To investigate the clinical implications of Golgi glycoprotein 73 (GP73) and granulocyte colony-stimulating factor (G-CSF) in children with bronchopneumonia (BP).
MethodsSeventy-two children with BP (observation group) and 81 healthy children (control group) consecutively brought to the present study's hospital between June 2019 and October 2020 were enrolled. GP73 and G-CSF levels were determined to analyze their diagnostic value for pediatric BP. High-sensitivity C-reactive protein (hs-CRP) was also measured. The clinical implications of GP73 and G-CSF in pediatric BP complicated with respiratory failure and their connections with the inflammatory response were discussed.
ResultsGP73 and G-CSF levels were remarkably higher in the observation group (p < 0.05). The sensitivity and specificity of combined detection (GP73+G-CSF) in predicting pediatric BP were 72.22% and 86.42%, respectively (p < 0.001). GP73 and G-CSF, which are closely related to X-ray classification and complications in the observation group, decreased after treatment and were positively correlated with hs-CRP (p < 0.05), especially in children complicated with respiratory failure. Regression analysis identified the independence of the course of the disease, hs-CRP, X-ray classification, GP73, and G-CSF as influencing factors of respiratory failure in children with BP (p < 0.05).
ConclusionGP73 and G-CSF, with elevated levels in children with BP, are strongly linked to disease progression and are independent influencing factors of respiratory failure, which may be the key to diagnosing and treating pediatric BP in the future.
Pediatric bronchopneumonia (BP) has afflicted more than 43.6% of infants and young children worldwide, as it is the most prevalent infectious disease among this patient population, with a rising incidence in recent years. 1,2 Dominantly triggered by pathogenic bacterial infection, pediatric BP has the most significant impact on pulmonary function, 3 which can cause severe respiratory dysfunction in children or even a series of neurological, digestive, circulatory, and other systemic diseases, directly threatening the life safety of children. 4,5 Clinical guidelines on pediatric BP point out that early diagnosis and treatment are the keys to ensuring the healthy growth of children. 6 However, at present, the diagnostic conditions for the disease in the clinic are still minimal, with imaging technology as the main evaluation index, which makes it impossible to realize large-scale clinical screening. 7 Therefore, finding an effective scheme that can quickly identify pediatric BP has been a hot and challenging issue in clinical research for a long time.
Golgi glycoprotein 73 (GP73), which exists in the transmembrane protein of Golgi, is an ideal serum marker for the early diagnosis and recurrence assessment of liver diseases, with high specificity and sensitivity. 8,9 It also has a very significant evaluation effect on pancreatic cancer, viral hepatitis B, and other inflammatory diseases. 10,11 Granulocyte colony-stimulating factor (G-CSF) is the main effector cell mediating the hepatitis response, which regulates the inflammatory response and immune response of the body by recruiting and aggregating hepatic stellate cells. 12,13 Research has proposed that G-CSF is of great reference significance as a marker for the early diagnosis of tuberculosis. Based on previous research on the mechanism of action of GP73 and G-CSF, the authors speculate that they also have a certain connection with the occurrence and development of pediatric BP. Nevertheless, no research has been conducted to confirm this hypothesis.
Accordingly, in the face of the increasing incidence of pediatric BP, the authors preliminarily confirmed the clinical implications of GP73 and G-CSF in the disease through experiments, aiming to provide new directions for future research regarding pediatric BP diagnosis and treatment.
Materials and methodsStudy populationSeventy-two children with BP (observation group) and 81 healthy children (control group) were selected as research participants. They were consecutively admitted to the studiedhospital between June 2019 and October 2020. Inclusion criteria for observation group: age 1-6 years; confirmed diagnosis of pediatric BP after examination in the present hospital; first onset; complete case data; clear consciousness; high degree of cooperation from parents. Exclusion criteria included congenital respiratory tract malformation, allergic history, other viral or bacterial infections, congenital immunodeficiency, comorbidities such as liver, kidney, and other organ diseases, and drug allergy.
