To describe a historical series on the median duration of breastfeeding in a population of mothers whose children were born from the 1960s onwards, identifying factors associated with the interruption of breastfeeding in each decade.
MethodsData were analyzed from the Pró-Saúde Study, a longitudinal epidemiological investigation started in 1999 among technical and administrative employees of a university in the state of Rio de Janeiro. Breastfeeding duration was collected in two study phases: Phase 1 (1999), and phase 4 (2011–2012). Of these, those who had at least one child and reported the duration of breastfeeding for the first child were selected (n=1539). To analyze the duration of breastfeeding, survival curves were constructed using the Kaplan–Meier method and the effect of covariates on the duration of breastfeeding was estimated by Cox regression model.
ResultsIt was found that the median duration of breastfeeding was higher in the 1990s and 2000s and lower in the 1970s, compared to the 1960s. In addition, there was an association between higher income and maternal age with breastfeeding interruption, which was focused in the 1970s.
ConclusionThere was shorter duration of breastfeeding in the 1970s compared to the 1960s. Increased duration and prevalence of breastfeeding from the 1970s onwards coincided with the national trend and the promotion of this practice since 1980.
Descrever uma série histórica sobre a duração mediana da amamentação em população de mães com crianças nascidas a partir da década de 1960, identificando fatores associados à sua interrupção em cada década.
MétodosForam analisados dados de 1539 participantes do Estudo Pró-Saúde (EPS), uma investigação epidemiológica longitudinal iniciada em 1999 entre trabalhadores técnico-administrativos de uma universidade localizada no Estado do Rio de Janeiro. Foram utilizadas informações sobre duração do aleitamento materno do primeiro filho coletadas em duas fases do EPS (1999 e 2011-12). Para análise da duração do aleitamento materno foram construídas curvas de sobrevida pelo método de Kaplan–Meier, e sua associação com covariáveis foi estimada pelo modelo de regressão de Cox.
ResultadosVerificou-se que a duração mediana do aleitamento materno foi maior nas décadas de 1990 e 2000, e menor na década de 1970, em comparação com a década de 1960. Além disso, houve associação entre maior renda e faixa etária maternas com interrupção do aleitamento materno, que se concentrou na década de 1970.
ConclusãoObservou-se menor duração do aleitamento materno na década de 1970 em relação à década de 1960. O aumento da duração e das prevalências de amamentação a partir da década de 1970 coincidiu com a tendência nacional e com a promoção dessa prática a partir de 1980.
Breastfeeding is considered one of the strategies that most contributes to the prevention of child death, with the potential to save more than 800,000 children under 5 years of age per year worldwide1,2 and to reduce neonatal mortality,3 which is recommended as an exclusive practice until 6 months of age and as a supplement up to 2 years of age or older.4 In spite of its relevance, social and economic circumstances may have a profound influence on the prevalence and duration of breastfeeding.5,6
In the mid-1960s, massive marketing campaigns were started to encourage the substitution of breastmilk with infant formula without any kind of regulation, reaching mothers from all social strata, which, together with cultural changes regarding the role of breastfeeding in society and the increasing integration of women into the labor market, led to the decline of breastfeeding duration.6–9 In response to that, global pro-breastfeeding movements, especially from the end of the 1970s onwards, led to the creation a set of standards based on ethical principles to regulate the commercial promotion of products that could interfere with maternal breastfeeding.10,11
Since the beginning of the 1980s, several laws, standards, and programs have been adopted by the Ministry of Health in Brazil to promote and support breastfeeding, which are considered responsible for the consistent increase in the prevalence and median duration of breastfeeding since the end of that decade,5,6,9,10 as demonstrated by national surveys,12,13 with such increments being associated with reduced morbidity and reduction in hospitalization rates.14,15
However, a historical series is not available with regard to the median duration of breastfeeding prior to the 1980s, as the only national survey carried out in the period (1974–1975) obtained only indirect information about this practice.16 To clarify whether maternal breastfeeding duration in Brazil showed an upward, steady, or downward trend before the 1980s, it is essential to employ the data obtained from other studies that are comparable to those from subsequent periods. This study aims to describe a historical series on breastfeeding duration in children born from the 1960s onwards and to identify factors associated with its interruption in each decade.
MethodsStudy populationData from the Pro-Saúde Study (PSS), a longitudinal epidemiological investigation started in 1999 with a population of technical and administrative employees of a university in the state of Rio de Janeiro, were analyzed. The main objective of the PSS is to elucidate the role of social determinants of health; between 1999 and 2013, four data collection steps were carried out, including self-completion of questionnaires, anthropometric measurements, and other tests.
