To describe the neurocognitive profile of 458 children with congenital hypothyroidism detected by neonatal screening, followed under the same treatment protocol over 25 years. To correlate estimated full-scale IQ (FSIQ) scores with age at the start of treatment, disease severity, and maternal education.
MethodsObservational, analytical, retrospective, and longitudinal cohort study, that evaluated children detected between 1991 and 2014, who underwent at least one psychometric assessment (WPPSI- R and/or WISC-III). Estimated FSIQ scores are described and correlated with prognosis determinants.
ResultsMedian T4 at diagnosis was 2.8 μg/dL (0.0–16.5), the median age at the start of treatment was 18.5 days (3–309). Maternal education (n = 445): 2.7% of illiteracy, 59.8% with basic education. Estimated FSIQ scores were 88.0 (±11.8) in WPPSI-R (age 5.6 ± 0.5 years) and 84.1 (±13.0) in WISC-III (age 9.1 ± 1.4 years). The intellectual deficit was identified in 11.6%. Correlation between age at the start of treatment and estimated FSIQ was found only in the WPPSI-R test (p = 0.02). Initial T4 and maternal education significantly correlated with estimated FSIQ scores in both tests, with the latter being the most important determining factor.
ConclusionsIn this large cohort of mainly low socioeconomic status children, most children achieved normal cognitive levels; however, a significant percentage presented with below-average estimated FSIQ scores and intellectual deficits. Maternal education was the main determining factor in cognitive level followed by hypothyroidism severity.
Early and adequate levothyroxine (l-T4) replacement provides normal growth, puberty, neurodevelopment, and schooling in the vast majority of children with congenital hypothyroidism (CH) detected by neonatal screening (NS).1-5 Although most patients achieve normal intelligence quotient (IQ), subtle cognitive and motor deficits may occur, suggesting that maternal thyroid hormones may not be sufficient to ensure normal fetal brain development, especially in cases of severe hypothyroidism.6,7 Thyroxine (T4dx) or free thyroxine (fT4dx) levels at diagnosis, age at the start of treatment, l-T4 dose, and adherence to treatment significantly correlate to neurodevelopmental outcomes,8 although other factors are influential, such as familial educational level and socioeconomic status (SES).9,10
A child's performance on an IQ test is greatly improved via effective education but can also be negatively affected by environmental and economic circumstances.11,12 Although IQ scores of CH patients have been published worldwide, most studies derive from first-world countries and developed environments.
Brazil has great socioeconomic and Human Development Index disparity among its states and even within each state.13 Data concerning low-middle income CH patients, specifically from the Brazilian population, are scarce and limited mostly by their small samples, but emphasize the importance of socioeconomic aspects on cognitive achievements.14,15 Therefore, the aims of this study were to describe the cognitive level of children with CH, mostly from a lower socioeconomic population,16 strictly followed under the same treatment protocol over 25 years in a reference center in southern Brazil, and to correlate estimated full-scale IQ (FSIQ) scores with neurocognitive prognosis determinants, such as age at the start of treatment, disease severity, and maternal education.
MethodsStudy designThis was an observational, analytical, retrospective, and longitudinal cohort study, in which the primary outcome was to obtain estimated FSIQ scores of children with primary CH detected by the NS-PR, and secondarily, to assess possible correlations between estimated FSIQ scores and neurocognitive prognosis variables, such as age at the start of treatment, T4dx and maternal education. The study was approved by the Human Research Ethics Committee of the Hospital de Clínicas da Universidade Federal do Paraná (CHC-UFPR), number 3.113.007.
SettingThe study was conducted in the Pediatric Endocrinology Unit (UEP) of the CHC-UFPR. The NS-PR for CH started in the early 1990s and is performed exclusively at the laboratory of the Fundação Ecumênica de Proteção ao Excepcional (FEPE) in the city of Curitiba. All screened neonates are referred to UEP for diagnostic confirmation and treatment.
PatientsThe study group consisted of 458 children with confirmed CH detected between 1991 and 2014, who had at least one psychometric evaluation: Wechsler Preschool and Primary Scale of Intelligence – Revised (WPPSI-R) and/or Wechsler Intelligence Scale for Children-Third Edition (WISC-III). Patients with genetic syndromes, chronic pediatric diseases, and undefined etiology of CH were not included. All evaluations were consented by parents or guardians.
