Most deaths in Pediatric Intensive Care Units involve forgoing life-sustaining treatment. Such deaths required carefully planned end-of-life care built on compassion and focused on palliative care measures. This study aims to assess topics related to the end of life care in Brazilian pediatric intensive care units from the perspective of a multidisciplinary team.
MethodThe authors used a tested questionnaire, utilizing Likert-style and open-ended questions. After ethics committee approval, it was sent by email from September to November/2019 to three Pediatric Intensive Care Units in the South and Southeast of Brazil. One unit was exclusively dedicated to oncology patients; the others were mixed units.
ResultsFrom 144 surveys collected (23% response rate) 136 were analyzed, with 35% physicians, 30% nurses, 21% nurse technicians, and 14% physiotherapists responding. Overall, only 12% reported enough end-of-life care training and 40% reported never having had any, albeit this was not associated with the physician's confidence in forgoing life-sustaining treatment. Furthermore, 60% of physicians and 46% of other professionals were more comfortable with non-escalation than withdrawing therapies, even if this could prolong suffering. All physicians were uncomfortable with palliative extubation; 15% of all professionals have witnessed it. The oncologic team uniquely felt that “resistance from the teams of specialists” was the main barrier to end-of-life care implementation.
ConclusionMost professionals felt unprepared to forego life-sustaining treatment. Even for terminally ill patients, withholding is preferred over the withdrawal of treatment. Socio-cultural barriers and the lack of adequate training may be contributing to insecurity in the care of terminally ill patients, diverging from practices in other countries.
The many advances in Pediatric Critical Care over the last 30 years have allowed a substantial reduction in mortality12 which now ranges between 2.5 to 12%, depending on the part of the world analyzed.34
What becomes even more relevant in the modern Pediatric Intensive Care Units (PICUs) is that most of the remaining deaths are not preceded by a sudden cardiac arrest, but rather are the culmination of a defined end-of-life care (EOLC) plan within palliative care (PC) context.56The decisions leading to this planned ending usually follow an agreement between the healthcare team and the family. These goals of care discussions lead to measures to forgo Life-Sustaining Treatment (LST) that include no-resuscitation and/or no-escalation orders or even withdrawal of technological support, medications, and even hydration, associated with multidisciplinary support for the family to comfort them, including ceremonials and memories creation.7
Recent data from PICUs in Brazil reflect this trend, with less than 50% of deaths being a consequence of failed cardiopulmonary resuscitation.89 The “Conesul End-of-Life Study Group” and the American College of Critical Care Medicine recommend a systematic approach to EOLC focused on the patient and their family at all stages utilizing a PC approach.1011The objective of these procedures is to provide a dignified, compassionate and, above all, humanized death in PICUs, despite the high technological complexity that characterizes them.711
In this scenario, the adequate preparation of multidisciplinary teams to achieve this objective is essential.712 When facing a patient considered terminal, the care team members may be subject to intense emotional suffering, associated with ethical dilemmas and conflicts of a social and/or religious nature with families and teams.12
The present study aims to investigate the perspectives of Brazilian PICU professionals about EOLC, including decision-making, bereavement, and family support, in order to promote a national debate on palliative care practices.
MethodsThis is a cross-sectional study applied in PICUs of three different hospitals from the South and Southeast of Brazil: two mixed PICUs, one with 46 beds and the other with 68 beds, both with cardiac postoperative care, and one at an oncologic hospital with 7 beds. All hospitals offer organ transplant programs and the two general PICUs have ECMO (Extracorporeal Membrane Oxygenation) programs. The oncologic PICU and one of the general PICUs are part of public hospitals, and the other general unit is part of a private hospital. They were chosen for convenience, aiming to capture the perspective of healthcare professionals working in tertiary/quaternary units.
The participation was voluntary, anonymous and without monetary incentive. The study was reviewed and approved by the coordinating entity and its ethics committees (Instituto PENSI - Pesquisa e Ensino em Saúde Infantil; CAAE nº 06681119.7.0000.5567).