All technical and administrative staff of a university in Rio de Janeiro were invited to participate in the study (n=4030 in phase 1 and n=2933 in phase 4); only those assigned to other institutions or who were on a leave of absence for reasons not related to health were considered ineligible. Employees on sick leave were invited to participate in the study, which included home visits, when necessary. All women who had children and participated in the phase 1 and phase 4 of PSS were eligible for the study. Women who participated in the Phase 1 and Phase 4 were considered only once. Details of recruitment and the population studied can be found in another publication.17
The present study used data on breastfeeding duration related to the first child, collected in two phases of the PSS: Phase 1 (1999), and phase 4 (2011–2012). The PSS included 2160 women in its two phases, of whom 1727 had at least one child. For this study, only those who were able to report the breastfeeding duration for the first child were considered (n=1539).
Data collectionData collection was performed with the aid of field researchers, using a multidimensional, self-completed questionnaire administered at the work environment. A pilot study, tool reliability testing, and independent double entry18 were performed to ensure the quality of data. Breastfeeding duration was obtained in months, through specific questions asked to women who had at least one child, including the month and year of birth, the practice (or not) of breastfeeding, and in which month breastfeeding had been interrupted, all related the firstborn child. The dates of birth were categorized into decades from 1960 onwards.
The per capita monthly family income was obtained through the conversion of the household net income divided by the total number of people who depended on this income, and was categorized into per capita income tertiles. As income data related to two different periods were used, the income reported in phase 1 was adjusted for inflation using the National Index of Consumer Prices (Índice de Preços ao Consumidor Amplo [IPCA]), to maximize its comparability with Stage 4. Data on self-reported race/ethnicity were collected according to the categories of the Brazilian Institute of Geography and Statistics (Instituto Brasileiro de Geografia e Estatística [IBGE]): African-descendant, mixed-race, Caucasian, Asian, and Indigenous. Maternal age was related to the time they had their first child. Additionally, mothers were questioned about the type of delivery (cesarean or vaginal).