Data collection and definitionsIn Brazil, CH screening is performed by measuring TSH on filter paper. In NS-PR, screening TSH (mU/L) cut-off values have changed over the years, ranging from 20 (1990–1996) and 15 (1997–2003) to the current value of 10 for samples collected ≥ 48 h of life. Data obtained from medical records included: T4dx, fT4dx, and TSHdx, maternal education, CH etiology, age, and IQ scores at the first and second psychometric evaluations. Screening TSH was measured by immunofluorimetric assay (Auto-DELFIA, PerkinElmer, Turku, Finland); confirmatory TSH (0.49–4.67 mU/L), T4 (6–12 μg/dL), and fT4 (0.71–1.85 ng/dL) were measured by commercial kits (Abbott Laboratories, Lake Bluff, Illinois, USA). Patients underwent 131I or 99mTechnetium thyroid scintigraphy and T4, fT4, and TSH measurements for diagnostic confirmation, four weeks after l-T4 withdrawal at the age of three years. Patients with presumed athyreosis on scintigraphy underwent thyroid ultrasonography to confirm the absence of the gland.
All psychometric evaluations were performed individually by the same psychologist using Brazilian versions of two Wechsler Intelligence Scales.17,18 Patients aged 5.4 to 6.9 years were evaluated with four subtests (Information and Arithmetic from the Verbal scale; Block Design and Picture Completion from the Performance scale) of a WPPSI-R abbreviated version, from which a FSIQ score was estimated. The WPPSI abbreviated version has been validated for use in clinical and research settings and has demonstrated high reliability.19 Patients aged ≥ 7.0 years performed five standardized subtests of WISC-III (Information, Vocabulary, and Similarities from the Verbal scale; Block Design and Picture Completion from the Performance scale), which provided an estimate of FSIQ. Subtest scores have a mean of 10 and a standard deviation (SD) of 3. FSIQ scores of 100 and SD of 15 were considered within the normal range, and an FSIQ score < 70 in at least one psychometric test was defined as an intellectual deficit (ID).20
Statistical analysisThe software SPSS® IBM® Statistics, version 21, was used for statistical analyses. The results are expressed as mean±SD or median with ranges, with 95% confidence intervals. Student's t-test and analysis of variance (ANOVA) were used to analyze continuous variables with normal distribution, and Mann-Whitney and Kruskal-Wallis for asymmetric variables. The significance level was defined as p-value ≤ 0.05. A multiple logistic regression analysis was used to test the independent relationship between FSIQ (WPPSI-R and WISC-III) and T4dx and maternal education as predictor variables; for this analysis, age at the start of treatment was not included due to its asymmetric distribution.
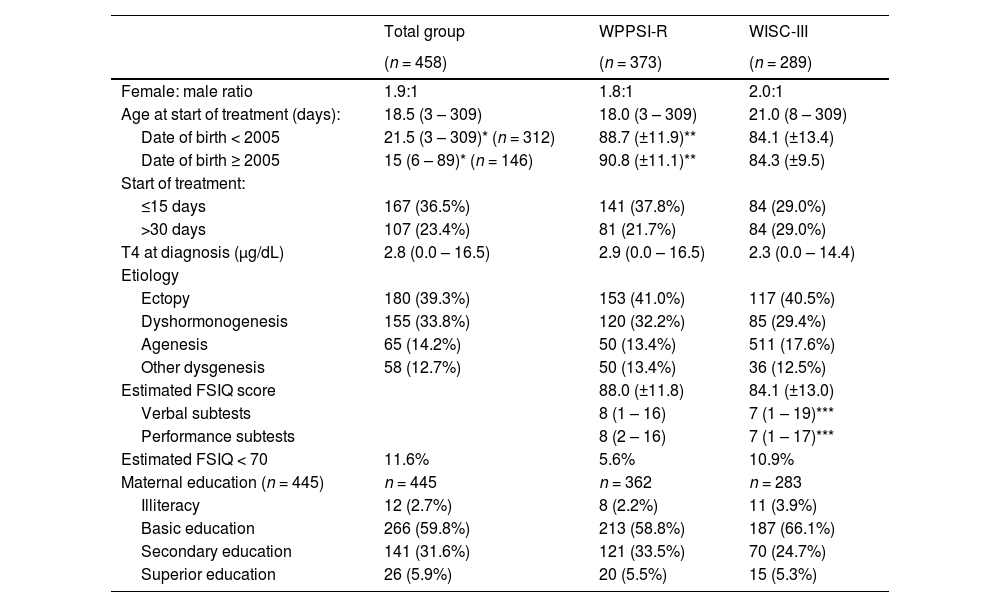
ResultsTable 1 shows the main characteristics of the cohort. Most patients (66.2%) had thyroid dysgenesis. TSHdx was > 75 mIU/L in 288 patients (62.8%); T4dx was < 3.0 μg/dL in 51.4% and ≥ 8.0 μg/dL in 13.8%; a higher prevalence of dyshormonogenesis (54.1%) was observed in the milder forms. The median age at the start of treatment was 18.5 (3–309) days. Maternal education was available for 445 patients (97.2%); the majority (59.8%) had only basic education and nearly 3% were illiterate.