The questionnaire was prepared using the Google Forms® platform (Mountain View, CA, USA), with its content validity evaluated and approved by 12 PICU experts, using the methodology described by Burns et al.13 Its final version contains 37 questions (34 multiple-choice and 3 free texts): 6 about training and personal experience; 6 evaluating the team's thoughts about the ideal practice; 3 exploring the professional's comfort level with decision-making; 6 about the existing EOLC model; 4 addressing family communication; 4 evaluating care after support limitation/withdrawal and death; 8 about demographic information (personal and institutional) (Supplemental Content).
The survey was distributed between 09/25/2019 and 12/15/2019, by email. Managers were encouraged to send three monthly reminders. This publication describes a portion of the data obtained, to be complemented by future publications.
For better understanding and respecting the decision-making roles, most of the answers were divided between physicians versus other Health Care Professionals (HCPs) of the multidisciplinary team (nurses, respiratory therapists, and nursing technicians). When relevant, the authors report the responses globally, that is, referring to “all professionals”.
Statistical analysisThe results obtained were tabulated using the Google Sheets® platform (Mountain View, CA, USA). Categorical variables were expressed as percentages or in descriptive form, compared with each other using the chi-square or Fisher's test, according to applicability. Univariate regressions were performed to assess the strength of the association between responses. Statistical analysis was performed using the R language version 3.5.2.14
ResultsThe three hospitals involved in this research have 626 professionals working in PICUs: 156 physicians (25%), 405 nurses and nursing technicians (65%), 40 physiotherapists (6%) and 25 other professionals (4%).
The authors obtained 144 responses (23% response rate). Six questionnaires were excluded from the analysis, due to the low representation of their professional class in the general sample (three social workers, one pharmacist, one nutritionist and one psychologist). Two questionnaires were excluded because they were incomplete, with the final sample consisting of 136 questionnaires.
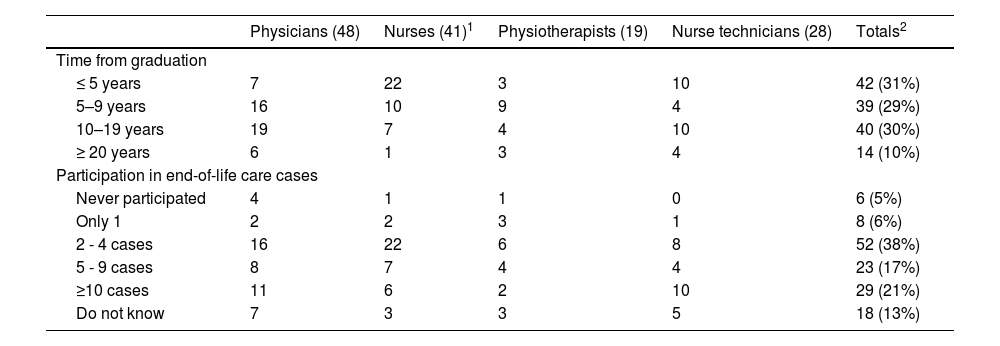
Participants profileTable 1 details the 136 participants included, broken down by profession, time since graduation and their involvement in EOLC cases.
Participants profile and participation on end-of-life care cases.
