Allergic rhinitis (AR) is a disease associated with impaired quality of life and heredity. This study aimed to investigate the association of allergic rhinitis in preschool children with exposure to indoor environment-related factors early in life.
MethodsIn August 2019, the authors implemented a study among 2020 preschool children in Urumqi City using a case-control design. The study included parental reports for the occurrence of AR in children, parental history of respiratory disease, and indoor environmental correlates of maternal exposure from 1 year prior to pregnancy until the child's age of 0-1 year.
ResultsMode of birth (cesarean section) (OR = 1.31, 95% CI = 1.02∼1.67), father with AR (OR = 2.67, 95% CI = 2.08∼3.44), mother with AR (OR = 3.70, 95% CI = 2.88∼4.74), mother with asthma (OR = 3.11, 95% CI = 1.18∼8.20), and mother with newly purchased furniture in the parents' residence during pregnancy (OR = 1.49, 95% CI = 1.03∼2.14) were risk factors for AR in children.
ConclusionsThe focus of allergic rhinitis should be on children with a family history of AR and asthma and cesarean delivery. Primary prevention efforts for AR in preschool children are avoiding exposure of children to indoor environmental hazardous factors early in life.
Allergic rhinitis (AR) refers to a noninfectious inflammatory disease of the nasal mucosa involving multiple immunocompetent cells and cytokines mediated by IgE after allergen exposure in atopic individuals.1 Most people ignore the harms posed by AR because of its milder symptoms, but several studies have confirmed that AR causes a range of serious harms. An important study from the Chinese lung health study group published in The Lancet in 20192 showed that AR is an important risk factor for asthma in adults. In addition, symptoms of AR adversely affect patients' work and quality of life, and in severe cases, sleep-disordered breathing can occur.3 AR also causes symptoms such as reduced learning ability and poor concentration in children and adolescents.4 A 2012 study from 10 cities in China involving an indoor environment and child health (CCHH) showed a prevalence of physician-diagnosed AR ranging from 2.2% to 23.9% in Chinese preschool children, including 9.8% in Urumqi City.5 Since Urumqi City is a multiethnic aggregation site, there are large differences in lifestyle habits among ethnic groups, and the climate is dry, which may affect the transmission of allergens within the environment. It is, therefore, necessary to carry out a large epidemiological survey study of AR in preschool children as soon as possible. A 2019 study suggested that exposure to environmental risk factors early in life may increase the incidence of AR in children.6
For the reasons set out above, the prevalence of AR among preschool-aged children and mothers’ residential environmental factors from preconception to the age of 1 year in 60 kindergartens in Xinshi District, Shayibake District, Tianshan District, Shuimogou District, Toutunhe District, and Midong District were investigated in August 2019. Exploring the association between exposure to indoor environment-related factors and AR in children during this period provides a scientific and theoretical basis for the prevention of AR in children.
MethodsInvestigated subjectsIn August 2019, the authors used stratified random sampling, six administrative districts were first selected in the Urumqi, which were Xinshi District, Shayibake District, Tianshan District, Shuimogou District, Toutunhe District, and Midong District. Then 8-12 kindergartens were randomly selected in each district. A total of 60 kindergartens were selected, and children with AR who diagnosed by doctors were investigated. In the same period, children who were sex -, age -, and ethnicity matched and had not been diagnosed with AR in the same kindergartens were selected as controls in a 1:4 ratio of the case: control. Every control child was included in this study with equal probability. This study was approved by the ethics committee of the Hospital, and the parents of the investigated children provided written informed consent.
Investigation contents and methodsQuestionnaires were developed for all children in the case group and control group; the questionnaire contents were adapted from the questionnaires used in the CCHH survey study and were slightly revised according to the specific context of Urumqi City.
The specific survey included:
- (1)
Demographic characteristics, including sex, ethnicity, and age at the home address.
- (2)
Feeding status, including whether they were only children, whether they were breastfed, and duration of breastfeeding.
- (3)
Prevalence of AR in children and family members, including AR in children and parents and AR-related symptoms.
