution of serial measurements of energy expenditure was evaluated from models for non-parametric longitudinal data for repeated measurements, for the difference between medians (Mann–Whitney test) and hierarchical modeling for association analysis.
Descriptive and bivariate analyses were performed to identify previous patterns and associations in the data. The level of significance for the analyses was set at 5%.
This project was approved by the Committee of Ethics in Human Research of Instituto Fernandes Figueira – CAAE: 00754612.9.0000.5269. The informed consent form was signed by the parents/guardians of the newborns eligible for the study.
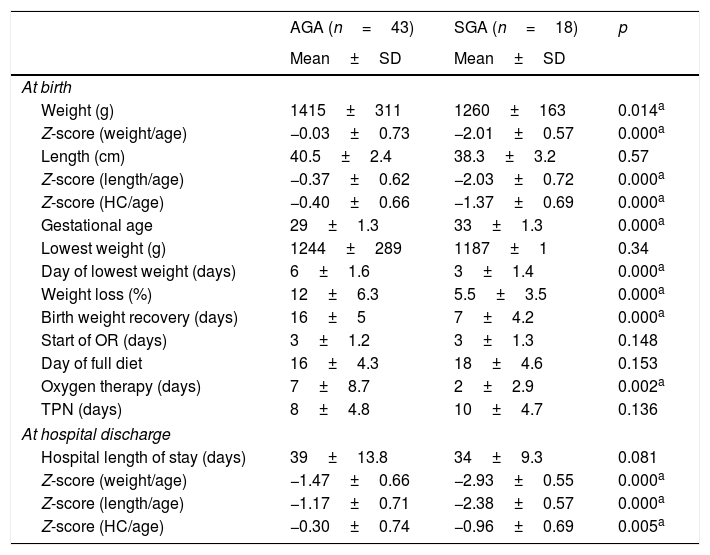
ResultsA total of 61 newborns participated in the study, of which 43 were appropriate (AGA – 18 males and 25 females) and 18 were small for gestational age (SGA – six males and 12 females). SNAPPE score values ≤20 were present in 81.4% of AGA and 77.8% of SGA infants. Regarding the type of delivery, the normal delivery frequency was 37.2% in the AGA and 5.6% in the SGA infants. Neonatal characteristics during hospitalization showed a significant difference between the two groups, which can be seen in Table 1.
Mean and standard deviation of neonatal characteristics during hospitalization.
| AGA (n=43) | SGA (n=18) | p | |
|---|---|---|---|
| Mean±SD | Mean±SD | ||
| At birth | |||
| Weight (g) | 1415±311 | 1260±163 | 0.014a |
| Z-score (weight/age) | −0.03±0.73 | −2.01±0.57 | 0.000a |
| Length (cm) | 40.5±2.4 | 38.3±3.2 | 0.57 |
| Z-score (length/age) | −0.37±0.62 | −2.03±0.72 | 0.000a |
| Z-score (HC/age) | −0.40±0.66 | −1.37±0.69 | 0.000a |
| Gestational age | 29±1.3 | 33±1.3 | 0.000a |
| Lowest weight (g) | 1244±289 | 1187±1 | 0.34 |
| Day of lowest weight (days) | 6±1.6 | 3±1.4 | 0.000a |
| Weight loss (%) | 12±6.3 | 5.5±3.5 | 0.000a |
| Birth weight recovery (days) | 16±5 | 7±4.2 | 0.000a |
| Start of OR (days) | 3±1.2 | 3±1.3 | 0.148 |
| Day of full diet | 16±4.3 | 18±4.6 | 0.153 |
| Oxygen therapy (days) | 7±8.7 | 2±2.9 | 0.002a |
| TPN (days) | 8±4.8 | 10±4.7 | 0.136 |
| At hospital discharge | |||
| Hospital length of stay (days) | 39±13.8 | 34±9.3 | 0.081 |
| Z-score (weight/age) | −1.47±0.66 | −2.93±0.55 | 0.000a |
| Z-score (length/age) | −1.17±0.71 | −2.38±0.57 | 0.000a |
| Z-score (HC/age) | −0.30±0.74 | −0.96±0.69 | 0.005a |
AGA, appropriate for gestational age; SGA, small for gestational age; BW, birth weight; OR, oral route; TPN, total parenteral nutrition; HC, head circumference.
