To verify the prevalence of the offer of ultra-processed foods (UPFs), and to analyze their associated factors in the child's first year of life.
MethodsCross-sectional study with 119 mother-infant pairs. At 5.5 months of the child, the mothers received guidance on complementary feeding (CF) according to three methods: Parent-Led Weaning (PLW), Baby-Led Introduction to SolidS (BLISS), or mixed (a combination of PLW and BLISS). At nine and 12 months, the mothers answered a questionnaire about the offer of UPFs. The NOVA classification, which classifies foods according to the nature, extent, and purposes of the industrial processes to which they are subjected, was used to list the UPFs. Descriptive statistics and multivariate Poisson regression, following a multilevel hierarchical model according to the proximity to the outcome, were used to estimate the association between dependent and independent variables.
ResultsThe prevalence of UPF consumption was 63% (n = 75) in the first year of life. Receiving guidance on healthy CF in the BLISS method showed to be a protective factor for offering UPFs (RR 0.72; CI95 0.52-0.99). Attending less than six prenatal consultations was a risk factor for the UPFs provision (RR 1.39; CI95 1.07-1.80).
ConclusionThe prevalence of UPFs offered in the first year of life in this study can be considered high, and future interventions aimed at avoiding UPFs offered in this population should consider the CF method.
The period of food introduction (FI) is called complementary feeding (CF) and starts at six months of age, with the readiness of the digestive system development and the coordination of the oral cavity to receive new foods.1,2 It represents a change in eating habits based on breast milk (BM) for a varied diet, with an increasing number of healthy foods, maintaining the supply of BM for up to two years or more.3
Commonly, at the beginning of CF, children receive mashed foods offered with a spoon by an adult. This method of feeding is also called Parent-Led Weaning (PLW) and is majority guided by the adult that is offering the food.4 More recently, the new Brazilian Food Guidelines for Children under Two Years suggests that soft foods shaped in large pieces could be offered for children from six months of age on to handle and that food has its consistency gradually increased until, at twelve months of life, it reaches the food consistency of the rest of the family, which characterizes participatory feeding.4
Approaches without the caregiver's interference at the time of feeding have been studied, such as the technique proposed by New Zealand scholars called Baby-Led Introduction to SolidS (BLISS), in which the child is encouraged to self-feed from six months of age, with foods cut into strips or sticks.5 This method is a modified version of a technique called Baby-Led Weaning (BLW), which also involves the child taking food to the mouth by themselves, with the difference that, in the BLISS technique, additional recommendations were included to avoid potential disadvantages of the BLW method regarding growth deficiency due to insufficient energy and iron intake, in addition to choking risk.6
On the other hand, in opposition to healthy CF recommendations, infants have been exposed to food products based on industrial formulations called ultra-processed foods (UPFs).7,8 Brazil was a pioneer in categorizing foods according to the NOVA classification, which is a tool that groups food according to the level of processing it went through before reaching the consumer's table. This includes physical, biological, and chemical processes, which can occur after food is harvested or after food is separated in nature. The foods are categorized into fresh or minimally processed, processed culinary ingredients, processed foods, and UPFs. The UPFs are defined as those produced mostly with substances extracted from food, derived from food constituents, or synthesized in a laboratory and whose purpose is to imitate the sensory qualities of unprocessed foods.9
Its consumption during FI is considered an unsuitable dietary practice, as it is strongly associated with long-term health-associated factors, which can affect the child's growth and development, as well as unfavorable outcomes up until adulthood.10 Studies have associated UPF consumption with hypercholesterolemia (in children),11 overweight and obesity (in all ages),12 metabolic syndrome (in adults),13 and death from cardiovascular disease and stroke (in all ages).4
Although studies describe the negative health impacts of UPFs,12-14 and the increasing offer at early ages,15 studies evaluating factors associated with UPFs consumption are scarce. This study aimed to verify the prevalence and to analyze the associated factors with the consumption of UPFs in children´s first year of life.