Demographic characteristics, age at the start of treatment and estimated FSIQ score of patients with congenital hypothyroidism.
* p < 0.001; ** p = 0.002; *** p = 0.006.Data presented as mean (±SDs), median and range, n (%).WPPSI-R, Wechsler Preschool and Primary Scale of Intelligence – Revised; WISC-III, Wechsler Intelligence Scale for Children-Third Edition.
WPPSI-R was performed in 373 (81.4%) children (median age 5.6 ± 0.5 years), while 289 (63.1%) performed the WISC-III (median age 9.1 ± 1.4) (Table 1); 207 (45.6%) performed both tests. The verbal subtests scores were significantly lower than the performance subtests scores in the WISC-III assessment (p = 0.006, Table 1).
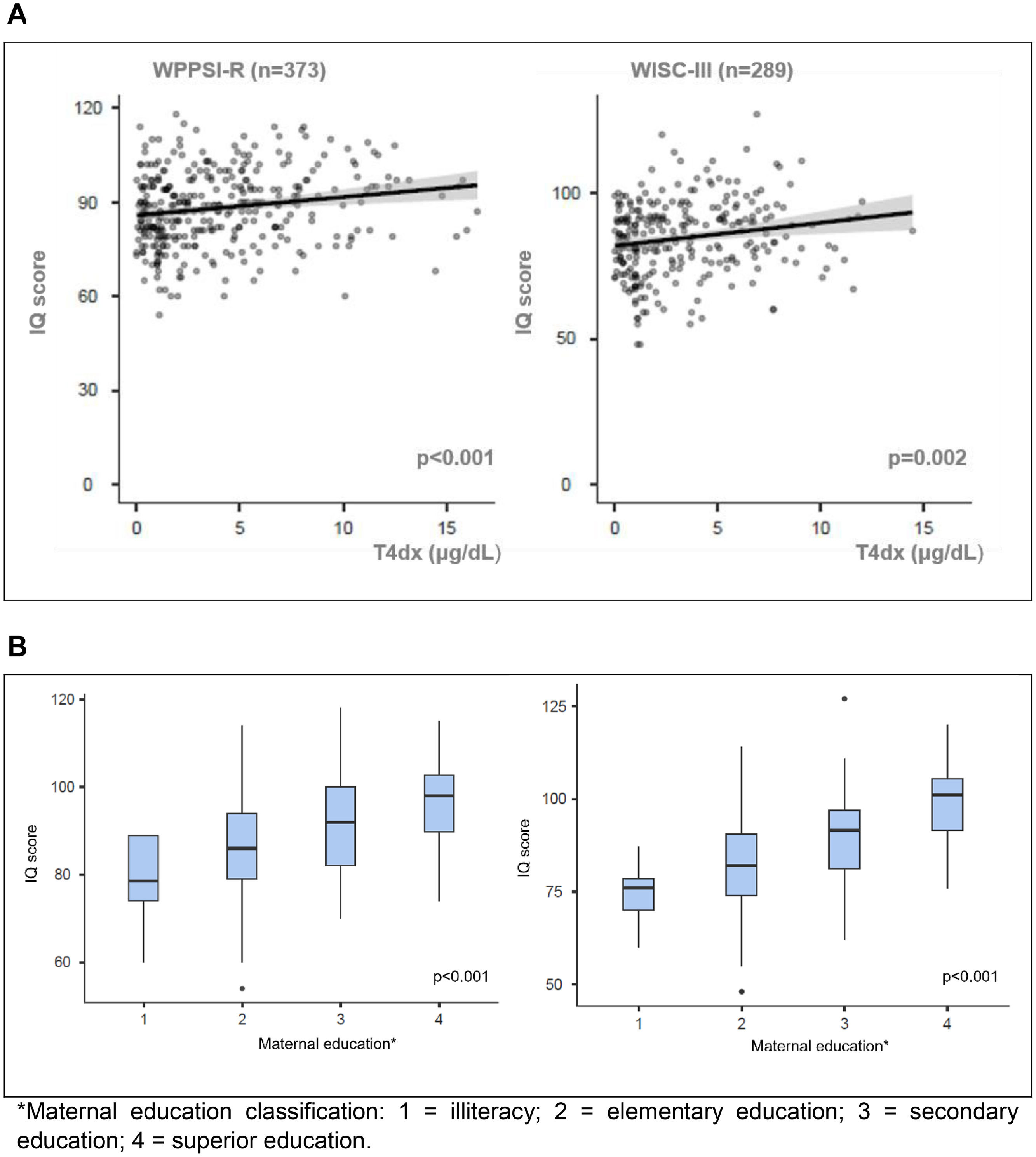
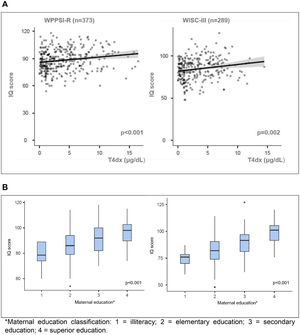
Estimated FSIQ scores were significantly correlated with T4dx (p < 0.001, r = 0.197 for WPPSI-R; p = 0.02, r = 0.183 for WISC-III) and with maternal education (p < 0.001 for both tests) (Figure 1A and 1B). There was a negative correlation between FSIQ and age at the start of treatment only in the WPPSI-R test (p = 0.02).
(A) Positive correlations of FSIQ scores with T4 at diagnosis (μg/dL) in WPPSI-R (r = 0.197) and WISC-III tests (r = 0.183). (B) Positive correlations of FSIQ scores with mother schooling in WPPSI-R (n = 362) and WISC-III (n = 283).
