To develop growth charts for weight-for-age, height-for-age, and body mass index (BMI)-for-age for both genders aged 2 to 18 years for Brazilian patients with Williams-Beuren Syndrome (WBS).
MethodsThis is a multicenter, retrospective, and longitudinal study, data were collected from the medical records of boys and girls with a confirmed diagnosis of WBS in three large university centers in the state of Sao Paulo, Brazil. Growth charts stratified by gender and age in years were developed using LMSchartmaker Pro software. The LMS (Lambda Mu Sigma) method was used to model the charts . The quality of the settings was checked by worm plots.
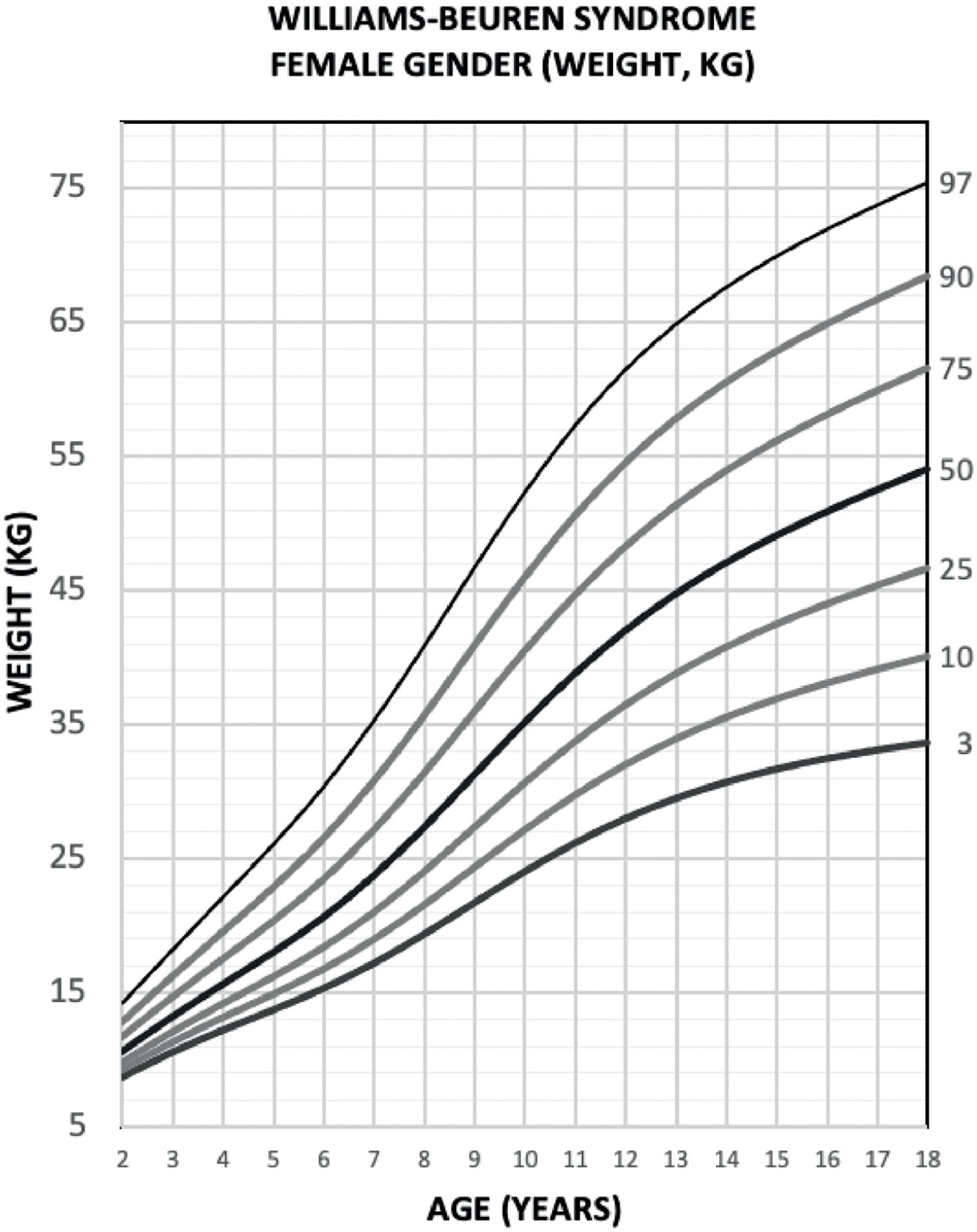
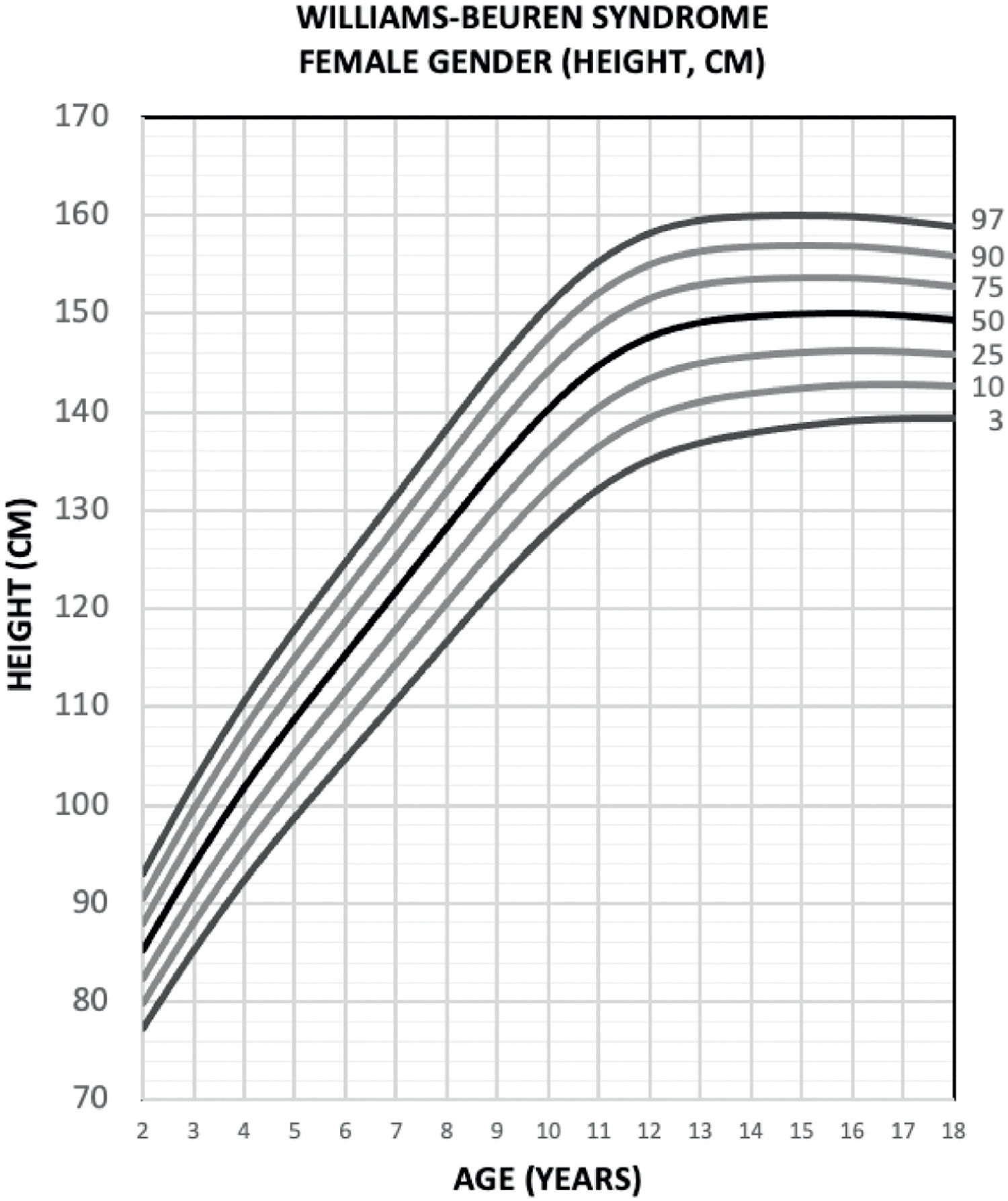
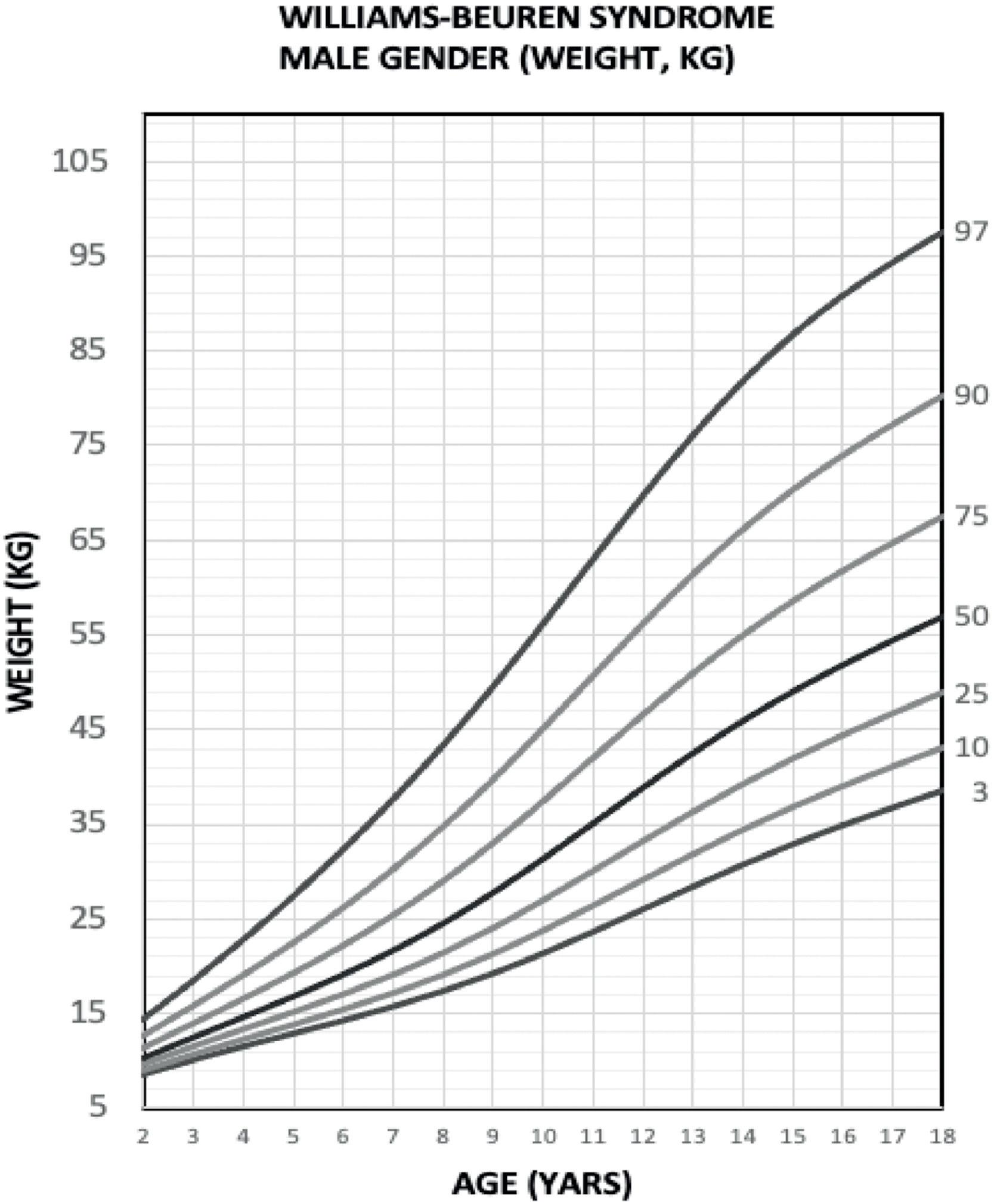
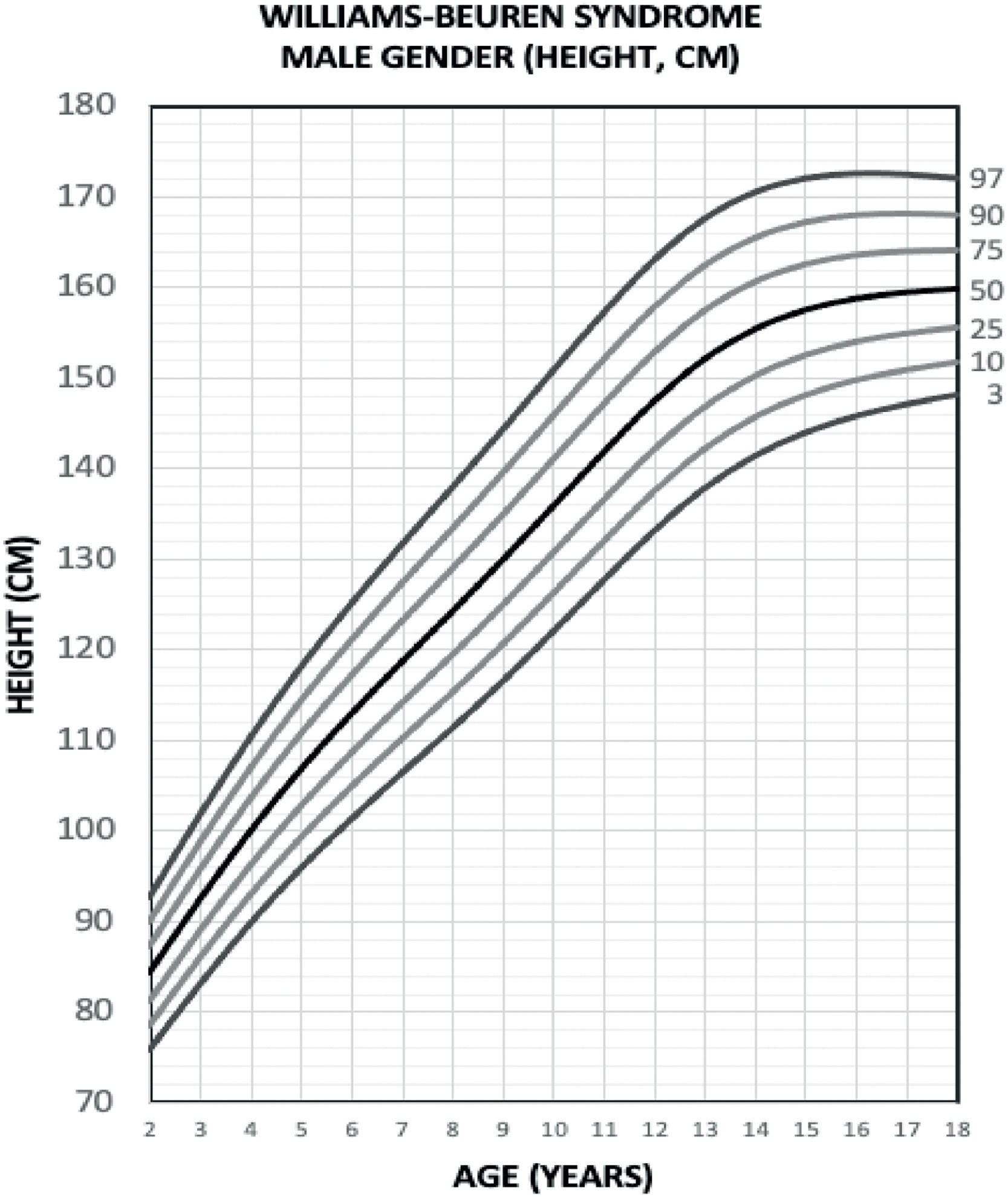
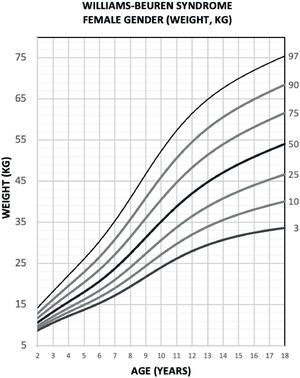
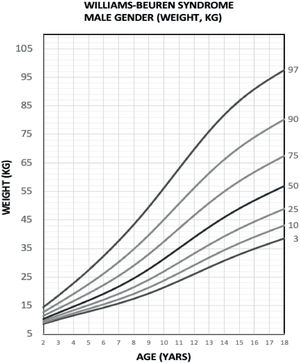
ResultsThe first Brazilian growth charts for weight-for-age, height-for-age, and BMI-for-age stratified by gender were constructed for WBS patients aged 2 to 18 years.