- (4)
Dwelling environment, including housing type, renovation situation, and furniture purchase situation.
- (5)
Living habits, including indoor pets and house plants, smoking, air conditioning, and the use of a new air filtering system.
- (6)
Dietary habits, including meal types and times.
Before the survey began, the subject group first had contact with the Education Bureau of Urumqi City and the kindergarten teachers, and uniform professional training was provided to the responsible teachers involved in the survey class before the survey. Consent for the questionnaire to be administered to the parents of the children was given in their kindergartens by the preschool teachers, and the questionnaires were completed by the parents or other guardians of the children at home. They were asked to complete the form within 1 week and submit it to the responsible teacher at the kindergarten, who then returned the questionnaire and uniformly sent it to the Education Bureau of Urumqi City. All questionnaires were reviewed by more than 2 trained subject team members, and ineligible questionnaires were excluded.
Determination of outcomes- (1)
AR: parent reports that the child has had at least 1 occasion in which AR has been definitively diagnosed by a physician, with the age of onset determined by the time of the first diagnosis of AR. Children who visited the hospital because of some symptoms such as frequent sneezing, rhinorrhea, nasal blockage, and nasal itching, then were diagnosed definitively with AR by the doctor.
- (2)
Passive smoking: refers to the exposure of a non-smoker to the smoke emitted from the ignition cigarette or to the smoke exhaled by the smoker for at least 1 day per week.7
Epi Data 3.1 was used to establish the database, and SPSS 26.0 software was used for data analysis and processing. Univariate analysis used the χ2 test. Factors associated with the onset of AR in preschool children were analyzed using multivariate logistic regression, reporting odds ratios (OR), and 95% confidence intervals (CI). All statistical analyses were performed using α = 0.05 two-sided test criterion, and P < 0.05 was considered statistically significant.
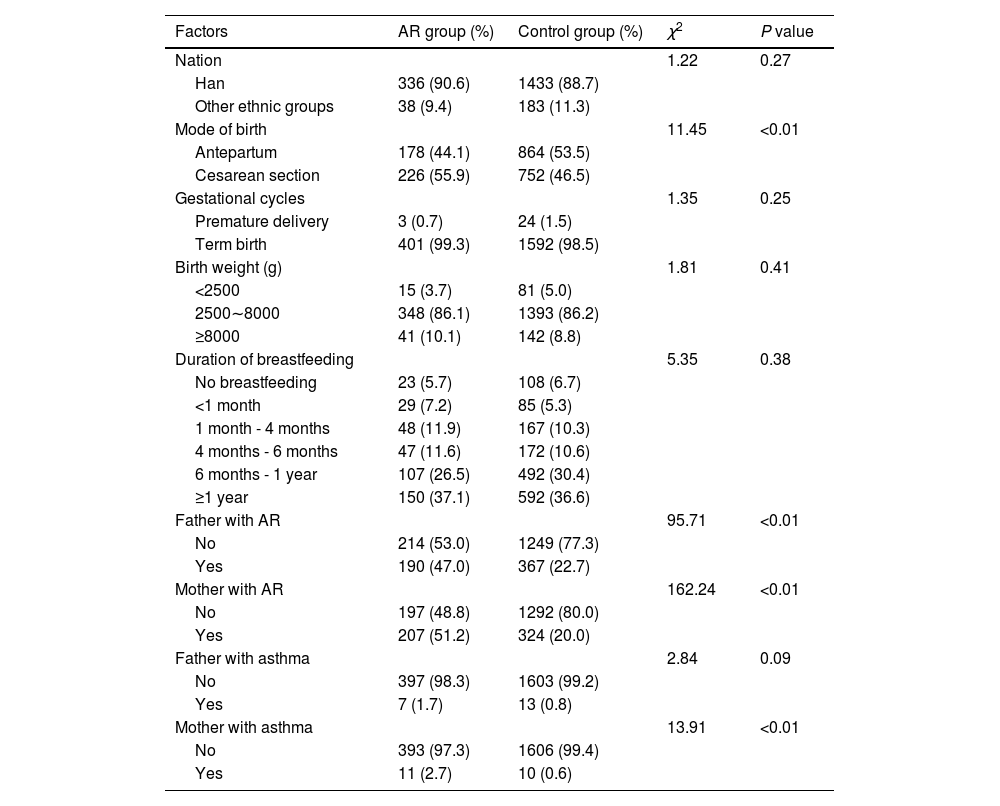
ResultsGeneral condition of the investigated subjectsA total of 404 cases were collected in this study, including 225 boys and 179 girls with a mean age of 5.18 ± 0.99 years and a mean age at onset of 3.29 ± 1.11 years. A total of 1616 individuals were matched in the control group in a 1:4 ratio of cases to controls. The control group used both age and sex as matching specifications. There were 900 boys and 716 girls with a mean age 5.13 ± 1.02 years in the control group. The distribution of mode of birth, father with AR, mother with AR, and mother with asthma showed significant differences between the two groups (all P < 0.05). There were no significant differences in the distribution of ethnicity, gestational cycle, birth weight, or duration of breastfeeding between the two groups (all P > 0.05) (Table 1).