MethodCross-sectional study nested in a randomized clinical trial (RCT) comparing three different CF methods in mother-infant pairs: (A) strict PLW;4,16 (B) strict BLISS5; and (C) Mixed method: a combination of PLW and BLISS created especially for this study.17,18
Participants were recruited through the internet on social networks, pages, and groups aimed at mothers. Those interested in participating in the study contacted the researcher by telephone. The researcher verified the inclusion criteria: mothers living in Porto Alegre, Rio Grande do Sul, Brazil, or nearby cities, with healthy singleton infants born at term, with birth weight ≥ 2500 g, between zero and four months of life, and who had not yet started the CF process.
After signing the consent form, participants were sequentially numbered and had their names entered into a randomization list of three blocks and equal numbers, previously computer-generated (http://www.randomization.com) by blinded research staff. Only at the time of the first intervention, the mothers were informed of their group allocation. Assessment data were collected by a different researcher from the one responsible for the intervention, blinded to the allocation group, in a different room.
The intervention occurred according to the previously published study protocol17,18 and was carried out at five and a half months of the child, in a private nutrition office equipped with an experimental kitchen, where a previously trained nutritionist prepared meals and instructed the mothers for 45 minutes on the method to which they were assigned. In addition to the method of introducing CF, the intervention addressed the recommendations for promoting healthy eating according to the Food Guidelines for Children under Two Years,4,16 including the recommendation to avoid UPFs before 24 months of age. Mothers also received reference folders containing the same guidelines provided in the intervention.
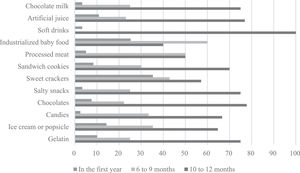
Data collection took place at nine and 12 months of the child's life. Planning included home visits, but due to the COVID-19 pandemic, part of the sample had to answer online questionnaires. To assess the offer of UPFs, the recommendations of the Ministry of Health of Brazil and the NOVA classification were used,9,19 and families were asked if the child had ever been exposed to a list of UPFs and, if so, at what age. The foods considered UPFs were chocolate milk, processed juice, soft drinks, processed porridge, processed meats (sausages), wafer-type or sandwich cookies, sweet cookies, savory snacks, chocolates or bonbons, candies or lollipops, jellies or instant puddings, milk-based ice cream or popsicles, and artificially flavored popsicles.
Maternal covariates were collected using a structured questionnaire and consisted of the mother's age (20 to 35 or ≥ 35 years), years of schooling (≥ 15 or < 15 years), mother working outside the home (yes or no), household monthly income (Brazilian reais) (> 3,000.00, 3,000.00 to 10,000.00 and > 10,000.00), number of prenatal consultations (< 6 or ≥ 6), marital status (with or without a partner), body mass index (BMI) calculated at the time of the intervention – adequate, overweight or obese),20 parity (primiparous or multiparous), help when cooking meals (yes or no), cohabitation with the father (yes or no), and with the maternal grandmother of the infant (yes or no). The infant's data analyzed were sex (female or male), exclusive breastfeeding (EBF) up to the sixth month (yes or no), breastfeeding (BF) up to 12 months of life (yes or no), pacifier use (yes or no) and bottle feeding (yes or no), method of food introduction according to randomization (PLW, BLISS or Mixed) and whether the child attended preschool (yes or no).
BF variables were categorized according to the World Health Organization (WHO) into EBF, when the child received only BF, without any other liquid or solid, except supplements and medications. And BF, when the child was breastfed, regardless of other liquids or solids provided.21
The sample calculation of the RCT primary outcome (BMI for age) used a unit standard deviation equal to 1, with a power of 80% and a significance level of 5%. Thus, the sample calculation for a difference of half a standard deviation was 48 mother-infant binomials for each of the three intervention groups, totaling a sample of 144 binomials. For this, the WinPepi® software version 11.65 was used. The definition of the sample size considered previous studies on the subject.5
The Statistical Package for the Social Sciences® (SPSS) program version 21.0 was used for double data entry and subsequent validation and data analysis. In the descriptive analysis, categorical variables were expressed as absolute numbers and percentages, and continuous variables were expressed as mean and standard deviation (± SD) or median and interquartile range [P25 – P75].