ConclusionThe growth charts developed in this study can help to guide family members and to improve the health care offered by health professionals.
Williams-Beuren syndrome (WBS) (OMIM#194050) 1 is a rare genetic disorder with an incidence of around 1:7,500 to 1:10,000 live births.2,3 It was first described in 1961 by the New Zealand study led by Williams et al.,4 and in 1962, in Germany, Beuren et al.5 independently described the same syndrome. The most frequent clinical features in WBS are typical facies; 2,3 heart disease (supravalvular aortic stenosis is the most frequent); 2,3 short stature; 6,7 endocrine disorders (idiopathic hypercalcemia,2,6 subclinical hypothyroidism 2,6 and early puberty,2,7 but not precocious, are the most frequent); mental disability; 2,3 and a highly sociable behavior.2 In 1993, a study by Ewart et al.8 identified that the genetic alterations that determine WBS are microdeletion of 1.5-1.8 million base pairs and the loss of one of the copies of 26 to 28 contiguous genes in the chromosomal region at 7q11.23.8 WBS can be inherited; however, it most often occurs de novo, with no predilection for gender or ethnicity.6 In general, the diagnosis is late 6,9 and the symptoms that usually trigger investigation are typical facies, heart disease, and hypercalcemia, although growth retardation is the earliest symptom.9 The tests currently used to confirm WBS are FISH (fluorescence in situ hybridization), MLPA (multiplex-ligating probe amplification), CMA (chromosomal microarray analysis), and microsatellite DNA markers.2
Regarding growth, several studies have already shown that WBS patients have a typical growth profile that is different from the growth patterns used as reference 6,10 and it is characterized by intrauterine growth restriction,9,10, low weight, length, and head circumference (HC) at birth,6,9 followed by global growth retardation in height in childhood and adolescence, determining final height below the average of the reference population.7,10,11 In 1988, Morris et al.12 published one of the first studies that evaluated the growth of WBS patients with only a clinical diagnosis; later, in 2007, the Martin et al. study 13 developed the British growth charts stratified by gender and age for WBS using the LMS (Lambda Mu Sigma) method and it was the first study to include only patients with molecular diagnostic confirmation.13 Martin et al.13 compared their study with the study by Morris et al.12 and observed that average final heights for adult men and women with WBS were similar in both studies and were on average 18 and 12 cm shorter than reference adult men and women.12,13
In pediatrics, growth correlates well with the health prognosis of children and, therefore, it is widely used as a health surveillance tool.9,14 Growth charts using weight, height, head circumference, and body mass index (BMI) are the most commonly used instruments for this purpose because they are easy to use, low cost, and highly accurate.14 However, these charts were constructed using growth data from reference populations not carrying specific genetic syndromes or clinical conditions.14,15 In many situations, patients do not have the same growth profile as the reference population and often have their growth underestimated as is the case with WBS.10,16-18 Correct growth assessment allows for the early detection of deviations in the growth pattern, enabling the best intervention in reversible or non-reversible pathological conditions that may affect the overall development of children and adolescents.15 CDC (Centers for Disease Control and Prevention) and WHO (World Health Organization) indicate there is a need for the development of specific growth charts to track populations with clinical conditions that deviate from the growth pattern currently used.14 The WHO growth charts,15 currently taken as a reference, are not compatible with the expected growth targets for the WBS population. Thus, it is necessary to construct growth charts for WBS patients in order to improve the assistance to this population.3,10,13 The aim of this study was to construct female and male charts of weight-for-age, height-for-age, and BMI-for-age for WBS patients in the age range of 2 to 18 years.