Demographics and characteristics of the AR and controls groups.
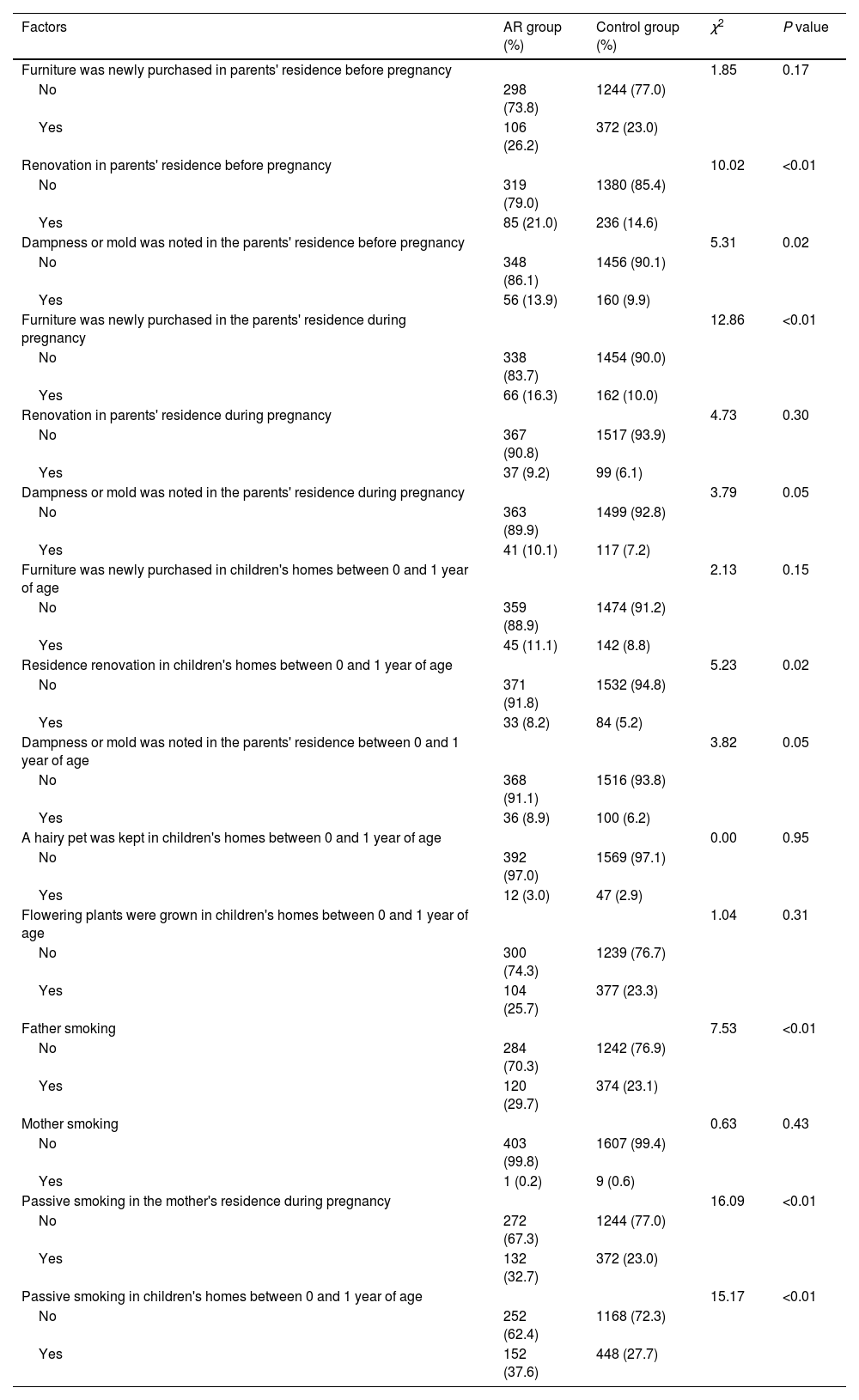
The results of the univariate analysis suggested that renovation or appearance of dampness or mold in the parents' residence before the mother's pregnancy, newly purchased furniture or passive smoking in the parents' residence during the mother's pregnancy, renovation or passive smoking in the children's residence during the child's 0-1 years of age, and father smoking were the main environmental factors contributing to the development of AR in children (all P < 0.05) (Table 2).
Univariate analysis of AR and indoor environmental factors in preschool children between AR and control groups.
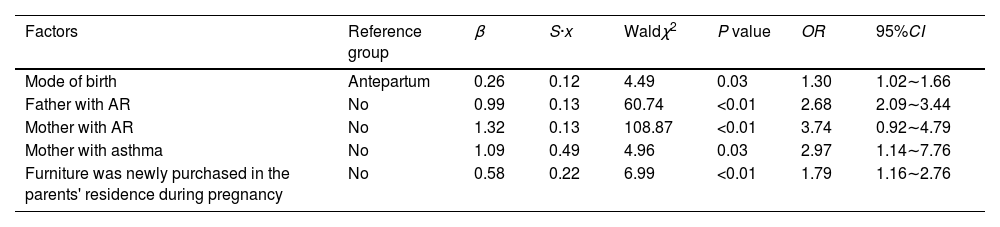
General condition survey analysis was introduced into the logistic regression model along with variables that were meaningful in the results of univariate analysis; suffering from AR was the dependent variable (0 = no, 1 = yes). Five variables of the final residency main effect model were associated with the onset of AR in preschool children. Mode of birth (cesarean section), father with AR, mother with AR, mother with asthma, and newly purchased furniture in the parents' residence during pregnancy were risk factors for childhood AR (all P < 0.05) (Table 3).
Multivariate logistic regression analysis of the onset of AR in preschool children between AR and control groups.
Previous investigators have suggested that the prevalence of AR is influenced by both genetic8 and environmental9 factors. This study found that the parental origin of AR contributed significantly to the pathogenesis of AR in children. Concomitant with the ongoing development of genome-wide association studies (GWAS), multiple genes implicated in the pathogenesis of AR