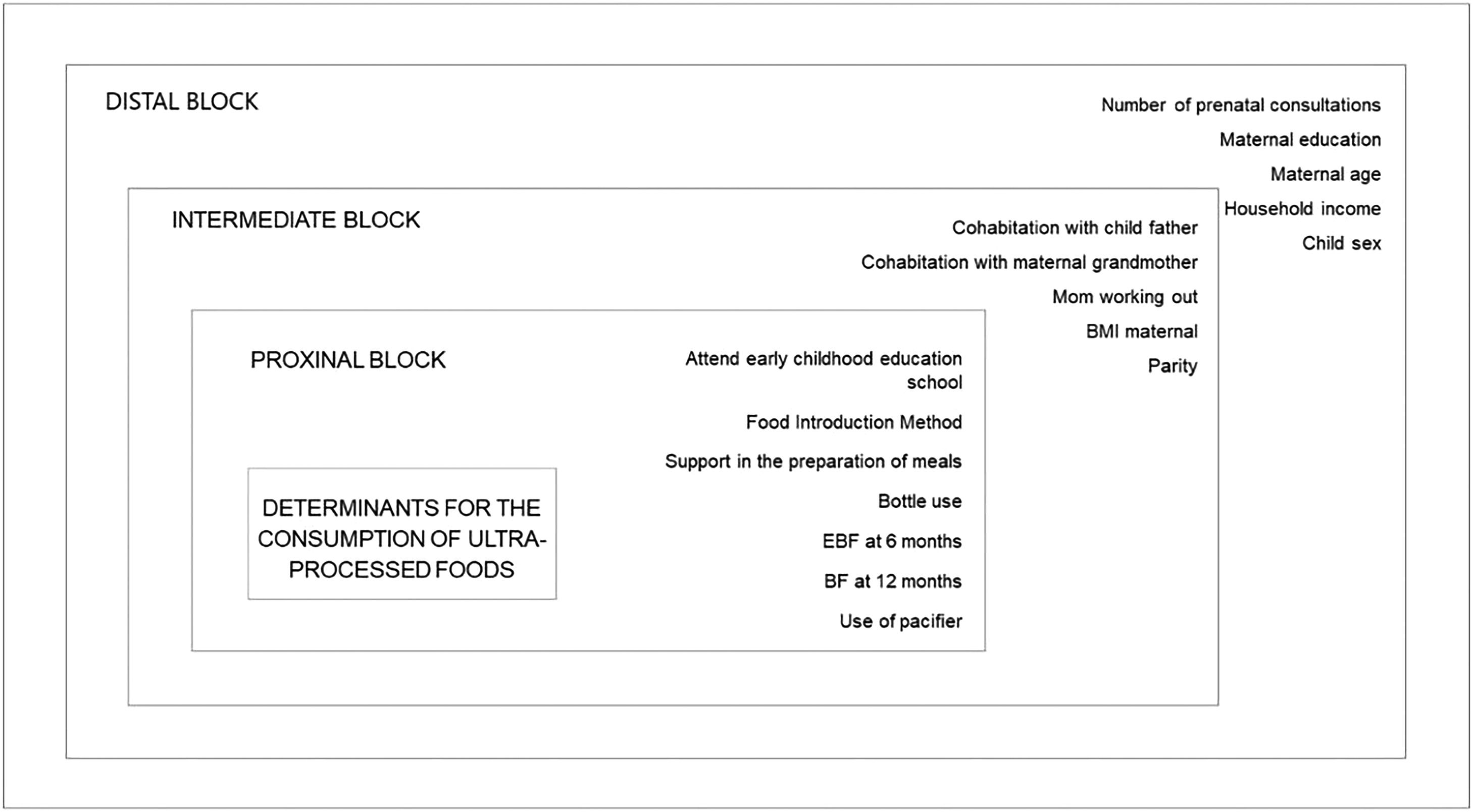
A conceptual hierarchical model was drafted (Figure 1) based on a similar study,22 through the grouping into three blocks of influence by proximity to the result. Initially, analyzes were conducted to measure the association between the outcome (offer of UPFs) and the variables of interest in each block, using univariate Poisson regression. The distal block variables that reached a significance level of p < 0.20 in the univariate analysis were submitted to multivariate regression, that is, they were submitted together to Poisson regression (interblock analysis), with only the variables that reached a significance level of p < 0.10 in the multivariate analysis of the distal block remaining in the model, for the adjustment of the distal intermediate block.