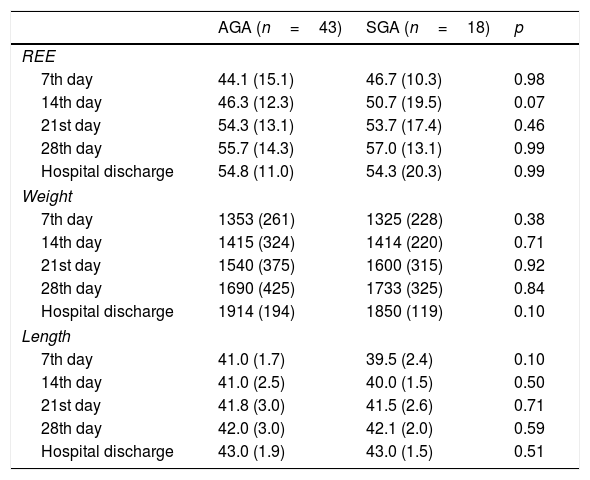
The analysis of the serial measurements of resting energy expenditure, although not disclosing statistical difference between the groups, showed that the values increased gradually each week. Up to the 28th day of life, there was an increase in energy expenditure of 26.3% in the AGA and 21.8% in SGA group (Table 2).
Median and IQR values of resting energy expenditure (kcal/kg/day), weight (grams), and length (cm) at each week of appropriate and small for gestational age preterm infants.
| AGA (n=43) | SGA (n=18) | p | |
|---|---|---|---|
| REE | |||
| 7th day | 44.1 (15.1) | 46.7 (10.3) | 0.98 |
| 14th day | 46.3 (12.3) | 50.7 (19.5) | 0.07 |
| 21st day | 54.3 (13.1) | 53.7 (17.4) | 0.46 |
| 28th day | 55.7 (14.3) | 57.0 (13.1) | 0.99 |
| Hospital discharge | 54.8 (11.0) | 54.3 (20.3) | 0.99 |
| Weight | |||
| 7th day | 1353 (261) | 1325 (228) | 0.38 |
| 14th day | 1415 (324) | 1414 (220) | 0.71 |
| 21st day | 1540 (375) | 1600 (315) | 0.92 |
| 28th day | 1690 (425) | 1733 (325) | 0.84 |
| Hospital discharge | 1914 (194) | 1850 (119) | 0.10 |
| Length | |||
| 7th day | 41.0 (1.7) | 39.5 (2.4) | 0.10 |
| 14th day | 41.0 (2.5) | 40.0 (1.5) | 0.50 |
| 21st day | 41.8 (3.0) | 41.5 (2.6) | 0.71 |
| 28th day | 42.0 (3.0) | 42.1 (2.0) | 0.59 |
| Hospital discharge | 43.0 (1.9) | 43.0 (1.5) | 0.51 |
IQR, interquartile range; REE, resting energy expenditure; cm, centimeters.
