Congenital diaphragmatic hernia (CDH) remains one of the most dreaded congenital anomalies in the neonatal intensive care units (NICUs). Herniation of the abdominal organs through a malformed and defective diaphragm during fetal development can lead to near-lethal pulmonary hypoplasia and cardiac deformation. Severe persistent pulmonary hypertension of the newborn (PPHN), hypoxic respiratory failure, and cardiac dysfunction often complicate the medical course of newborns with CDH. Recognizing the interdependence of the pulmonary and cardiovascular systems, especially in the context of abnormal physiology, is of paramount importance when providing medical management to these patients.
The incidence of CDH is estimated at approximately one case per 3,000 live births. A reliable estimation, however, is complicated by termination of pregnancy, inaccurate data collection, and unreported cases of newborns who die of the disease without a known prenatal diagnosis (referred to as “hidden mortality”).1 The condition is uncommon enough so that the majority of regional NICUs manage less than a dozen cases of CDH annually, which also explains the ongoing challenges in conducting prospective randomized studies. In 1995, the CDH Study Group (CDHSG) registry was established with the purpose to unite tertiary referral centers across four continents to compile data on live born infants with CDH, and to assess therapies and outcomes.2 Short of randomized controlled trials, registries such as the CDHSG and observational studies such as the study by Carmo et al.3 in this issue of Jornal de Pediatria provide an important source of knowledge.
There were 129 newborns with a prenatal diagnosis of CDH delivered at a large NICU in Rio de Janeiro, Brazil during the years 2005–2015. The reported newborn characteristics (i.e., gestational age at birth, sex, side of the CDH, liver herniation, associated incidence of congenital anomalies, etc.) are similar to other published reports on CDH. The overall mortality of 61%, however, is significantly higher compared to the estimated mortality of approximately 20–30% reported from large registries that include centers where extracorporeal membrane oxygenation (ECMO) is available.2–6 This large discrepancy in mortality can partly be explained by the lack of ECMO. Given that 30.3% of CDH patients reported to the registry between 2007 and 2013 were placed on ECMO4 and nearly 51% of CDH undergoing ECMO do not survive,7 only half of the deaths reported by Carmo et al.3 can probably explained by lack of ECMO. Gaining a better understanding on why mortality would be so much higher in a large tertiary NICU with other resources is crucial to identify areas of inadequacy that can be addressed to improve outcomes. As is the nature with observational studies, the present work suffers from limitations that make interpretation of the prognostic indicators incomplete. No information is provided regarding fetal lung volume assessment, echocardiographic assessment of cardiac function, or defect size, factors that have all shown to strongly correlate with survival (Fig. 1).
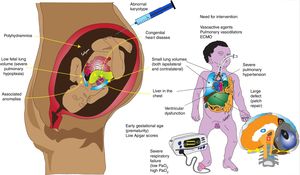
Factors associated with poor prognosis in congenital diaphragmatic hernia (CDH).
Antenatal factors such as low fetal lung volume, associated anomalies (especially cardiac), polyhydramnios, abnormal karyotype, and liver in the chest can be associated with lower survival. Postnatal factors associated with severe pulmonary hypertension (low PaO2), lung hypoplasia (high PaCO2), large defect requiring patch repair, ventricular dysfunction, and need for vasoactive agents and/or ECMO are associated with higher mortality.
Copyright Satyan Lakshminrusimha.