Hierarchical model proposed to assess factors associated with the consumption of ultra-processed foods by infants in Porto Alegre and the metropolitan area, Rio Grande do Sul, Brazil, 2021. Source: Adapted from LOPES et al, 2020.22 BMI: Body mass index; EBF: exclusive breastfeeding; BF: breastfeeding.
Then, the variables contained in the second block (distal intermediate level) that reached a significance level of p < 0.20 in the univariate analysis were submitted to multivariate Poisson regression together with the variables of the distal block that reached a significance level of p < 0.10 in the multivariate analysis, and so on. The model predicted that, once the variable reached a significance level of p < 0.10 in the intra-block analysis, it would remain in the model until the end, adjusting the interactions between the variables of the other blocks, as they were considered possible confounding factors. The degree of association between the different variables and the outcome was estimated by incidence ratio and their respective 95% confidence intervals (95% CI), with a p-value < 0.05 being considered significant.
This study was approved by the Research Ethics Committee of Hospital de Clínicas de Porto Alegre (under number 2019-0230, CAAE: 1537018500005327) and the RCT is registered with the Brazilian Registry of Clinical Trials (ReBEC): RBR- 229SCM.
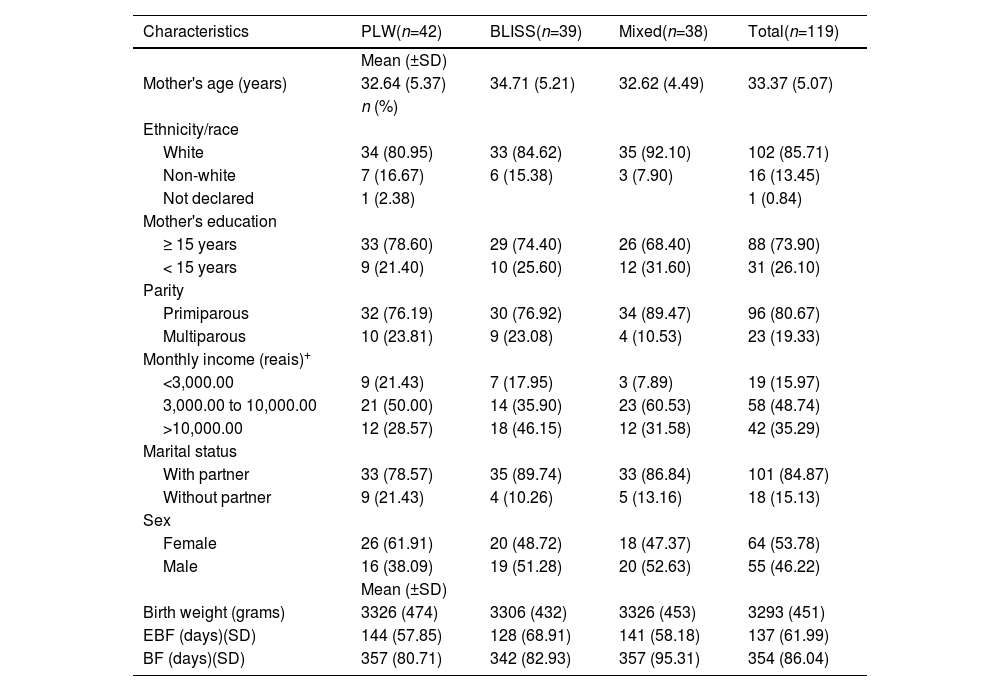
ResultsAt nine months, 132 participants answered the questionnaire, and at 12 months, 119 participants. Of these forms, according to Table 1, 50.74% (n = 67) at nine months and 80.30% (n = 94) at twelve months were collected online. Most mothers declared themselves white 85.71% (n = 102), with a mean age of 33.37 years (± 5.07), 73.9% (n = 88) had 15 years of schooling or more and and 48.7% (n=58) of the families have a family income of 3,000.00 to 10,000.00 Brazilian reais.