have been identified thus far. Within the past 10 years alone, there have been more than 20 investigative studies on genetic susceptibility genes for AR.8 A 2018 study by Waage et al.10 also identified 41 risk loci for AR, which also suggested that AR has high genetic susceptibility. In addition to AR in parents, this investigation identified maternal asthma as a risk factor for AR in children, the mechanism of which is not fully defined. However, this conclusion was similarly reached in a 2007-2008 survey by Wu et al.11
Asthma and AR are both more common allergic diseases with similar aetiologies, often coexisting in the same family or patient.12 In fact, AR as a significant risk factor for asthma in adults2 has been previously reported. As early as 2008, a study from Western Europe13 was published in The Lancet proposing that either allergic or nonallergic rhinitis could predict the onset of asthma in adults. Regarding how maternal asthma contributes to the onset of AR in children, the authors speculate that on the one hand, there may be an overlap with susceptibility genes. In 2007, the first GWAS on asthma in Nature identified a locus (ORMDL3, GSDML, ZPBP2, and IKZF3) on chromosome 17q21 that confers an increased risk of childhood asthma.14 A subsequent study from Japan15 also confirmed that variants in this locus were involved in the pathogenesis of AR. On the other hand, AR shares the same environmental influences as asthma. A study by Zhao and colleagues16 found that passive smoking and petkeeping could increase the risk of AR and asthma in children. In addition, there are many genes associated with asthma and AR pathogenesis and environmental influencing factors that may be responsible for the increased risk of developing AR in children with maternal asthma.