Casuistic and methodsThe study was conducted according to the ethical principles of the Declaration of Helsinki and theolution no. 466/12 of the Brazilian National Health Council, and it was approved by the State University of Campinas (UNICAMP) Human Research Ethics Committee (CAAE: 42981421.0.0000.5404) and it was also authorized by the heads of each Service of each Institution.
CasuisticThis is a multicenter, retrospective, and longitudinal study. The data were collected by reviewing medical records from the Clinics Genetics Service of the Clinical Hospital of the School of Medical Sciences of the State University of Campinas (UNICAMP), Campinas, Sao Paulo, Brazil; from the Outpatient Clinic of the Genetics Unit of the Institute of Child Health of Clinical Hospital of the School of Medicine of the University of Sao Paulo (USP), Sao Paulo, Sao Paulo, Brazil; and from the Genetic Counseling Service of the Genetics Department of the Biosciences Institute of the State University of Sao Paulo (UNESP), Botucatu, Sao Paulo, Brazil.
All patients aged 0 to 20 years with a diagnosis of WBS with laboratory confirmation by at least one of the following methods were included: FISH and/or MLPA and/or CMA and/or microsatellite markers.
It was excluded: 1. data where it was not possible to retrieve the age at the time of evaluation; 2. duplicate data for having been seen at different institutions or at the same institution with a time difference of less than one month for the calculation of the measures from 0 to 23 months, and less than 12 months for the calculation of the measures from 2 to 20 years; 3. data between 0 and 2 years in which the individual had a history of prematurity or in which the history of prematurity could not be recovered; 4. data from individuals with untreated hypothyroidism, or whose treatment information was not available; 5. data from individuals with other hormonal disorders or treatments that could interfere with growth (precocious puberty, growth hormone use, chronic corticotherapy); 6. data from individuals with other non-hormonal disorders that could interfere with growth; 7. data from individuals with congenital heart disease and requiring treatment who were not treated, or whose treatment information was not available; 8. data from individuals who were recorded as having lost height with advancing age; 9. anthropometric data with more than five standard deviations (plus or minus) for age and gender.
Data collectionThe data collected was: 1. gender (male or female); 2. date of birth and date of consultation, with subsequent calculation of age at consultation in years and months; 3. weight (kg); 4. height (cm); 5. head circumference (cm). BMI (kg/m2) was calculated from the data collected on weight and height. A data collection form was prepared to include the serial data mentioned above and to fill in the other relevant data for the research: test or tetestsperformed to confirm WBS, history of prematurity, birth data, hypothyroidism, congenital heart disease, other diseases, and drugs of continuous use.
Statistical analysisGrowth charts stratified by gender and age in years were developed using LMSchartmaker Pro software. The LMS (Lambda Mu Sigma) method was used to model the charts.19 The fitting quality was checked by worm plots.20 The 3rd, 10th, 25th, 50th, 75th, 90th, and 97th percentiles were generated to construct the weight-for-age, height-for-age, and BMI-for-age charts.