Characterization of the sample of mothers and infants in Porto Alegre and the metropolitan area, Rio Grande do Sul, Brazil, 2021.
| Characteristics | PLW(n=42) | BLISS(n=39) | Mixed(n=38) | Total(n=119) |
|---|---|---|---|---|
| Mean (±SD) | ||||
| Mother's age (years) | 32.64 (5.37) | 34.71 (5.21) | 32.62 (4.49) | 33.37 (5.07) |
| n (%) | ||||
| Ethnicity/race | ||||
| White | 34 (80.95) | 33 (84.62) | 35 (92.10) | 102 (85.71) |
| Non-white | 7 (16.67) | 6 (15.38) | 3 (7.90) | 16 (13.45) |
| Not declared | 1 (2.38) | 1 (0.84) | ||
| Mother's education | ||||
| ≥ 15 years | 33 (78.60) | 29 (74.40) | 26 (68.40) | 88 (73.90) |
| < 15 years | 9 (21.40) | 10 (25.60) | 12 (31.60) | 31 (26.10) |
| Parity | ||||
| Primiparous | 32 (76.19) | 30 (76.92) | 34 (89.47) | 96 (80.67) |
| Multiparous | 10 (23.81) | 9 (23.08) | 4 (10.53) | 23 (19.33) |
| Monthly income (reais)+ | ||||
| <3,000.00 | 9 (21.43) | 7 (17.95) | 3 (7.89) | 19 (15.97) |
| 3,000.00 to 10,000.00 | 21 (50.00) | 14 (35.90) | 23 (60.53) | 58 (48.74) |
| >10,000.00 | 12 (28.57) | 18 (46.15) | 12 (31.58) | 42 (35.29) |
| Marital status | ||||
| With partner | 33 (78.57) | 35 (89.74) | 33 (86.84) | 101 (84.87) |
| Without partner | 9 (21.43) | 4 (10.26) | 5 (13.16) | 18 (15.13) |
| Sex | ||||