| Physicians (48) | Nurses (41)1 | Physiotherapists (19) | Nurse technicians (28) | Totals2 | |
|---|---|---|---|---|---|
| Time from graduation | |||||
| ≤ 5 years | 7 | 22 | 3 | 10 | 42 (31%) |
| 5–9 years | 16 | 10 | 9 | 4 | 39 (29%) |
| 10–19 years | 19 | 7 | 4 | 10 | 40 (30%) |
| ≥ 20 years | 6 | 1 | 3 | 4 | 14 (10%) |
| Participation in end-of-life care cases | |||||
| Never participated | 4 | 1 | 1 | 0 | 6 (5%) |
| Only 1 | 2 | 2 | 3 | 1 | 8 (6%) |
| 2 - 4 cases | 16 | 22 | 6 | 8 | 52 (38%) |
| 5 - 9 cases | 8 | 7 | 4 | 4 | 23 (17%) |
| ≥10 cases | 11 | 6 | 2 | 10 | 29 (21%) |
| Do not know | 7 | 3 | 3 | 5 | 18 (13%) |
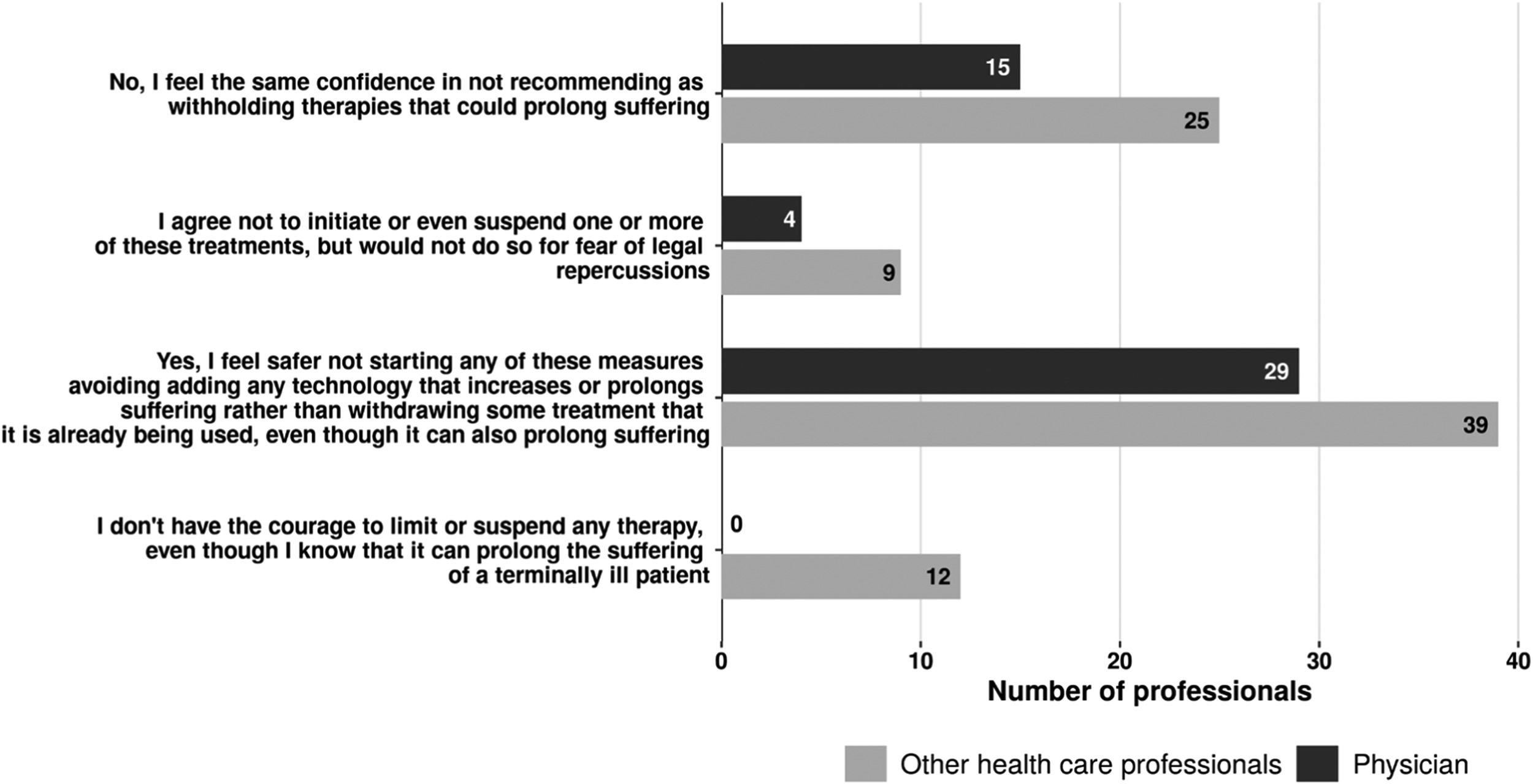
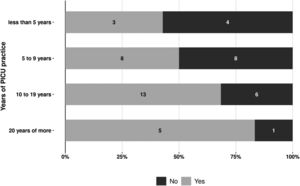
The questionnaire evaluated the professionals' self-reported confidence and comfort in carrying out Goals of Care meetings with the patient's family members. Among physicians, there is a trend to greater confidence in the elaboration of an EOLC plan according to their practice time (Figure 1). When asked about the reason for their insecurity, 18 of the 20 physicians agreed with the statement “I believe these conversations are important, but I don't feel technically prepared for this type of conversation”.