The relationship between diaphragmatic defect size and survival was first reported following the analysis of 3,062 cases of CDH from data gathered by the CDHSG registry spanning nine years from 1995 to 2004, and the size of the defect has been found to have the most important impact on survival.8 Thereafter, a classification system including defect size (graded “A” for small to “D” as agenesis of the diaphragm – Fig. 1)9 and presence or absence of associated major cardiac anomalies has been included in the data analysis. Later reports have shown that babies with a size “A” defect and no major cardiac anomalies have a survival of 99%, compared to 39% survival in patients who have a size “D” defect with a major congenital heart defect.10 The most recent analysis from the CDHSG registry – including 7,617 cases since the inception of the registry in 1995 until 2013 – has reported a marginal increase in overall survival from 67.6% in 1995–2000 to 71.6% in 2007–2013.4 However, patients who required a patch repair saw a greater increase in survival, from 68.1% to 76.9%.4 In spite of a possible higher incidence of larger defects over the past couple of decades, as indicated by the greater need for patch repair, the improved survival in these patients shows a promising trend. It should be kept in mind, however, that most centers in this registry have access to ECMO, which may increase the chances of survival.11
Prenatal diagnosis of CDH, better imaging modalities (magnetic resonance imaging [MRI] vs. ultrasound), and the use of fetal echocardiography can provide information that may help determine success of survival and need for ECMO. Data from the Canadian Pediatric Surgery Network including 140 infants with antenatally diagnosed CDH (75 inborn and 65 outborn) reported that the likelihood of mortality was significantly higher for outborn deliveries (odds ratio 2.8) when adjusting for severity of illness.6 In the aforementioned study, mortality between inborn and outborn infants did not reach statistical significance at 17/75 (20%) compared to 21/65 (38%), respectively (p = 0.25). However, inborn patients had a significantly higher illness severity score. In a more recent analysis from data of the Diaphragmatic Hernia Research and Exploration, Advancing Molecular Science (DHREAMS) study including 220 cases of CDH, patients that were transferred (i.e., outborn) to one of the seven referring centers had higher survival, at 85% (68/80) compared to 71.4% (100/140) for inborn patients.5 No definitive conclusions can be drawn in respect to these studies regarding survival rate and location of delivery, but the data support that outborn newborns with a diagnosis of CDH who survive transfer to a referral center may have less severe disease.
If a prenatal diagnosis of CDH is confirmed, careful fetal evaluation by ultrasound, MRI, and fetal echocardiography can identify several prognostic predictors of newborn outcomes, which include herniation of the liver into the thoracic cavity, assessment of lung volume (e.g., lung-to-head ratio [LHR], percent predicted lung volume [PPLV], and total lung volume [TLV]), evidence of left ventricular (LV) hypoplasia, and any associated congenital anomalies.12 In a recent meta-analysis, confirmation of liver herniation (407 fetuses) compared to no visualization of the liver in the thoracic cavity (303 fetuses) was associated with significantly lower survival (45.4% vs. 73.9%, respectively).13 Furthermore, need for ECMO has been found to be significantly higher in cases of CDH with liver herniation.14 MRI has shown to have superior predictive value compared to ultrasound in assessing lung volume.15 PPLV < 15% and TLV < 20 mL have been shown to be strong predictors of poor outcome and higher ECMO use,16 as would be expected, since lower lung volumes imply severe hypoplasia. Estimation of fetal lung volume can, therefore, improve survival of the most severely affected infants if maternal transfer prior to delivery to a center with ECMO capability can be arranged.
Observations made on post-mortem anatomy studies over three decades ago in infants who died of CDH revealed hypoplastic left hearts and decreased cardiac mass.17 In addition, fetal echocardiography studies in fetuses with CDH showing evidence of LV hypoplasia before 24 weeks gestation have reported 100% mortality after birth.18 Recently, early assessment of cardiac function by echocardiography in infants with CDH has shown that decreased cardiac function is a better predictor for the need for ECMO than severity of pulmonary hypertension.19
The timing and preferred mode of delivery in CDH pregnancies continues to be controversial. Stevens et al. initially suggested that early term delivery may confer an advantage in CDH.20 However, Hutcheon et al. showed that infant mortality significantly decreased with advancing gestation, from 36% at 37 weeks of gestation to 20% at 40 weeks of gestation.21 In addition, a study by Odibo et al. of 107 CDH cases found that gestational age at delivery was inversely correlated to the need for ECMO.22 In contrast, Safavi et al. found no difference in mortality when dividing gestational age at delivery categorically as under 37 weeks, 37–38 weeks, and beyond 39 weeks.23 There was no difference in mortality between vaginal and cesarean delivery. In the absence of strong evidence, it seems reasonable to schedule delivery at 39 weeks or beyond and in a setting with access to tertiary NICU services.
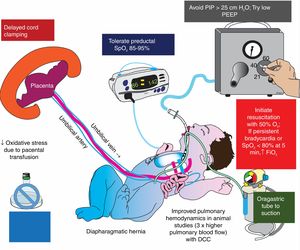
Delayed cord clamping is being investigated in a pilot trial for infants born with CDH (NCT03314233). Studies in lambs suggest that physiological/delayed cord clamping reduces pulmonary vascular resistance (PVR) and significantly increases pulmonary blood flow in CDH.24 A strategy combining ventilation using lower levels of inspired oxygen with lower ventilator pressures25,26 and with an intact cord might be an effective approach during the delivery room resuscitation of CDH (Fig. 2).