Inclusion criteria for the control group: age 1-6 years; no major medical history; routine examination results within the normal range.
Informed consent was signed by the next kin of each child, and the ethics committee of Ningbo Women and Children's Hospital approved this study.
X-ray classificationType Ⅰ: increased and thickened bilateral lung texture, without infiltrating alveoli or other special clinical manifestations; Type Ⅱ: the patchy shadow of the lungs spread from the hilum to the surroundings, and the texture of the lungs increased, thickened, and invaded the alveolar tissue; Type Ⅲ: alveolar obstruction occurred under the influence of mucous secretions, and the lesion showed substantial changes in the patchy exudate shadow, with translucent lung tissue; Type IV: the pulmonary infection lesion showed diffuse infiltration and developed into exudative pleurisy.
TreatmentAfter admission, children received routine treatment, such as oxygen inhalation, cough relief, expectorant, spasmolysis, and anti-infection, as well as symptomatic and complication prevention treatment after the pathogen of infection was confirmed. Furthermore, adequate rest was provided, and the position of the children was adjusted to promote sputum excretion. To prevent cross-infection, isolate treatment was also administered. Furthermore, to avoid acidosis and electrolyte disturbances, water and electrolytes were properly supplemented. In the case of dyspnea or arterial blood gas abnormalities, oxygen therapy was administered to children with relatively severe conditions, and noninvasive ventilation or mechanical ventilation was provided as needed.
Detection methodsVenous blood (5 mL) was divided into two parts. One part was centrifuged (1505 × g, 4 °C) for 10 min to obtain serum for the detection of GP73 (Kit purchased from Wuhan Yipu Biology, Serial number: CK-E11598) and G-CSF (Kit purchased from Jiangxi Aiboyin Biotech, Serial number: IB-E10040) levels by ELISA, and the specific operation was carried out in strict accordance with the kit instructions. The absorbance value of each well (450 nm) was determined using a microplate analyzer. One part was directly used to detect the high-sensitivity C-reactive protein (hs-CRP) in the blood using an automatic hematology analyzer.
Statistical analysisData were processed by SPSS 24.0 software. Categorical variables were recorded as (%) and analyzed by the chi-square test. Continuous variables were represented by (χ±s) and compared by independent samples t test, paired t test, or one-way ANOVA and SNK post hoc test, as appropriate. ROC analysis was utilized to assess the predictive value. Correction analysis was performed by the Pearson correlation coefficient, and the influencing factors were analyzed by multivariate logistic regression analysis. The significance level was p < 0.05.
ResultsComparison of clinical baseline dataA total of 153 subjects were enrolled. There were 72 children with BP and 81 healthy children. The ages of the children in the observation group (2.2 ± 1.4) and the control group (2.1 ± 1.2) were not significantly different (p > 0.05). The numbers of males and females in the observation group were 38 (52.78%) and 34 (47.22%) and 39 (48.15%) and 42 (51.85%) in the control group, respectively, and the ratio was not significantly different (p > 0.05). The detailed clinical baseline data of the observation group and the control group are shown in Supplementary Material 1, and it was found that the differences were not statistically significant (p > 0.05).