WPPSI-R, Wechsler Preschool and Primary Scale of Intelligence – Revised; WISC-III, Wechsler Intelligence Scale for Children-Third Edition.*Maternal education classification: 1 = illiteracy; 2 = elementary education; 3 = secondary education; 4 = superior education.
Since 2005, the median age at the start of treatment has significantly decreased (p < 0.001) (Table 1). Patients born ≥ 2005 (n = 146) performed better than those born < 2005 (n = 258) in the WPPSI-R (90.8 ± 11.1 vs. 88.7 ± 11.9, p = 0.002). In the younger group only 31 patients were old enough to perform the WISC-III and their FSIQ scores (84.3 ± 9.5) did not differ from those born < 2005 (84.1 ± 13.4). ID was more prevalent in the older group (15.1% vs. 6.5%, p < 0.001). The prevalence of mother illiteracy and basic education in the younger group was 1.4% and 43.8%, respectively, and 3.3% and 67.4% in the older group.
ID was identified in 11.6% of the whole cohort. In these patients, the median T4dx was 1.5 (0.4–14.5) and the median age at the start of treatment was 21.5 (8–92) days. Regarding maternal education, 9.6% were illiterate, 78.9% elementary school, 11.5% secondary education, and none had a superior level. Of the 21 patients with ID in the WPPSI-R (mean FSIQ score 64.3 ± 3.7), 15 (71.4%) performed WISC-III, in which 9 still scored less than 70 (59.2 ± 5.6). Of the 32 with FSIQ < 70 in the WISC-III (63.8 ± 5.2), 13 (40.6%) had performed the WPPSI-R test (FSIQ 76.6 ± 5.2).