| Female | 26 (61.91) | 20 (48.72) | 18 (47.37) | 64 (53.78) |
| Male | 16 (38.09) | 19 (51.28) | 20 (52.63) | 55 (46.22) |
| Mean (±SD) | ||||
| Birth weight (grams) | 3326 (474) | 3306 (432) | 3326 (453) | 3293 (451) |
| EBF (days)(SD) | 144 (57.85) | 128 (68.91) | 141 (58.18) | 137 (61.99) |
| BF (days)(SD) | 357 (80.71) | 342 (82.93) | 357 (95.31) | 354 (86.04) |
SD: Standard deviation; PLW: Parent-Led Weaning; BLISS: Baby-Led Introduction to SolidS; Family income expressed in reais (BRL)
The mean time of EBF was 137 days (± 61.99) and was practiced by a similar number of mothers between the intervention groups (p = 0.865); in which the PLW was 36.90 % (n = 24), BLISS was 30.80% (n = 20), and mixed, 32.30% (n = 21). Regarding BF, the mean was 354 days (86.04), with no statistically significant difference between the methods (p = 0.784)
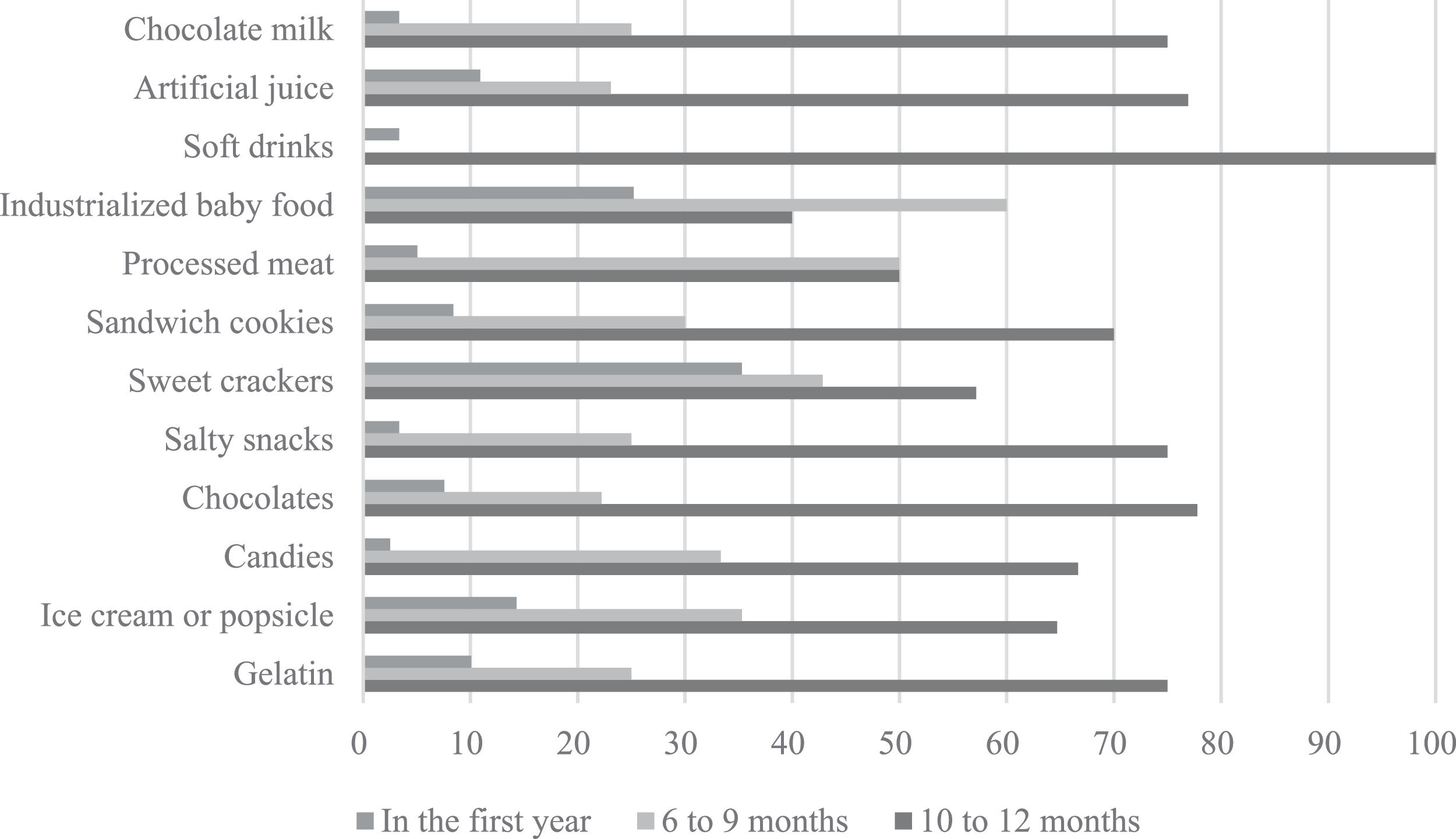
The prevalence of mothers who offered at least one type of UPFs was 63.0% (n = 75), as follows: 73.8% (n = 31) in PLW, 53.8% (n = 21) in BLISS, and 60.5% (n = 23) in the mixed type. The mean (± SD) for the introduction of at least one type of UPF was 340 days (± 5.76) in PLW and 355 days (± 3.16) in BLISS and Mixed. The prevalence of offer of each type of UPF is described in Figure 2.