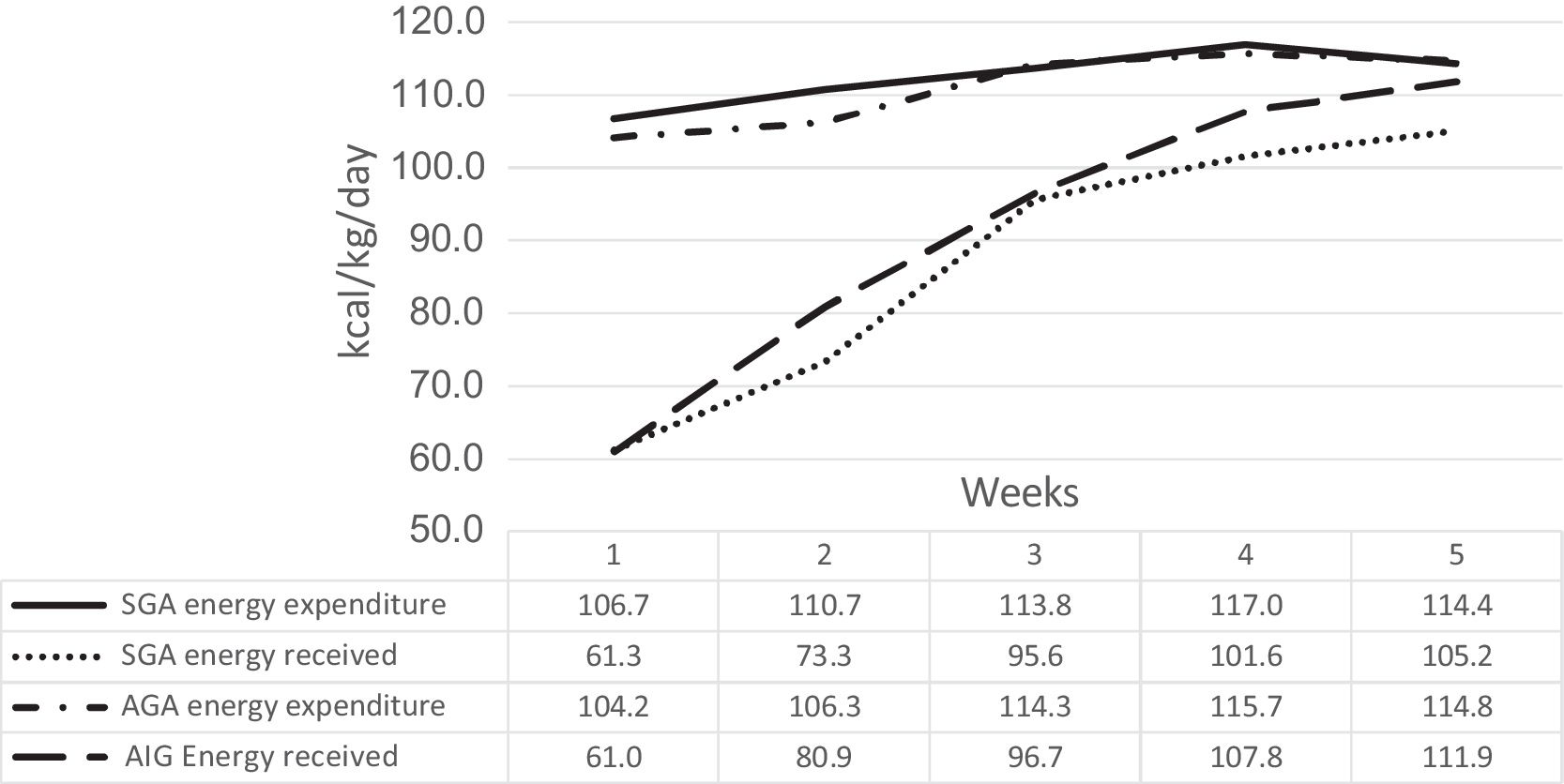
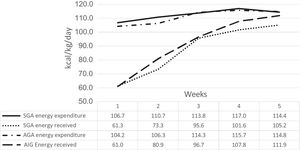
Fig. 1 shows the energy supply received by the two groups during the first weeks of life, demonstrating values below the measured energy requirement. This difference may have contributed to the decline in weight/age and length/age Z-scores over time (Table 1).