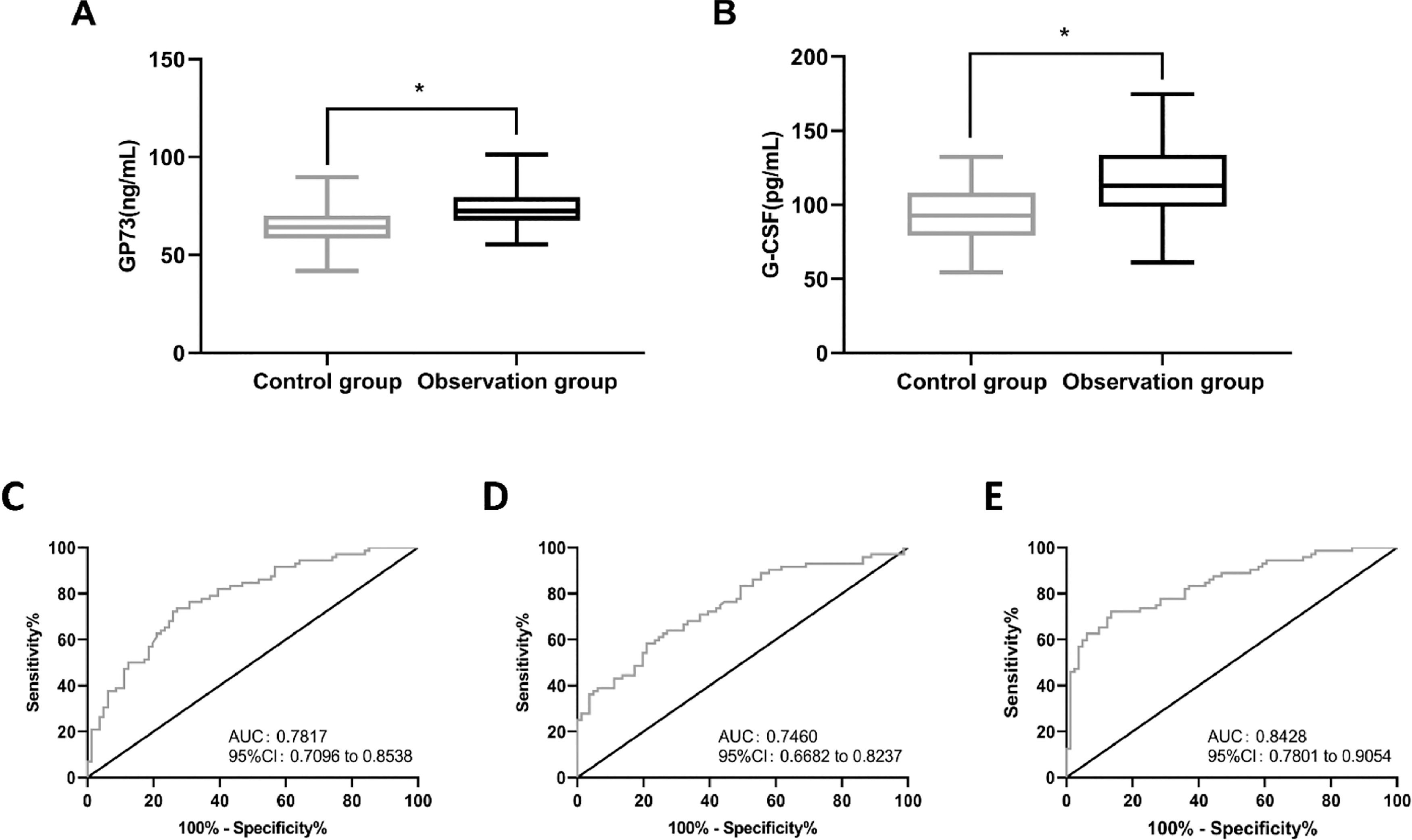
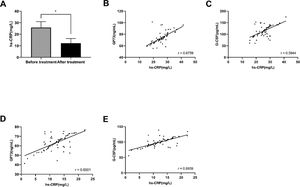
Levels and diagnostic value of GP73 and G-CSFGP73 and G-CSF levels were detected in the serum of the subjects by ELISA. The results showed that the observation group had a higher level of GP73 (79.89 ± 9.82 ng/mL) than the control group (p < 0.05) (Figure 1A). Similarly, the G-CSF (114.88 ± 23.68 pg/mL) levels were found to be higher in the observation group than in the control group (p < 0.05) (Figure 1B).