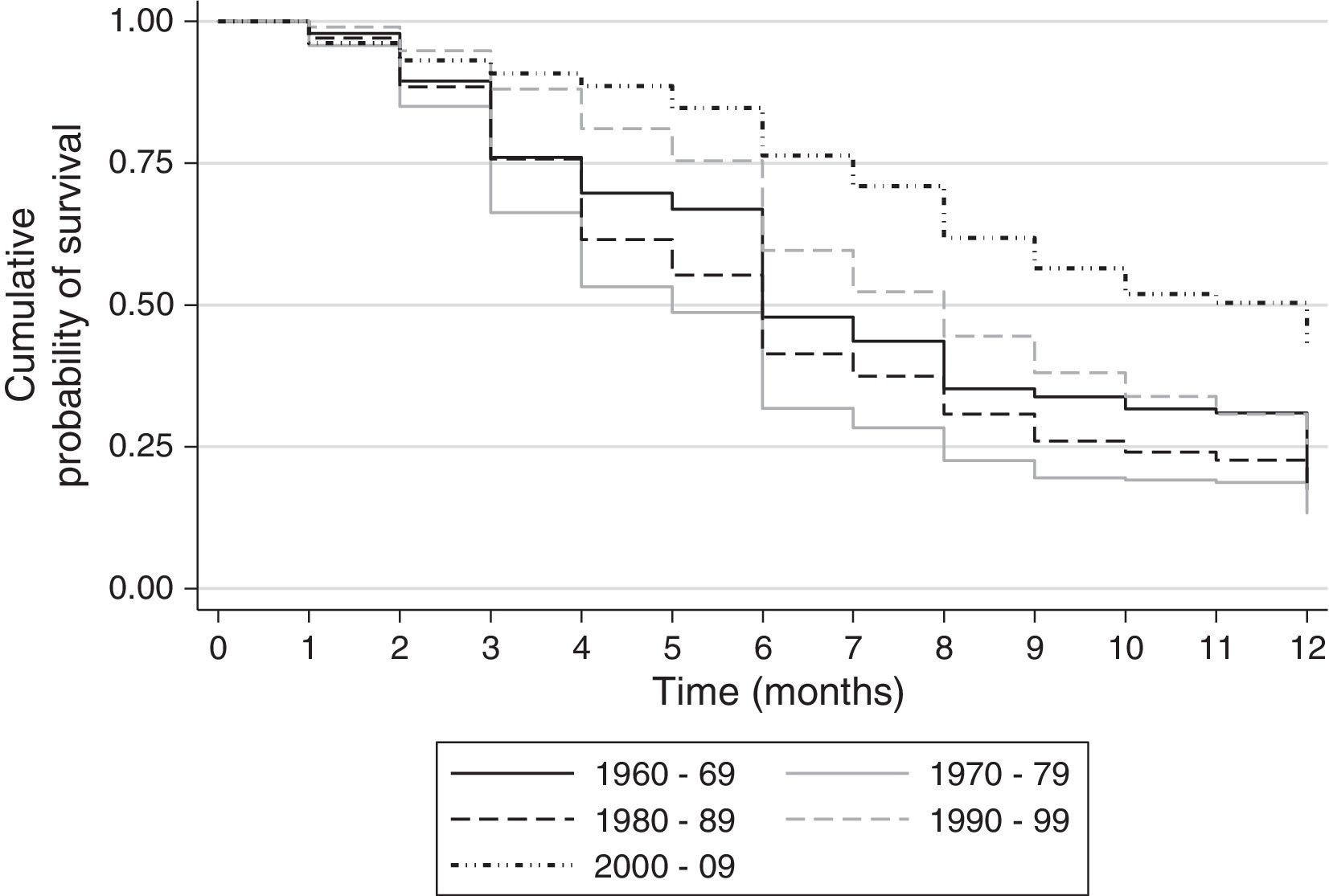
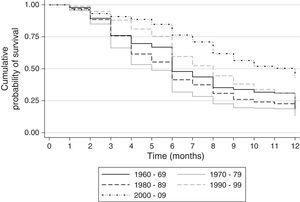
Data analysisTo analyze breastfeeding duration, survival curves were constructed using the Kaplan–Meier method for each reported decade, representing the cumulative probability of breastfeeding over the course of months. Time of breastfeeding was censored at 12 months and the association of covariates with breastfeeding duration was estimated by Cox regression.
It was decided not to include the individuals classified as Asian and Indigenous regarding skin color/ethnicity in the analysis because of their low frequencies (1.7% and 0.7%, respectively). The assumption of proportional hazards required for Cox regression was tested (including interactions of covariates with time) and by Schoenfeld residuals (1982); of the decade of birth as an independent variable was also conducted. The tested statistical significance level was 5%, and the software Stata (StataCorp. 2011. Stata Statistical Software: Release 12. College Station, USA) was used for the analysis.
Phase 1 of the PSS was approved in 1999 by the Research Ethics Committee (REC) of Hospital Universitário Pedro Ernesto (registration No. 224/1999) and phase 4 was approved in 2011 by the REC of Instituto de Medicina Social da UERJ (CAAE No. 0041.0.259.000-11).
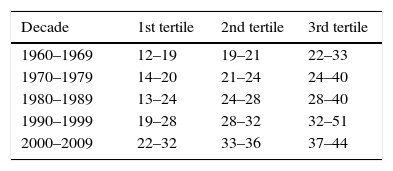
ResultsTable 1 shows the age in tertiles in each decade studied. This classification was chosen because the mothers’ mean age increased according to the first child's decade of birth.
Tertiles of mothers’ age (in years) according to decade of birth of their child. Pró-Saúde study, 1999 and 2011–2012.
| Decade | 1st tertile | 2nd tertile | 3rd tertile |
|---|---|---|---|
| 1960–1969 | 12–19 | 19–21 | 22–33 |
| 1970–1979 | 14–20 | 21–24 | 24–40 |
| 1980–1989 | 13–24 | 24–28 | 28–40 |
| 1990–1999 | 19–28 | 28–32 | 32–51 |
| 2000–2009 | 22–32 | 33–36 | 37–44 |
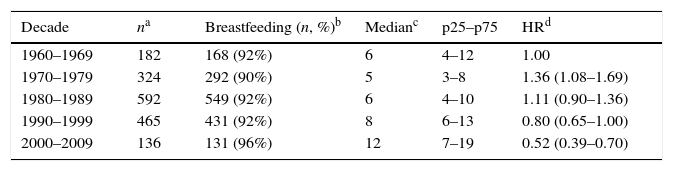
Table 2 shows the median duration of breastfeeding and the hazard ratio (HR), which expresses the risk of discontinuing breastfeeding in each decade, taking the 1960s as a reference. An increased risk of interruption in the 1970s (HR=1.36; p<0.001) and a lower risk in the 2000s (HR=0.52; p<0.001) were observed. Survival curves for breastfeeding are shown in Fig. 1, which emphasizes the lower probability of a mother to remain breastfeeding over the first 12 months of her child's life in the 1970s, and a greater increase in breastfeeding duration in the 2000–2009 period.