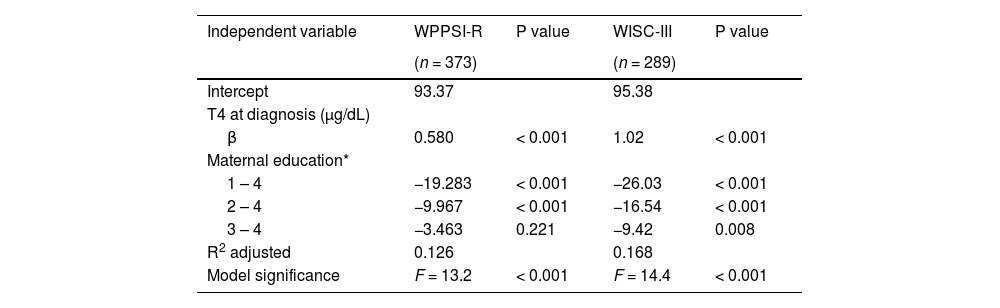
T4dx and maternal education were significantly and independently associated with cognitive levels, but maternal education was the most important variable for both tests (Table 2).
Results of multiple regression analysis with T4 at diagnosis (µg/dL) and maternal education as independent variables and WPPSI-R and WISC-III estimated FSIQ scores as dependent variable.
*Maternal education classification: 1 = illiteracy; 2 = elementary education; 3 = secondary education; 4 = superior education.WPPSI-R, Wechsler Preschool and Primary Scale of Intelligence – Revised; WISC-III, Wechsler Intelligence Scale for Children-Third Edition.
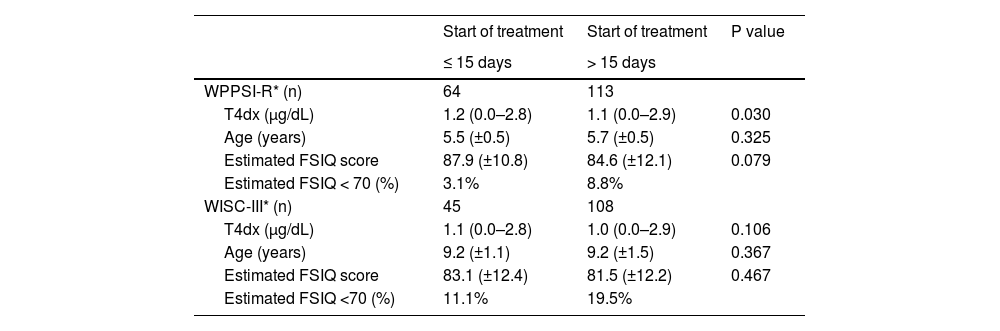
Table 3 shows FSIQ scores of patients with more severe CH (T4dx < 3.0 μg/dL), separated according to age at the start of treatment. FSIQ scores were not statistically different in either test. However, ID was more prevalent in those patients who started treatment > 15 days.
Estimated FSIQ scores of patients with T4dx<3.0 μg/dL according to age at start of treatment.
| Start of treatment | Start of treatment | P value | |
|---|---|---|---|
| ≤ 15 days | > 15 days | ||
| WPPSI-R* (n) | 64 | 113 | |
| T4dx (μg/dL) | 1.2 (0.0–2.8) | 1.1 (0.0–2.9) | 0.030 |
| Age (years) | 5.5 (±0.5) | 5.7 (±0.5) | 0.325 |
| Estimated FSIQ score | 87.9 (±10.8) | 84.6 (±12.1) | 0.079 |
| Estimated FSIQ < 70 (%) | 3.1% | 8.8% | |
| WISC-III* (n) | 45 | 108 | |
| T4dx (μg/dL) | 1.1 (0.0–2.8) | 1.0 (0.0–2.9) | 0.106 |
| Age (years) | 9.2 (±1.1) | 9.2 (±1.5) | 0.367 |
| Estimated FSIQ score | 83.1 (±12.4) | 81.5 (±12.2) | 0.467 |
| Estimated FSIQ <70 (%) | 11.1% | 19.5% |
To our knowledge, this is the largest cohort of children with primary CH with cognitive level assessment. It is also the first study to describe the cognitive level in a large group of CH children mainly of a low SES population.