The levels and diagnostic value of GP73 and G-CSF. The levels of GP73 and G-CSF were examined in the subjects by ELISA. (A) The levels of GP73 in the control group and observation group. (B) The levels of G-CSF in the control group and observation group. (C) ROC of GP73 in predicting BP in children; (D) ROC of G-CSF in predicting BP in children; (E) ROC of GP73 combined with G-CSF in predicting BP in children. * indicates p < 0.05 in comparison with the control group.
Next, ROC analysis was performed to assess the diagnostic value of GP73 and G-CSF. The results showed that when GP73 was greater than 73.61 ng/mL, the sensitivity and specificity to predict BP were 73.61% and 72.84%, respectively (p < 0.001) (Figure 1C). When G-CSF levels were greater than 109.80 pg/mL, the sensitivity and specificity of G-CSF to predict BP were 58.33% and 79.01%, respectively (p < 0.001) (Figure 1D). The levels of GP73 and G-CSF in the two groups were then entered into SPSS, and the formula for the joint detection of GP73 and G-CSF was obtained by binary logistic regression analysis, which was Log(P) = -13.368 + 0.125 × GP73 + 0.045 × G-CSF. The subsequent ROC analysis revealed that when Log(P) > 0.5636, the sensitivity and specificity of GP73 + G-CSF in predicting BP were 72.22% and 86.42%, respectively (p < 0.001) (Figure 1E).
Correlation of GP73 and G-CSF with the pathology of pediatric BPGP73 was significantly associated with X-ray classification and complications (p < 0.05), whereas G-CSF was significantly associated with disease course, X-ray classification, and complications (p < 0.05) (Supplementary Material 2).