Distribution of women who breastfed, median duration, and risk of breastfeeding interruption in the first year of life per decade of birth of the first child. Pró-Saúde study, 1999 and 2011–2012.
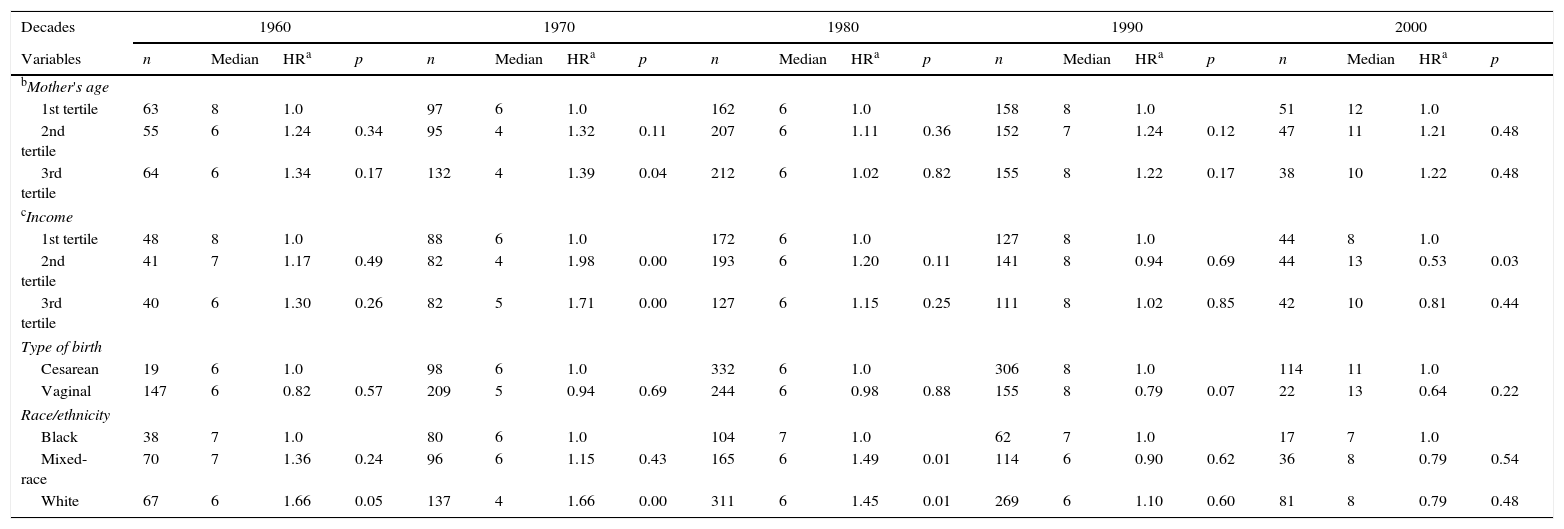
Table 3 shows the Cox model estimates for associations between covariates and time of breastfeeding for each studied decade. Statistically significant associations with the mother's income and age are concentrated in the 1970s. Older women (3rd tertile) showed a 39% higher risk of breastfeeding interruption when compared to younger ones (1st tertile). Regarding household income, participants in the second and third tertiles (higher per capita income) showed a higher risk of breastfeeding interruption in the 1970s; in the 2000s, an inverse association was observed, in which women from the second tertile of income showed lower risk. Women who self-declared their ethnicity as African descendants had a lower risk of breastfeeding interruption when compared to Caucasians in the 1960s and 1970s, as well as when compared to Caucasians and mixed-race women in the 1980s. The type of delivery was not associated with the risk of breastfeeding interruption.