The cognitive level was evaluated in 458 children (373 with WPPSI-R and 289 with WISC-III; 207 performed both tests). The mean estimated FSIQ score was 88.0 (±11.8) in the WPPSI-R and 84.1 (± 13.0) in the WISC-III, and ID was identified in 11.6% of patients. Treatment was started with a median age of 18.5 days; most patients (51.4%) had severe hypothyroidism, and. most mothers (59.8%) had only basic education. Correlation between age at the start of treatment and estimated FSIQ was found only in the WPPSI-R test. The cognitive level was independently and significantly associated with T4dx and maternal education in both tests, with the latter being the most important determining factor.
NS is considered an important medical intervention to prevent intellectual disability. Unfortunately, even three decades after its implementation in Brazil, NS national coverage is still estimated to be around 85%, due to technical and logistical difficulties in many regions.21 Since the beginning of the NS-PR in the early 1990s, progressive logistics improvement over the decades and guidance campaigns for health services and professionals have allowed achievements of high-standard NS quality indicators from 2005 onwards.5 The NS-PR also provides systematic psychometric evaluation, performed individually and by the same psychologist since the beginning of the program.
Disease severity, age at the start of treatment and maternal educationAs expected, patients with milder forms of CH had mainly dyshormonogenesis while most severely affected patients concentrated all cases of athyreosis. Disease severity has been recognized for decades as an important predictor of adverse neurocognitive outcomes.7,9,10,22 In the present cohort, FSIQ was significantly correlated with disease severity in both psychometric evaluations, highlighting the importance of thyroid hormone levels for neurological development.
It has been demonstrated that an earlier start of treatment combined with a high l-T4 dose, especially in more severe cases, contributes to better cognitive outcomes, and a normal FSIQ, that does not differ from unaffected siblings, may be achieved.3,4,23 In the present sample, age at start of treatment was a determining factor for better cognitive outcomes in severely affected patients only in the WPPSI-R. No correlation between FSIQ scores and age at the start of treatment was found in the results obtained with the WISC-III evaluation. It is possible that for older ages, when higher performances are required, this variable loses importance as a prognosis-determining factor and what prevails is the consequence of lack of exposure to thyroid hormones, probably since intrauterine life, and environmental stimuli, here partially represented by maternal education. Although in general, all patients start treatment with l-T4 dose of 10–15 µg/kg/day, individual data were not evaluated for this study. However, in a previous survey of a large group (n = 414) of CH patients routinely followed-up at UEP-CHC-UFPR mean initial dose was 11.7 ± 1.9 µg/kg/day.5
In every context, children´s cognitive development, opportunities, health, and behavior are strongly related to maternal education, which is significantly representative of SES. In the present study, maternal education appears an essential factor in determining the cognitive level, followed by T4dx.
NS improvement over the yearsIn a previous study of the same service carried out in 2005, both intelligence tests were applied on 43 unaffected patients’ siblings (mean age 7.2 ± 1.3), whose mean FSIQ scores (85.0 ± 14.4) were not significantly different from 120 patients (p = 0.06). These results have suggested that the cognitive level of patients was within the normality average of the studied population, considering the limitations related to their SES.16
There has been an improvement in the Brazilian SES level over the past three decades,24 which is closely related to an improvement in the population's educational level. Simultaneously, better quality indicators in the NS-PR and the observed increase in IQ scores due to the Flynn effect over the years should contribute to higher IQ scores achievements.11 However, a significant difference in cognitive level was only observed in the WPPSI-R test when the younger group was compared to the older group. It is possible that for older ages, as discussed above when higher cognition is required, the fact that the median age at the start of treatment has reduced is still not sufficient to raise IQ scores. Maybe it will be possible to observe higher estimated cognitive levels in patients during future assessments.