Through univariate regressions compared with other HCPs, physicians were 3.45 times more likely to feel confident in relation to EOLC participation (p < 0.001). Less than 50% of the total group answered that they had some training focused on EOLC, however, considering it insufficient for their practice; 46% (22/48) physicians and 36% (32/89) of the other HCPs reported never having had any training in this area. Only 6% (3/48) of physicians reported that they had sufficient training to conduct EOLC.
Barriers to EOLC implementationIn a multiple-choice question, participants were asked about the main barriers to EOLC implementation, with 133 responses and 3 abstentions. “Cultural/social” difficulties are the biggest obstacle, with “difficulty/resistance of families to approach this subject” as the reason mentioned by 65% (87/133) of the participants.
For 38% (51/133) professionals, the main barrier was “resistance from the teams of specialists involved in the case”. This item was chosen by 73% (16/22) of the professionals from the oncologic PICU, a different pattern from that observed in the other two hospitals; 43% (16/37) and 26% (19/74) respectively (p < 0.001). Religious reasons, both from patients and professionals, were mentioned by 23% of the participants.
The “difficulty in the clinical recognition of the patient's terminality” was reported in less than 14% (19/133) of the answers. “Litigation fear”, “lack of institutional support” or “resistance within the PICU team to EOLC decisions/practices” were mentioned in approximately 20% of the responses each. Specifically considering the physicians' responses, “resistance within the PICU team itself” was identified as a barrier by 36% (17/47) of them, while only 8% (7/86) of other HCPs had this perception (p < 0.001). Likewise, the “litigation fear”, pointed out by 36% (17/47) of the physicians, was one of the reasons mentioned by only 8% (9/86) of the other HCPs (p < 0.001).
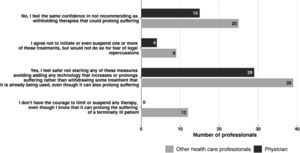
Decisions of withholding and withdrawing LSTParticipants were asked how confident or comfortable they felt about the decisions of withholding and withdrawing LST. Considering the physicians' perception that the resistance of the PICU team itself is an EOLC implementation barrier, a comparison was made between physicians (43 replies) and other HCPs (68 replies) (Figure 2). Among the responses, 67% (29/43) of physicians and 57% (39/68) of other HCPs felt more confident in non-escalating than in the withdrawal of LST, even if it could prolong the patient's suffering (p = 0.68).