Breastfeeding median duration and risk of interruption in the first year per decade of birth of the first child. Pró-Saúde study, 1999 and 2011–2012.
| Decades | 1960 | 1970 | 1980 | 1990 | 2000 | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | n | Median | HRa | p | n | Median | HRa | p | n | Median | HRa | p | n | Median | HRa | p | n | Median | HRa | p |
| bMother's age | ||||||||||||||||||||
| 1st tertile | 63 | 8 | 1.0 | 97 | 6 | 1.0 | 162 | 6 | 1.0 | 158 | 8 | 1.0 | 51 | 12 | 1.0 | |||||
| 2nd tertile | 55 | 6 | 1.24 | 0.34 | 95 | 4 | 1.32 | 0.11 | 207 | 6 | 1.11 | 0.36 | 152 | 7 | 1.24 | 0.12 | 47 | 11 | 1.21 | 0.48 |
| 3rd tertile | 64 | 6 | 1.34 | 0.17 | 132 | 4 | 1.39 | 0.04 | 212 | 6 | 1.02 | 0.82 | 155 | 8 | 1.22 | 0.17 | 38 | 10 | 1.22 | 0.48 |
| cIncome | ||||||||||||||||||||
| 1st tertile | 48 | 8 | 1.0 | 88 | 6 | 1.0 | 172 | 6 | 1.0 | 127 | 8 | 1.0 | 44 | 8 | 1.0 | |||||
| 2nd tertile | 41 | 7 | 1.17 | 0.49 | 82 | 4 | 1.98 | 0.00 | 193 | 6 | 1.20 | 0.11 | 141 | 8 | 0.94 | 0.69 | 44 | 13 | 0.53 | 0.03 |
| 3rd tertile | 40 | 6 | 1.30 | 0.26 | 82 | 5 | 1.71 | 0.00 | 127 | 6 | 1.15 | 0.25 | 111 | 8 | 1.02 | 0.85 | 42 | 10 | 0.81 | 0.44 |
| Type of birth | ||||||||||||||||||||
| Cesarean | 19 | 6 | 1.0 | 98 | 6 | 1.0 | 332 | 6 | 1.0 | 306 | 8 | 1.0 | 114 | 11 | 1.0 | |||||
| Vaginal | 147 | 6 | 0.82 | 0.57 | 209 | 5 | 0.94 | 0.69 | 244 | 6 | 0.98 | 0.88 | 155 | 8 | 0.79 | 0.07 | 22 | 13 | 0.64 | 0.22 |
| Race/ethnicity | ||||||||||||||||||||
| Black | 38 | 7 | 1.0 | 80 | 6 | 1.0 | 104 | 7 | 1.0 | 62 | 7 | 1.0 | 17 | 7 | 1.0 | |||||
| Mixed-race | 70 | 7 | 1.36 | 0.24 | 96 | 6 | 1.15 | 0.43 | 165 | 6 | 1.49 | 0.01 | 114 | 6 | 0.90 | 0.62 | 36 | 8 | 0.79 | 0.54 |
| White | 67 | 6 | 1.66 | 0.05 | 137 | 4 | 1.66 | 0.00 | 311 | 6 | 1.45 | 0.01 | 269 | 6 | 1.10 | 0.60 | 81 | 8 | 0.79 | 0.48 |
The present study investigated the evolution of breastfeeding duration between 1960 and 2009, observing an initial decline in duration in the 1970s when compared to the 1960s, and a subsequent increase in the following decades. The lowest risk of interruption was observed in the period of 2000–2009. The evolution of duration observed here cannot be compared directly to that observed in other studies assessing breastfeeding duration over the years due to the methods used for the analysis, but follows similar patterns.5,6,9,10
The National Survey on Child Mortality and Family Planning (Pesquisa Nacional de Mortalidade Infantil e Planejamento Familiar [PNMIPF])19 and the National Demographic and Health Survey (Pesquisa Nacional de Demografia e Saúde [PNDS])12 showed, respectively, a median breastfeeding duration of 9 months (1986) and 14 months (2006), a similar evolution to that observed in the National Breastfeeding Prevalence Survey (Pesquisa Nacional de Prevalência do Aleitamento Materno [PPMA]),13 conducted in the Brazilian capital cities in 1999 (9.8 months) and 2008 (11.3 months). In São Paulo, a hospital-based study with information related to the years 1954–1985 showed that the median breastfeeding duration was approximately 150 days in the 1960s and 100 days in the 1970s, with subsequent increase to over 100 days in the next decade.6
The shortest breastfeeding duration was observed in the 1970s when compared to the previous decade, which may be associated with distinct and complex sociocultural determinants, such as the increasing participation of women in the labor market and the changes in paradigms regarding the nature of breastfeeding,8 constructs that are difficult to measure with the available data from the studies. However, it is a consensus among the authors who have studied this period that this decline coincides with the peak of marketing and commercialization practices that occurred without regulation by the food industry in Brazil and worldwide during this period, as well as the cooptation of health professionals who encouraged the use of infant formula, the so-called “breastmilk substitute.”7–9,13,20 It is noteworthy that the decline in breastfeeding duration in the developed countries had occurred a previous period (1930s), with breastfeeding practice also being re-established after the 1970s.21
In the international context, breastfeeding prevalence and duration is lower in developed countries, and yet, the prevalence of exclusive breastfeeding is 37% in developing countries, with large disparities between the poorer and the richer mothers.1 In this unfavorable scenario for breastfeeding, Rolins et al. carried out a case study published in the Lancet Breastfeeding Series, which concludes that Brazil is one of the success stories in improving breastfeeding patterns due to the involvement of civil society, as well as the government's strong support and investment regarding the adoption of practices such as the international code monitoring, implementation of paid maternity leave, the creation of a human milk bank network, and child-friendly hospitals.22