Changes in GP73 and G-CSF pre- and posttreatmentThe posttreatment levels of both GP73 and G-CSF in the observation group were significantly lower than the pretreatment levels. The levels of GP73 in the observation group were 79.89 ± 9.82 ng/mL prior to treatment but decreased significantly to 63.32 ± 7.78 ng/mL following treatment (p < 0.05) (Supplementary Material 3A). The G-CSF levels in the observation group were 114.88 ± 23.68 pg/mL before treatment, and they were significantly reduced to 95.58 ± 14.10 pg/mL after treatment (p < 0.05) (Supplementary Material 3B).
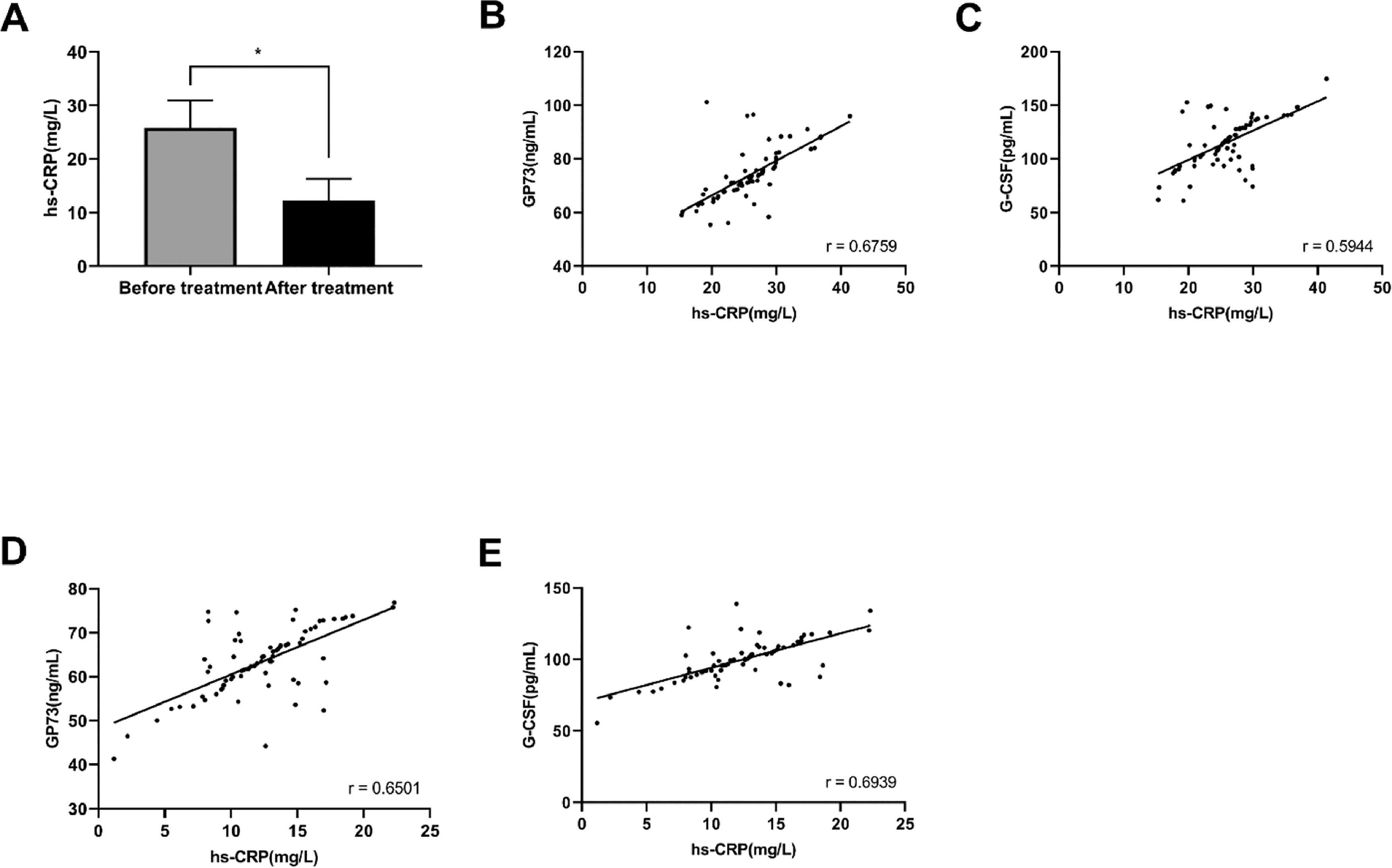
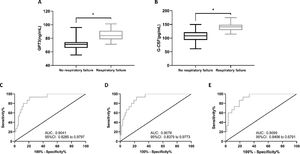
Correlation of GP73 and G-CSF with the inflammatory process of pediatric BPThe levels of hs-CRP in the observation group before the treatment were 25.81 ± 5.15 mg/L, and after the treatment, the levels of hs-CRP decreased significantly (12.26 ± 4.07 mg/L) (p < 0.05) (Figure 2A). Pearson correlation coefficient analysis was performed to assess the correlation of hs-CRP with GP73 and G-CSF pre- and posttreatment. The results showed that hs-CRP was positively correlated with GP73 and G-CSF before treatment (p < 0.05) (Figure 2B and C). Similarly, a positive correlation of hs-CRP with GP73 and G-CSF after the treatment was observed (p < 0.05) (Figure 2D and E).
Correlation of GP73 and G-CSF with the inflammatory process of pediatric BP. (A) hs-CRP levels in the observation group before and after treatment; * indicates p < 0.05 in comparison with before treatment. (B-E) Pearson correlation coefficient analysis was performed to assess the correlation of hs-CRP with GP73 and G-CSF pre- and posttreatment. (B) correlation between GP73 and hs-CRP before treatment; (C) correlation between G-CSF and hs-CRP before treatment; (D) correlation between GP73 and hs-CRP after treatment; (E) correlation between G-CSF and hs-CRP after treatment.