The present investigation found that cesarean section is a risk factor for AR in children. Previous studies have also suggested that children born by caesarean section have a higher risk of respiratory and allergic diseases than those born vaginally.17,18 In particular, elective cesarean section is more likely to cause respiratory morbidity in children.19 Many studies have confirmed that cesarean section has an important effect on the development and maturation of the neonatal immune system. This may be because children delivered via the birth canal can be exposed to normal beneficial gut microbes from the maternal vagina during delivery. Caesarean-section children are not exposed to these microorganisms, which leads to an imbalance of intestinal flora and the occurrence of diseases such as allergies and autoimmunity.20,21 The study by Azad et al.22 also confirmed that infants born by cesarean section had significantly lower richness and diversity of gut flora than those born vaginally, which may be one of the reasons why children born by cesarean section are more susceptible to AR.
For indoor environmental factors, this study only found an association between newly purchased furniture in the parents' residence during the mother's pregnancy and the onset of AR in children. Newly produced furniture, renovation materials, etc., contain large amounts of volatile organic compounds, of which formaldehyde, benzene, toluene, and xylene are the most common substances.23 Inhalation of such substances at high concentrations irritates the respiratory tract, inducing respiratory disease in children, and formaldehyde is the most representative of these. Many current studies24 have confirmed that formaldehyde can cause respiratory injury. In addition, substances such as formaldehyde can also cross the placental barrier and act on the embryo, causing abnormal fetal growth and development.
Several studies have previously confirmed that indoor passive smoking,16 parental smoking,25-27 keeping houseplants,28 petkeeping,16 and indoor dampness phenomena29 are closely related to the development of respiratory diseases in children, although this study did not draw the above conclusions. This may be because this study employed a case-control design, and for the case group, subjects were selected strictly according to the physician-diagnosed AR. Some children who presented with AR symptoms but were not definitively diagnosed with AR were not included in the case group. This may have been overly conservative, resulting in the above factors not being found to be associated with AR pathogenesis in children. Additionally, it has been suggested that outdoor air pollution may negatively affect respiratory health but may also enhance sensitization to some plants and fungi.30 In 2012, a "coal to gas" project was launched in Urumqi City, Xinjiang, which greatly improved the outdoor air quality and may have impacted some factors in the analysis. Therefore, based on the results of the present investigation, it is not yet possible to demonstrate, that the abovementioned factors are not associated with the onset of AR in children. Further confirmation through population-based cohort studies is required to further clarify the contributing factors to the onset of AR in children.
ConclusionCesarean section, parents with AR, mother with asthma, and buying new furniture in the mother's home during pregnancy are risk factors for AR in preschool children. The authors should actively carry out AR prevention for cesarean section preschool children with a family history of AR and asthma, and prevent children from contacting harmful factors in the indoor environment early in life.
Data availabilityThe datasets generated and/or analyzed during the current study are not publicly available due to the data belonging to the School of Public Health of Fudan University but are available from the corresponding author upon reasonable request.
Ethics approval and consent to participateThe study was conducted strictly in accordance with the Declaration of Helsinki and approved by the research ethics committee of Fudan University (protocol no. IRB00002408 & FWA00002399), all parents and class teachers of the children under investigation have signed written informed consent.
FundingThis study was supported by the National Natural Science Foundation of China (grant no. 81861138005, 81860179); Teacher's professional development project of the Shanghai Municipal Education Commission and High-Level Local University Construction Projects of Shanghai University of Medicine & Health Sciences.