When analyzing the factors associated with the risk of breastfeeding interruption, maternal income and age were highlighted. Older mothers showed greater risk of breastfeeding interruption when compared to younger ones. Similarly, mothers in the higher income stratum had a higher risk of breastfeeding interruption when compared to lower-income ones, a pattern similar to that found in different groups and countries from all regions: when analyzing 98 studies carried out in developing countries, Victora et al. found that, regardless of the country and region of the world, mothers belonging to the poorest strata breastfed for longer periods than those from the richest strata.1 Interestingly, these differences were concentrated in the 1970s, the same period when shorter breastfeeding duration was observed. The higher income favored weaning by allowing the purchase of artificial formula,14 in a context of important influence by the industry and deconstruction of natural breastfeeding benefits.20 However, there was a noteworthy reversal in the association between income and breastfeeding interruption observed in the 2000s, in which mothers with the highest income had lower risk of weaning (although it was statistically significant only for the intermediate stratum). This change can be understood as a reflection of the change in the mothers’ perception regarding the importance of breastfeeding, the result of the efforts of pro-breastfeeding movements, and the legislation that regulated the advertising of artificial formula.9,14
In fact, national survey data (1975/1989)14 had already signaled this trend. The association between breastfeeding duration and income showed to be inversely associated in 1975, being four-fold higher in children of lower income when compared to those of higher income. In 1989, this difference decreased to less than two-fold and was no longer an inversely linear association, considering all income strata. Moreover, this phenomenon was also identified in 66 countries studied since the 1990s, in which women from the poorest quintiles breastfed longer than women from the richest quintiles.22
Regarding skin color/ethnicity, the present study disclosed shorter median breastfeeding duration among Caucasian mothers when compared to African descendants. There may be cultural influences on infant feeding patterns in different ethnic groups; however, there is little evidence about how such patterns have been modified, and whether they have been influenced by public policies remains unknown.23
Some limitations of this study should be emphasized. First, data on household income are related to the time of the interview and not of the child's birth; however, such income was categorized in relative terms (tertiles) and it is possible that these positions have remained stable.
Second, the smaller sample size in the 1960s and 2000s reduced the statistical power to detect differences between the variables in these periods; it should be noted, however, that the sample size was larger in the 1980s and 1990s, but statistically significant differences were not observed in these periods in relation to breastfeeding. As for possible recall bias, a test–retest study of the self-reported duration of breastfeeding was carried out in a subpopulation of women followed since 1999 in the PSS; the short-term (14 days) and long-term (13 years) reliability was considered adequate, indicating that the recall bias may not be important in the study (Robaina et al., in press). The external validity can be questioned, but the similarity with the evolution of breastfeeding patterns observed at the national level allows for raising hypotheses about the evolution of breastfeeding since the 1960s.
The results of this study disclosed the dynamics of breastfeeding duration evolution over the decades, with a shorter duration in the 1970s when compared to the previous decade and a subsequent increase in duration in the following decades. Moreover, more noteworthy individual differences were observed among the population of mothers in the 1970s. The resulting increase in breastfeeding duration in the following decades suggests that the adoption of policies, standards, and practices for the promotion, protection and, support of maternal breastfeeding, adopted from the 1980s onward, were favorable to this practice.
FundingState of Rio de Janeiro Research Foundation (n. E-26/010.001796/2015), Brazilian National Research Council (n. 484636/2013-8).
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Oliveira DS, Boccolini CS, Faerstein E, Verly-Jr E. Breastfeeding duration and associated factors between 1960 and 2000. J Pediatr (Rio J). 2017;93:130–5.
Study conducted at Universidade do Estado do Rio de Janeiro (UERJ), Rio de Janeiro, RJ, Brazil.