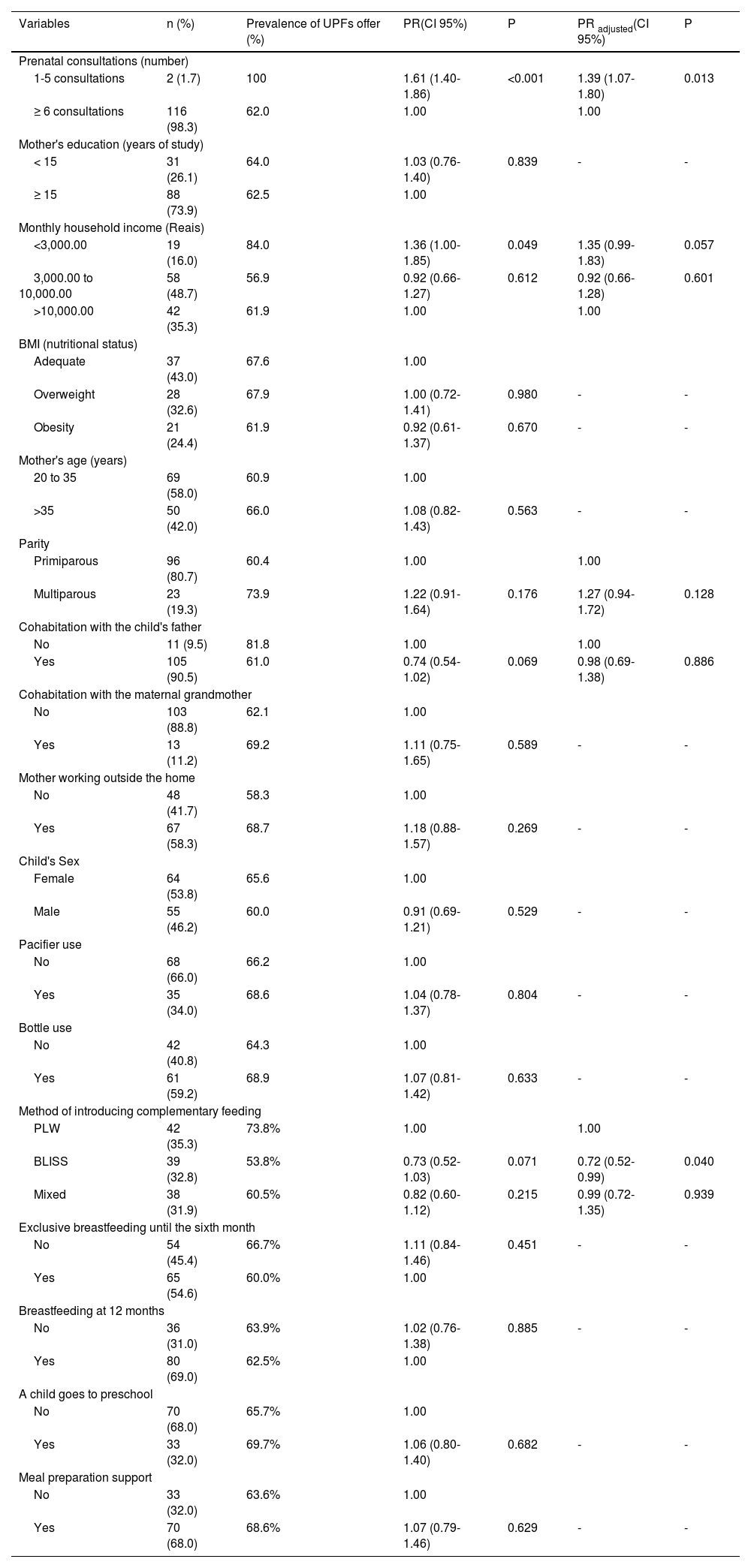
Table 2 compiles the associations between the offer of UPFs and the variables included in the previously described hierarchical model. In the univariate analysis, the number of prenatal consultations and monthly family income in the distal block was shown as possible adjustment factors; as well as living with a partner, parity, and cohabitation with the child's father in the intermediate block; and CF method in the proximal block.