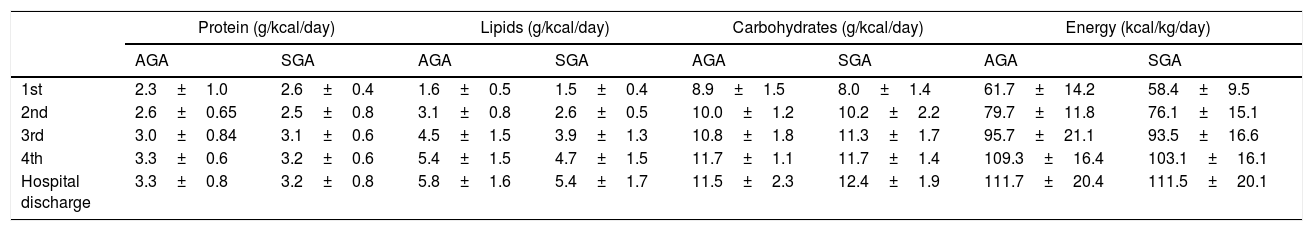
The energy and macronutrient values received by the newborns during hospitalization are shown in Table 3. No significant difference was found between the nutritional therapy received by the AGA and SGA groups.
Mean values of macronutrients and energy received by the two groups during the first four weeks of life and at hospital discharge.
| Protein (g/kcal/day) | Lipids (g/kcal/day) | Carbohydrates (g/kcal/day) | Energy (kcal/kg/day) | |||||
|---|---|---|---|---|---|---|---|---|
| AGA | SGA | AGA | SGA | AGA | SGA | AGA | SGA | |
| 1st | 2.3±1.0 | 2.6±0.4 | 1.6±0.5 | 1.5±0.4 | 8.9±1.5 | 8.0±1.4 | 61.7±14.2 | 58.4±9.5 |
| 2nd | 2.6±0.65 | 2.5±0.8 | 3.1±0.8 | 2.6±0.5 | 10.0±1.2 | 10.2±2.2 | 79.7±11.8 | 76.1±15.1 |
| 3rd | 3.0±0.84 | 3.1±0.6 | 4.5±1.5 | 3.9±1.3 | 10.8±1.8 | 11.3±1.7 | 95.7±21.1 | 93.5±16.6 |
| 4th | 3.3±0.6 | 3.2±0.6 | 5.4±1.5 | 4.7±1.5 | 11.7±1.1 | 11.7±1.4 | 109.3±16.4 | 103.1±16.1 |
| Hospital discharge | 3.3±0.8 | 3.2±0.8 | 5.8±1.6 | 5.4±1.7 | 11.5±2.3 | 12.4±1.9 | 111.7±20.4 | 111.5±20.1 |
AGA, appropriate for gestational age; SGA, small for gestational age.
One of the main goals of neonatal nutritional practices is to provide the preterm infant with an adequate quantity and quality of nutrition that results in an increase in weight indices similar to that of fetuses of the same intrauterine gestational age.17
A technique that may help in the adequate planning of daily energy supply is the knowledge of resting energy expenditure, considering its high contribution, estimated at around 40–50%, to the daily energy requirement.18
The present study analyzed the resting energy expenditure between the two groups of preterm infants and did not find any significant differences. However, from the third week of life in the two groups, the median values of energy expenditure were above the value estimated by the guideline of the American Academy of Pediatrics (2009).14
The values established in the guideline are used to calculate the nutritional therapy offered to the preterm newborn and the knowledge of this percentage above the previous estimate should be considered, so that the energy calculation is not underestimated. Other studies have also demonstrated a progressive increase in energy expenditure and values above those used in the current recommendations,19–21 which corroborates the need to change the nutritional prescriptions in NICUs and the provision of adjusted total energy for this at-risk population.
The group of small for gestational age newborns is poorly evaluated in relation to the energy requirement. Some studies suggest that they have a hypermetabolism when compared to infants without intrauterine growth restriction. In this study, no significant metabolic difference was found in the first weeks of life, which is different from some literature results.10,22,23
Studies that found a difference in the energy expenditure of small and appropriate for gestational age infants also used indirect calorimetry to measure basal metabolism. However, the methods employed were different from those used in this study.
In 1988, Calderay et al.22 assessed eight small (35±2 weeks) and 11 appropriate for gestational age (32±2 weeks) infants; the energy expenditure was assessed when the daily weight gain was above 15g/kg/day. This assessment occurred between the second and third weeks of life and the energy expenditure values were significantly different, 64±8kcal/kg/day in the group of small for gestational age and 57±8kcal/kg/day in the appropriate for gestational age infants.