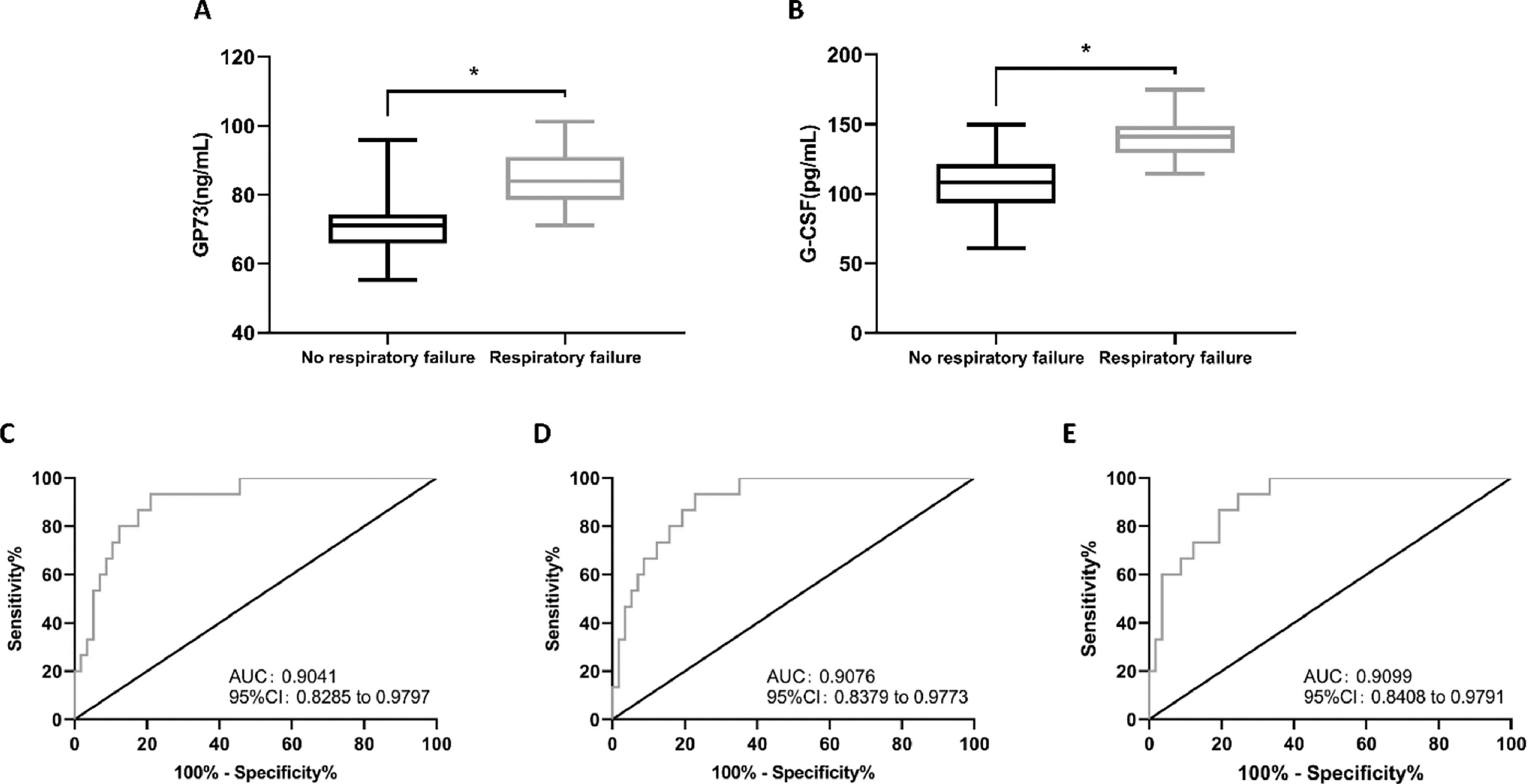
The authors evaluated the GP73 and G-CSF levels in children who experienced respiratory failure and those without respiratory failure. The results showed that in the observation group, 15 children developed respiratory failure during treatment. The pretreatment GP73 and G-CSF levels in children with respiratory failure were 85.18 ± 8.59 ng/mL and 140.99 ± 14.38 pg/mL, respectively, which were significantly higher than those in children without respiratory failure (p < 0.05) (Figure 3A and B).