Univariate and multivariate analyses of factors associated with the provision of UPFs in infants between six and twelve months of age, according to the hierarchical model.
UPFs: Ultra-processed foods; PR: Prevalence Ratio; CI: Confidence interval; BMI: Body mass index; BLISS: Baby-Led Introduction to Solids; PLW: Parent-Led Weaning.
Calculations were performed using the Poisson Regression Model. In the univariate analysis, variables were considered statistically significant when the p-value < 0.20. In the multivariate analysis, variables were considered as adjustments of the posterior block when the p-value < 0.10 and considered statistically significant when the p-value < 0.05.
Subsequently, in the multivariate analysis, a significant association was found in children who were randomized to the BLISS group (p = 0.040) and in those who received six or more prenatal consultations (p = 0.013).
DiscussionWith regard to the prevalence of UPFs offered, the result of 63% achieved in the studied sample is high, despite the mothers having received recommendations on healthy CF and the instruction not to offer UPFs. When comparing with another study carried out in Porto Alegre, researchers found that 79% of infants received some type of UPF in the 24-hour food records applied, and most of them (62.6%) had also received instructions on healthy CF from health professionals. However, the caregivers of the children in this study had lower education and income than the sample.23 Broader data, such as those from the Ministry of Health, with parents recruited from Basic Health Units in several Brazilian municipalities (n = 38.566), showed exposure to UPFs in 56% of infants.24 Other national studies also found alarming prevalence during CF, such as 86.3% in the Federal District,25 in São Paulo 43.1%,8 and 90.6% in Alagoas.7
The BLISS method showed to be a protective factor for the UPFs offered. Another study carried out in New Zealand aimed at assessing the BLISS method and nutrient intake and concluded that children following the BLISS technique consumed less saturated fat at twelve months of age compared to those spoon-fed porridge and puree.26 Although the authors did not discuss the level of food processing, it is possible that the difference in saturated fat consumption is associated with lower consumption of UPFs, because saturated fat, sodium, and sugar are ingredients present in high concentrations in UPFs.26
The cross-sectional design of this study does not assist in elucidating the mechanisms involved in this interaction;26 nevertheless, the BLISS method is considered a nutritionally viable approach, capable of guaranteeing a suitable nutritional status and providing a relationship with lighter demand to eat and greater pleasure in eating.27
The present study has shown that performing less than six prenatal consultations increased the risk of UPF offers. Considering the number of mothers in this category, the possibility of a statistical bias should be highlighted. Although, it is known that in these consultations, professionals provide healthy eating guidelines that include the consumption of minimally processed foods in pregnancy;28 therefore, mothers who consulted less could have been poorly educated on the subject.
Although in the present study the authors did not have a significantly association between schooling, age, and maternal income and the consumption of UPF, a cohort study pointed out that the consumption of these foods was higher among children with mothers with low schooling, younger and low income.29 On the other hand, national data show that individuals belonging to families with higher income, despite having a more diversified diet rich in nutrients, which included several fresh foods, had higher consumption of industrialized foods and ready meals.30 Some limitations of this study should be addressed. Since the sample was spontaneously recruited mainly from on-target social networks, it could result in mothers previously interested in healthy eating. The socio-economic profile of the families included in the study does not reflect the reality of the Brazilian population; therefore, the generalization of these results should be done with caution. Furthermore, the authors did not measure the frequency of exposure of the children to UPF the infant in the first year.
However, it is noteworthy that the present results constitute the first known publication to investigate factors associated with UPFs offered in this population.
In conclusion, the offer of UPFs was high in the first year of life, although the mothers received guidance not to offer. In addition, the BLISS method showed to be a protective factor for the offer of UPF in CF, and less than six prenatal consultations were shown to be a risk factor. Further research is needed to confirm the association between CF and UPFs, reinforcing the need for the frequency and quantity of UPFs to be quantified in researches.
This article will be submitted to publication ISSN.