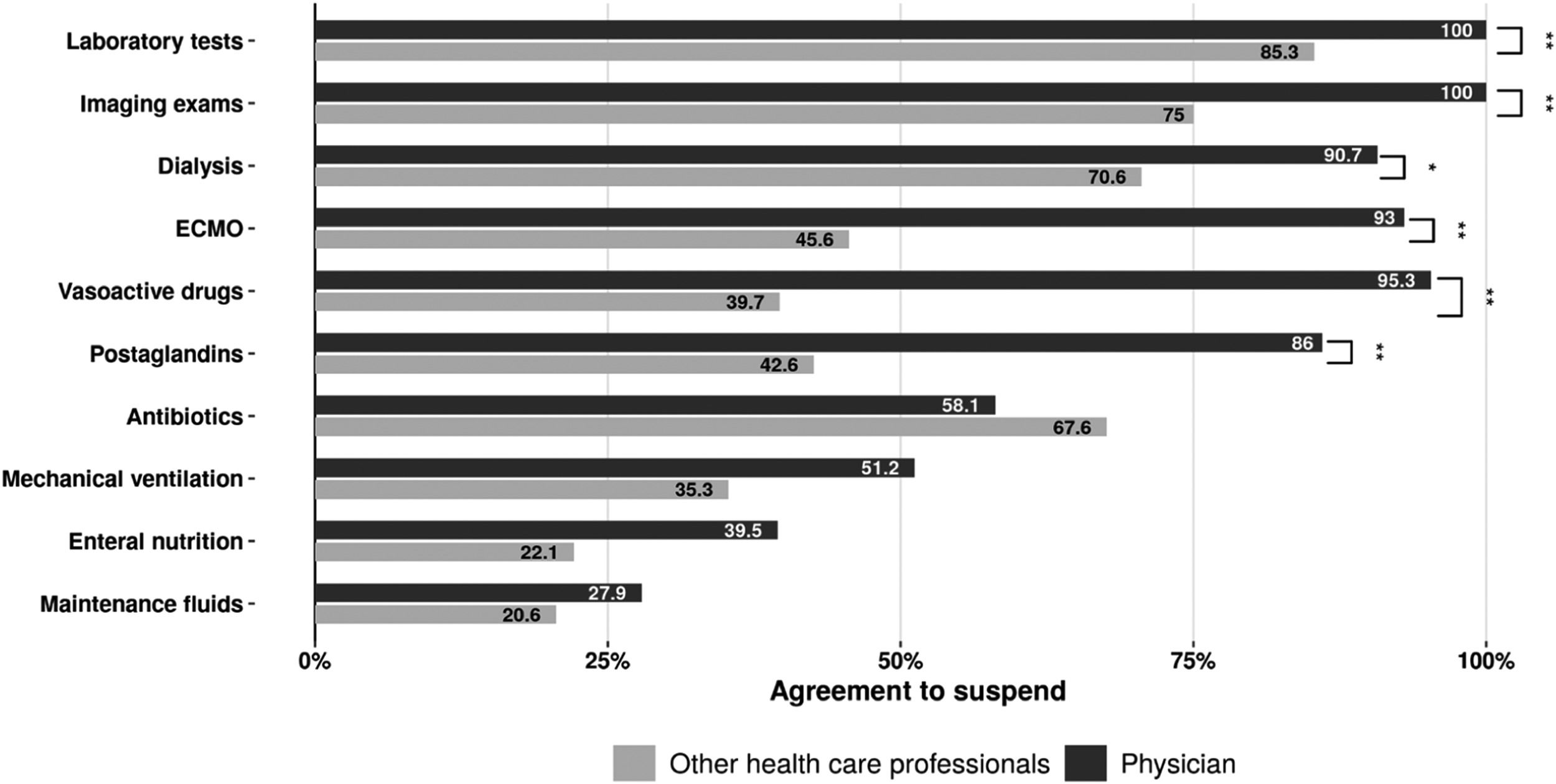
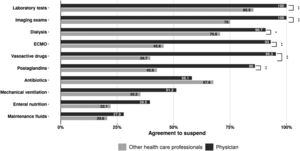
In a multiple choice question, professionals picked the types of therapy they would withdraw (Figure 3). The physicians unanimously would not perform complementary exams, unlike the other HCPs. Similarly, withdrawal of hemodynamic support, whether pharmacological or mechanical (ECMO), was indicated by almost all physicians but less than half of the other HCPs. Regarding mechanical ventilation, there was no statistical difference between the two groups, with half of the physicians agreeing with its withdrawal. Stopping fluids was a very infrequent choice for both groups.