GP73 and G-CSF levels, as well as their association with respiratory failure and predictive value for respiratory failure in children with BP. (A) GP73 levels were found to be higher in children with respiratory failure than in those without respiratory failure. (B) The levels of G-CSF were higher in children with respiratory failure than in children without respiratory failure. * indicates p < 0.05 in comparison with the no respiratory failure group. (C) ROC of GP73 in predicting respiratory failure in children with BP; (D) ROC of G-CSF in predicting respiratory failure in children with BP; (E) ROC of GP73 combined with G-CSF in predicting respiratory failure in children with BP.
The authors used ROC analysis to determine the predictive value of GP73 and G-CSF in children with BP for respiratory failure. The results demonstrated that when GP73 > 75.28 ng/mL, the sensitivity and specificity in predicting BP were 93.33% and 78.95%, respectively (p < 0.001) (Figure 3C). In addition, when G-CSF > 122.20 pg/mL, the sensitivity and specificity in predicting BP were 93.33% and 77.19%, respectively (p < 0.001) (Figure 3D). Next, the GP73 and G-CSF levels were substituted into SPSS for binary logistic regression analysis, and the combined detection formula of GP73 and G-CSF was obtained as Log(P) = -14.097 + (-0.060 × GP73) + (0.138 × G-CSF). The subsequent ROC analysis identified that when Log(P) > 0.1310, the sensitivity and specificity of the combined formula for predicting BP were 93.33% and 75.44%, respectively (p < 0.001) (Figure 3E).
Related factors affecting respiratory failure in children with BPAccording to the univariate logistic regression analysis, age, disease course, hs-CRP, X-ray classification, complications, GP73, and G-CSF were all factors contributing to respiratory failure in children with BP (p < 0.05). Multivariate logistic regression analysis revealed that the course of the disease, hs-CRP, X-ray classification, GP73, and G-CSF were all independent factors contributing to respiratory failure in children with BP (p < 0.05) (Table 1).
Related factors affecting respiratory failure in children with BP.
Pediatric BP is a common disease that affects children's life safety. Clinically, its etiology is closely related to the living environment, genetic factors, and nutrition intake. 14 The onset of pediatric BP is usually extremely rapid and may develop into severe pneumonia if not treated in a timely and effective manner, further increasing the risk of the disease. 15 At present, efforts are being made to explore sensitive markers of BP at home and abroad, aiming to improve the early detection rate of pediatric BP, but no significant breakthrough has been made yet. 16 This research, by analyzing the clinical implications of GP73 and G-CSF in children with BP, can lay a reliable foundation for the two as keys to the future diagnosis and treatment of pediatric BP.
First, the authors detected peripheral blood GP73 and G-CSF in cases and controls and determined their elevated levels in cases, which was consistent with the results of previous studies on the expression profiles of the two, 17,18 suggesting that both of them may interfere with BP onset and progression in children. GP73, as a Golgi transmembrane protein, has been found to be expressed in various organs, such as the liver, stomach, and peripheral blood, to varying degrees, but its mechanism of action has not yet been fully defined. 19 Mao and Wang demonstrated that GP73 inhibited epithelial cell proliferation and differentiation; additionally, it can act as a negative regulator of host innate immunity, inhibiting the host immune response and increasing the risk of pathogen infection. 20,21 Therefore, GP73 may be crucial in pediatric BP, a disease largely caused by decreased immunocompetence and pathogen infection. While G-CSF is primarily produced by T lymphocytes and macrophages, it can induce granulocyte aggregation by binding to target cell receptors. 22 Hoshina et al. indicated that G-CSF can prolong the life cycle of eosinophils by enhancing their adsorption and aggregation on vascular endothelium at inflammatory sites. In addition, it is able to release chemical toxicity by activating eosinophils in the human body, causing tissue damage and increasing lung susceptibility. 23,24 In renal ischemia-reperfusion injury, the continuous increase in G-CSF constantly stimulates aggravation of the inflammatory response and tissue damage, resulting in long-term incurable disease. 25 The authors speculate that in children with BP, the lung tissue is damaged by the invasion of foreign pathogens, which leads to a continuous increase in G-CSF and acceleration of BP. Then, the authors analyzed their diagnostic value for pediatric BP, which is the key to all BP research. 26 Compared with the current pediatric BP diagnosis scheme, the advantages of blood markers lie in the convenience of access, rapid detection, convenient preservation, and wide range of sample screening at any time. Thus, the early detection rate of BP is improved, and the treatment time for children is shortened. The present study's findings showed that both GP73 and G-CSF were effective in predicting the occurrence of BP, and the specificity of their combined detection reached 86.42%, demonstrating that GP73 and G-CSF have the potential to become diagnostic markers of pediatric BP in the future.