Delivery room management in congenital diaphragmatic hernia (CDH).
Oxidative stress plays an important role in the pathogenesis of pulmonary hypertension and injury to hypoplastic lungs in CDH. Delayed cord clamping, limiting barotrauma (with low ventilator pressures), and restricting FiO2 to target preductal SpO2 in the mid-80 s to low 90 s are important strategies to limit oxidative stress in CDH.
DCC, delayed cord clamping; PEEP, positive end-expiratory pressure.
Copyright Satyan Lakshminrusimha.
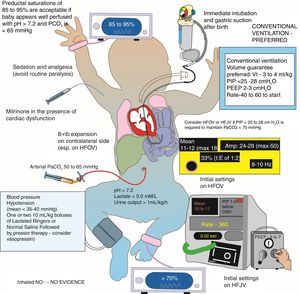
CDH is a complex and unforgiving syndrome, whereby an incomplete understanding of the pathophysiology underlying the hypoxic respiratory failure – as well as the associated PPHN and cardiac dysfunction – can risk an abrupt deterioration of the patient if medical management is not optimized. The hypoplastic lungs are particularly sensitive to ventilator-induced lung injury. Gentle ventilation using low tidal volumes (3–4 mL/kg), low mean airway pressures, and low positive end-expiratory pressure (thereby accepting permissive hypercapnia with CO2 values between 50–65 mm Hg) have shown to improve outcomes and should be considered before high-frequency ventilation.27 Ensuring adequate preductal oxyhemoglobin saturation (SpO2) targets (85–95%) and preventing extremes of hypoxemia (SpO2 < 80%; shown to increase pulmonary vascular resistance) or hyperoxia (SpO2 >95%; known to produce excess reactive oxygen species and cause biotrauma) will optimize oxygenation (Fig. 3).28
Postnatal management of congenital diaphragmatic hernia (CDH) in the neonatal intensive care unit (NICU).
Tolerating preductal oxygenation saturations in 85–95% range, preference of conventional ventilation with a low PEEP, and permissive hypercapnia using strategies of gentle ventilation are important elements of NICU management of CDH.
HFJV, high frequency jet ventilation; CMV, conventional mechanical ventilation; HFOV, high frequency oscillatory ventilation; PEEP, positive end-expiratory pressure; PIP, positive inspiratory pressure.
Copyright Satyan Lakshminrusimha.
Despite clinicians’ best efforts to adopt lung protective strategies and readily available access to selective pulmonary vasodilators (e.g., inhaled nitric oxide [iNO]), the overall number of infants who are placed on ECMO has not changed over the past decade. CDH remains the most common indication to start ECMO, and only approximately half of patients survive to discharge.7 The reason there has been no decrease in the number of CDH ECMO cases and no improvement in survival following ECMO in this population could be because contemporary CDH patients rescued onto ECMO are more critically ill as a result of better medical management compared to their predecessors a few years ago.
Emerging evidence suggests that cardiac dysfunction (especially decreased LV function) may be at the root of impending irreversible cardiopulmonary failure, more so than the severity of PPHN.19,29,30 Poor LV function would be expected to lead to increased left atrial pressure with resultant pulmonary venous congestion and increased pulmonary venous pressure. Decreasing pulmonary arterial pressure in the setting of poor LV function can lead to pulmonary edema and further exacerbate respiratory status. Supporting cardiac function, therefore, may be as critical as managing PPHN in infants with CDH. The role of milrinone (a pulmonary vasodilator also known to have cardiac inotropic and lusitropic effects) is currently being evaluated in a randomized trial in participating centers of the neonatal research network.31 A concomitant European multicenter randomized controlled trial is investigating intravenous sildenafil and iNO incorporating cardiac function assessment (CoDiNOS trial – EudraCT number 2017-000421-13).
Creating algorithms that address the cardiac pathophysiology associated with CDH is likely to lead to substantial improvements in the care of these patients. The aforementioned clinical trials investigating the role of cardiotropic and pulmonary vasodilator drugs may help resolve this hypothesis and improve survival. An evidence-based and systematic approach to CDH management in the delivery room (Fig. 2) and NICU (Fig. 3) has the potential to reduce mortality.
FundingThe work has been supported by NIH grants HD096299 (PV) and HD072929 (SL).
Conflicts of interestThe authors declare no conflicts of interest.