However, when confronted with a fictitious clinical terminality scenario, none of the physicians would remove ventilatory support: 63% (30/43) would rather not escalate ventilatory settings; 25% (12/43) of them would agree with adjusting ventilation upon clinical deterioration, waiting for cardiorespiratory arrest, with the agreement of 41% (36/68) of the other professionals. None of the physicians would agree with palliative extubation, albeit 5% (4/68) of the other HCPs would accept that.
Participants were asked if they had already participated in the decision-making process of withholding or withdrawing LST involving terminally ill children in the PICU; 62% (84/136) reported having already participated. Only 15% (21/136) already witnessed or had knowledge of palliative extubation in their unit.
Creating memories and posturing after deathRegarding the team's support for the family after death, 61% (29/48) of physicians agree or totally agree with sending a letter of condolences, but 54% (48/89) of other HCPs are neutral, do not think it is necessary or disagree with the measure (p = 0.10). As for a postmortem closure meeting with the families to review the child´s PICU stay, 35% (31/89) of the other HCPs see such meetings as not possible. Only 10% (13/136) reported that this had already been done in their PICU. As for a celebration of life or memorial service for the deceased children, 14% (19/136) reported that it is a regular or sporadic practice.
DiscussionThis study describes the results of a survey on practices surrounding EOLC by the multidisciplinary team of three Brazilian PICUs. Most professionals have already witnessed withholding or withdrawal of LST without, however, adequate training in EOLC to feel comfortable with it themselves. Discomfort with withdrawing treatment was evident, with non-escalation being preferred. This was especially evident by the physician's unanimity on not being comfortable with palliative extubation and the rarity of this procedure in their PICUs. Even after the diagnosis of terminality and knowing that this could prolong the patient's suffering, most professionals would maintain or even adjust ventilatory support.
There were some differences between the studied hospital's PICUs regarding EOLC practices. At the private institution, there was support for the limitation of LST, however a greater resistance to removing LST and palliative extubation. At the Oncologic PICU, there was resistance to limitation and no support for the withdrawal of LST, and no palliative care extubation had been witnessed.
Confidence and comfort with EOLC practices by PICU professionals were not statistically correlated to previous experiences or training in PICU in this small sample. Communication skills between the multidisciplinary team, the patient, and the family are considered one of the relevant domains in the provision of EOLC 15 and are recognized as a challenge by health professionals. This training is associated with the acquisition of self-confidence, controlling emotional reactions, and improving teamwork.16 Lautrette et al. in 200717 studied late family “end points” of a proactive communication strategy in EOL family conferences, with a significant reduction of scores with specific training, suggesting the benefit of EOLC training programs. The National Curriculum Guidelines for the Undergraduate Course in Medicine recommended communication skills in its curriculum since 2001, however, teaching facilitated by communication skills simulation is still incipient.18 Few medical schools, residencies, and multidisciplinary programs have specific teaching in this area.1920 This study corroborates these findings and suggests the need to expand pediatric PC training programs for health professionals in Brazil. Goals of care conversations between the PICU team and the family should incorporate details about advanced care planning and preferences of EOLC,21 including documenting choices regarding resuscitation, invasive ventilation and even withdrawal of LST when certain circumstances arise.21 A Brazilian adult ICU study showed that the variability in EOLC is directly associated with differences in the characteristics of physicians, with those who reported training in EOLC and PC showing a greater probability of applying to forgo LST measures and documenting a “do not resuscitate order” in medical records.22