Below-average IQ levels and IDThe main points of concern in this study are the low FSIQ mean and high prevalence of ID of patients. In a societal context IQ level has been correlated with productive capacity, meaning that cognitive impairment is inversely related to personal economic gains, which leads to lower income, life expectancy reduction, and increases in societal expenditures for compensatory education.25
Approximately 1–3% of children worldwide receive the diagnosis of intellectual impairment due to a wide variety of etiologies,26 and in Brazil, it is estimated that 0.8–1.3% of the general population has some kind of intellectual disability.27 It has been previously demonstrated that children of low SES receive limited cognitive stimuli, are more exposed to environmental hazards such as malnutrition, iron deficiency, parasitic infection, and diarrhea, and in risk of inadequate parenting. Thus, SES affects cognitive performance through multiple factors simultaneously.12,28 In the present study the low level of maternal education was the main factor affecting the results.
In a Swiss group of 63 adolescents, FSIQ (WISC-R) was significantly lower than in controls after adjustment for SES, but no ID was described.7 The study of Rovet (n = 42), found only one case of ID (2.4%).6 The Norwegian study, which evaluated FSIQ (Wechsler Abbreviated Scale of Intelligence, WASI) in adults, showed that although FSIQ values were optimal (mean 102.4), they were significantly lower than in controls; ID was also not found and there were no individuals of lower socioeconomic class. It is suggested by the authors that the lack of influence of the SES in the results is also due to the relatively homogeneous Norwegian society. Also in the Dutch study (n = 82), no ID was found,1 which led them to suggest that possibly with further advancement in treatment strategies intellectual and motor deficits could disappear, and if deficits remain, they might be the consequence of the prenatal hypothyroid state. The authors could also add that in socioeconomically disadvantaged countries, these improvements may not be enough to achieve higher levels of intellectual outcomes.
In Brazil, a previous study evaluated 31 children with CH (WPPSI, n = 24; WISC, n = 7); none started treatment < 15 days and lower FSIQ values were associated with lower T4dx values and maternal education, which, in turn, was also associated with SES.13 In another study, an evaluation of 34 adolescents with CH (WISC-IV), the family's SES and caregiver's schooling along with the initial l-T4 dose was the most important determinant factors to cognitive performance.14 In South America, studies in Chile and Colombia emphasize the influence of SES as a limiting factor for cognitive outcomes.29,30 These data along with those from the present study strongly suggest that it is mandatory to seriously consider the weight of SES-related variables in low SES populations. Therefore, in developing countries, public policies aimed at education rate improvements may be as important as medical treatment protocols.
A strength of this study is a large number of children systematically evaluated at the same service and with psychometric tests carried out by the same professional over more than two decades. In addition to providing medical and neurocognitive information, the present results are linked with the historical evolution of the NS-PR. It is also the first large cohort of socioeconomically disadvantaged children with CH described in the literature.
The present study's results concerning CH main characteristics are similar to many longstanding studies in the literature, reaffirming the correlation of severe hypothyroidism with worse neurocognitive prognosis. The authors couldn´t demonstrate, however, that earlier treatment, especially before 15 days, may be neurologically more favorable for these severely affected patients. Yet, the authors are faced with the fact that the social inequalities of the studied country and the SES of most of the patients unfortunately may act as limiting factors for the benefits offered by the NS and adequate CH treatment.
The present limitations are related to the fact that it is a retrospective analysis and to the lack of a control group for IQ references and comparisons. Considering that IQ scores increase over the years as described by the Flynn effect,11 the authors compare estimated FSIQ scores of tests carried out over 25 years.
These data provide evidence that hypothyroidism severity is a strong cognitive level determinant in childhood. However, despite the normalization of FSIQ in most of the CH patients, a significant proportion of children still manifest low average and below-average FSIQ scores and even ID. Maternal education, which partially represents SES, followed by hypothyroidism severity were the main influencing factors at the cognitive level. These results suggest that, regardless of the medical and treatment protocols, investments in education are needed in order to obtain better cognitive outcomes in societies with great social inequality.
FundingThis study was self-funded.
Research ethics approvalHuman Research Ethics Committee of the Hospital de Clínicas da Universidade Federal do Paraná (CHC-UFPR), number 3.113.007, January 15, 2019.
Institution or service with which the work is associated for indexing in Index Medicus/MEDLINE: Complexo Hospital de Clínicas da Universidade Federal do Paraná (UEP – CHC – UFPR), Curitiba- Paraná – Brazil.