To further understand the clinical implications of GP73 and G-CSF in pediatric BP, the authors analyzed the correlation of the two with patient pathology. The results identified that GP73 and G-CSF, which are closely related to X-ray classification and complications in OG, decreased after treatment and were positively correlated with hs-CRP, especially in children with respiratory failure. hs-CRP, as one of the most sensitive indicators of inflammatory conditions in the human body, is also a common observation indicator for pediatric BP. 27 In a previous study, hs-CRP was found to have a trend of positive correlation with G-CSF and G-CSF mobilization stimulated an overactivation of inflammation in ischemic cardiomyopathy. 28 Both GP73 and G-CSF levels correlated well with hs-CRP levels, implying that hs-CRP could also reflect the progression of BP and be easily detected. To the best of our knowledge, the correlation between GP73 and hs-CRP levels has not been investigated. In future studies, the correlation of GP73 and G-CSF levels with hs-CRP levels could be useful for detecting BP. All the above results fully demonstrate that GP73 and G-CSF are closely related to pediatric BP progression, which further confirms their great potential value in the disease.
Apart from that, as a kind of lung injury disease with rapid onset, the effect of the pathogen on lung function is the most direct pathological manifestation of pediatric BP. 29 Respiratory failure, a critical complication that directly threatens the life safety of children, is also one of the most common complications of pediatric BP. 30 Therefore, if the significance of GP73 and G-CSF in children with BP complicated by respiratory failure can be further proven, it will provide an important guarantee for the safety of children in the future. In subsequent studies, the authors found that GP73 and G-CSF were higher in children with BP complicated with respiratory failure than in those without respiratory failure, and their predictive value for respiratory failure was extremely significant, which preliminarily confirmed the above stated viewpoint. However, in this experiment, GP73 combined with G-CSF was not as effective as single detection in predicting BP respiratory failure. The reason, the authors speculate, might be that the effect of GP73 and G-CSF on predicting respiratory failure in BP is already very significant, so the effect will not be further enhanced by the combination of the two. On the other hand, it may be that ROC analysis usually requires large case data to be more accurate, while the number of cases included in this study is small, resulting in contingency calculations. Finally, through logistic regression analysis, the authors found that independent of the course of the disease, hs-CRP, X-ray classification, GP73, and G-CSF were factors contributing to respiratory failure in children with BP, which reverified the significance of GP73 and G-CSF in the disease.
As previously stated, due to the small number of participants included, statistical calculations may contain errors. Additionally, because this study did not include a more detailed grouping design for children with BP, the authors will investigate the significance of GP73 and G-CSF in pediatric BP with different pathogens and disease courses in the future. Additionally, due to a dearth of in vitro experiments, the authors are unable to confirm the precise mechanism by which GP73 and G-CSF act in pediatric BP. The preceding are critical points that merit further discussion in the future.
ConclusionGP73 and G-CSF, with elevated levels in children with BP, are strongly linked to disease progression and are the factors contributing to respiratory failure, which may be the key to diagnosing and treating pediatric BP in the future.
FundingNone.