Although there is no ethical or legal difference between withholding or withdrawing therapies,711 most surveyed professionals felt more comfortable not starting or continuing something than suspending it, even knowing that this could prolong suffering. The act of withdrawal of LST holds the perception of taking an attitude that can “accelerate” death, being often misinterpreted as euthanasia, contrary to their professional values.11 When analyzing a fictitious scenario about a terminal patient, this discomfort was evident with the unanimity among physicians not to perform palliative extubation, a method acceptable by 5% of other professionals. And, although all physicians agreed not to perform additional tests in patients undergoing EOLC, 25% of them and 42% of other HCPs agreed with the alternative of adjusting the ventilatory parameters following laboratory exams, waiting for an eventual cardiorespiratory arrest. The fear of palliative extubation being interpreted as euthanasia, an illegal practice in Brazil, may be the underlying explanation for this practice since 36% of physicians reported fear of legal consequences as one of the barriers to implementing EOLC. It is noteworthy that the Brazilian legislation and the CFM (Brazilian Council of Medicine) support the implementation of palliative care (including withholding and withdrawal of LST) on irreversible life-threatening illness and terminally ill patients when the family agrees.23 The main barrier to the implementation of EOLC mentioned by 65% of professionals was the resistance of families to discuss PC. Brazilian studies have already pointed to a culture that considers parents unprepared to participate in the discussion about EOLC, highlighting a paternalistic bias by the team.22 The presumption that the family does not have enough information or education, combined with a lack of training in the PC approach by the team, can aggravate and prolong the family's grief.24 Furthermore, in Latin America, there is a greater tendency to maintain rather than withdraw LST than in other parts of the world.25 This resistance to performing palliative extubation was also described in a Chilean pediatric study.26 In reality, some pediatric Brazilian centers are already practicing palliative extubation,2728 with a significant increase in the percentage of situations of forgoing LST in Brazil over the last 2 decades. These findings signal that education and better knowledge, associated with legislation changes, may challenge the pervasive idea that the resistance to pursuing better EOLC is socio-cultural in nature.29 A recent study on EOLC practices in a Southern Brazilian PICU highlighted the presence of parents at the time of death in most cases,28 a significant change in practice.
In addition to the resistance of the families, the resistance of the other specialists in initiating the discussion about EOLC planning was one of the main barriers highlighted, being one of the particularities noted in the oncology hospital. This difficulty in approaching EOLC for cancer patients is described worldwide, often related to the paradoxical fear of bringing more suffering at the time of diagnosis or during cancer treatment.24 The emotional and clinical investment in the oncological patient and the complexity of the treatment may explain the professional's difficulty in accepting therapeutic exhaustion and terminality.30
This study showed that it was infrequent to contact the family after the death or to carry out any kind of memorial ceremony. Unlike other professionals, the physicians were willing and interested in contacting the families to review the death. Not surprisingly, 60% of bereaved families in one study expressed a desire to meet with their child's intensivist in the weeks after death31 to revisit their child's trajectory, make sure the decisions were correctly made and give feedback to the medical team. These meetings can clarify final events, offer a sense of “closure”, and are an important support for them. They also provide an opportunity for evaluation of possible abnormal grief. The holding of “celebration of life” or memorial services, letters sending by the team, and formal family follow-up by defined periods after the child's death in the PICU are common practices in North American centers but rarely practiced in Brazil.7
Strengths and limitationsThis study has some limitations. It included just three hospitals, with a relatively low response rate, in an economically developed urban area of Brazil, perhaps not reflecting the reality of less privileged areas. In some questions, the interpretation of the statement may have influenced the participant's response. Also, local policies or guidelines about EOLC were not requested formally. As a strength, the survey was multidisciplinary, properly tested and validated, and included PICUs in hospitals with different models of care.
ConclusionThis study reveals that EOLC in Brazil has been carried out with professionals that feel rather unprepared for it. They also expressed their preference for no escalation rather than withdrawal of LST, which was corroborated by the finding that palliative extubation is still rarely performed. After a child's death, there is no culture of celebrating the child's life, follow up, or memory building. These results point to the need to invest in education and research in this area.
The authors thank the PENSI institute for the logistical support and the experts in pediatric critical care (physicians, nurses, nursing technicians and physiotherapists) that had agreed to test the survey and made suggestions for improvements.
Institution to which the work is linked: Instituto PENSI - Fundação José Luiz Egydio Setubal.