In 2003, Cai et al.23 evaluated 154 full-term newborns with an average of 5.4±0.7 postnatal days, birth weight between 2500 and 4000g. The energy expenditure values showed a significant difference between children with birth weight >4000g (44.5±5.9kcal/kg/day) and weight between 2500–4000g (48.3±6.1kcal/kg/day). The authors suggest that birth weight has a strong effect on energy expenditure, and that it is lower compared to that of preterm newborns due to the energy demands of high-metabolism organs (such as the brain, liver, heart, and kidneys) and because they have less brown adipose tissue.
In 2011, Bauer et al.10 evaluated 32 preterm newborns at 35 weeks of gestational age and indicated a statistical difference in energy expenditure between small and appropriate for gestational age infants, but without hormonal, lipid profile, and blood pressure alterations. They suggest that energy expenditure is inversely correlated with birth weight.
In this study, the newborns were classified as appropriate and small for gestational age according to weight, length, and head circumference corrected for each gestational age. The anthropometric measurements (weight, length, and head circumference) were analyzed through the Z-score throughout the study period, thus using a gestational age-adjusted measure, unlike the abovementioned studies. Thus, it was possible to study energy expenditure in a more homogeneous population.
As seen in Table 2, the weight and length over the assessed weeks are similar between the two groups, and their corresponding gestational ages (difference of 4 weeks) are what differentiate them.
Other varying factors among the studies are the methodologies used, the gestational age when the energy expenditure evaluation was performed, and the different nutritional practices.
In 2013, Sepúlveda et al.24 also assessed the energy expenditure and body composition of children. However, preterm infants were assessed at around 6 or 7 years of age, and were separated according to the nutritional status at birth, as very low birth weight infants and appropriate for gestational age. These authors verified differences in body size, metabolic parameters, and energy expenditure, suggesting that future assessments are necessary to understand the effects of postnatal growth.
In this study, nutritional therapy was similar in both groups, and it is noteworthy that the energy and protein values recommended for the adequate weight gain in very low birth weight infants, according to Koletzko et al.,25 were achieved only between the 3rd and 4th weeks of life.
The long period of time required to achieve the recommended minimum values of energy and macronutrients becomes a relevant factor for the extrauterine growth, as the nutrient deficit accumulation occurs every day during this low intake period, especially of proteins and total energy.6
Due to the difference between the required energy and energy intake, there is a low weight gain each week, which results in nutritional status impairment, as observed in the weight and length Z-score at hospital discharge in relation to birth measures in both groups. Regarding the head circumference, the Z-score at hospital discharge was higher than at birth in both groups.
Despite the inadequate growth in the first postnatal weeks, reflected by the decline in weight and length Z-scores, adequate evolution of the head circumference Z-score may suggest the hypothesis that the body saves energy for brain development. This growth dynamics in preterm infants can minimize sequelae in the child's neurological development.26
Postnatal growth impairment between birth and hospital discharge remains a major problem in preterm newborns. Feeding practices should follow a more aggressive protocol, with individualized care and a nutritional support team aimed at improving the outcome in these high-risk children.27
More studies are required to follow the infants’ growth after hospital discharge, to assess the effects of the nutritional restriction in this initial period of postnatal life, evaluating body composition in the short and long term, assessing changes in body growth, brain growth through head circumference, as well as the neuropsychomotor development, hormonal changes, and other future changes.
Considering the results that show high energy expenditure during the first weeks of life, the need becomes evident to provide the newborn with better energy intake during these first weeks, so that infants with or without intrauterine restriction can reach their maximum potential for growth and development.
FundingCNPq.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Abranches AD, Soares FV, Villela LD, Méio MD, Zin OA, Junior SC, et al. Energy expenditure, growth, and nutritional therapy in appropriate and small for gestational age preterm infants. J Pediatr (Rio J). 2018;94:652–7.