ResultsFrom October 2021 to May 2022, 341 medical records were analyzed. Then, 302 patients were included, and 6,809 growth measurements were collected (weight: 3,465; height: 3,344). In the next step, exclusion criteria 1 to 8 were applied, with subsequent preliminary statistical analysis. At this stage, 3,660 growth measurements (weight: 1,876; height: 1,784) and 29 patients were excluded. 3,149 growth measurements (weight: 1,589; height: 1,560) and 273 patients remained for preliminary statistical analysis. After preliminary statistical analysis, data were removed by criterion 9 and the construction of growth charts for the age group 2 to 18 years was defined, since there was not enough data in the age groups from 0 to 23 months and from 19 to 20 years that would allow building accurate growth charts. Thus, birth data, data from 1 to 23 months, and data from 19 to 20 years were also excluded. At this stage, 788 growth measurements (weight: 405 measurements; height: 383) and 28 patients were excluded (Supplement – Table 1).
Finally, 2,361 anthropometric measurements (weight = 1,184 measurements; height = 1,177 measurements) and 245 patients born from 1981 to 2015 remained for the construction of the charts. Out of 245 participants, 112 were female (provided a minimum of 1 and a maximum of 16 measurements per participant) and 133 were male (provided a minimum of 1 and a maximum of 17 measurements per participant) (Supplement – Table 2).
In the evaluation of comorbidities, the most prevalent alterations were neuropsychiatric disorders in which all participants presented some cognitive alteration, followed by cardiovascular diseases (176/245; 71.8%), with congenital heart diseases being the most frequent (166/245; 67.7%), and among them the most frequent was supra valvular aortic stenosis either isolated or associated (72/245; 29.4%). Changes in the gastrointestinal tract were present in 48.2% of cases (118/245), with constipation (62/245; 25.3%) and gastroesophageal reflux (48/245; 19.6%) being the most frequent ones. Hypothyroidism and hypercalcemia were present in 10.6% (26/245) and 3.7% (9/245) of cases, respectively (Supplement – Tables 3 and 4).
Weight-for-age, height-for-age, and BMI-for-age growth charts for boys and girls aged 2 to 18 years were constructed according to the proposed statistical modeling. Weight-for-age and height-for-age growth charts for boys and girls are presented in Figs. 1-4 (BMI-for-age growth charts for boys and girls are presented in the supplement section – Figures 5 and 6). The quality of the settings was checked, and statistical diagnoses were performed with the Q-statistic and worm plots method, and they comply with the references (Q-statistic between + 2 and - 2 and linear worm plots), therefore free of bias (Supplement – Tables 5 – 10).
DiscussionThis study constructed the first weight, height, and BMI charts stratified by gender and age from 2 to 18 years for the Brazilian population with WBS. The participant selection process and the strict exclusion criteria contributed to constructing charts that represent a growth profile more suitable for the usual health profile of this population and it was compatible with current literature data.2,3,10 The average final height for girls was 149 cm, 3 cm less than the average female final height published in the study by Martin et al.13 – which was 152 cm – and 14 cm less than the average WHO reference female population 15 – which was 163 cm. The average final height for boys was 159 cm, the same as the average male final height published in the study by Martin et al.13 and 17 cm less than the average WHO reference male population 15 – which was 176 cm.
The mechanisms that determine this growth pattern are still unclear. Many authors argue that it is related to the intrinsic changes of the microdeletion, the multisystemic changes secondary to it, and the pattern of pubertal development, which is typical of these patients.2,6,10 The highest proportion of loss of height occurs in early childhood, markedly up to the age of 4, when the growth rate is lower.7,11,21
Gastrointestinal symptoms such as gastroesophageal reflux, recurrent cramps, constipation, and vomiting are the conditions most often related to difficulty in gaining weight in the first years of life, probably because they lead to insufficient caloric intake.7,11,21
The assessment of the role of heart disease on growth has been limited in the studies and does not seem to be a determining factor in growth impairment.2,10,21 In the study by Pankau et al.,21 no significant difference was observed in the growth of WBS individuals with and without heart disease, and there was no catch-up in the group of patients with treated heart disease.21
Regarding endocrine changes, the typical pubertal development pattern characterized by early (but not precocious) puberty and a shortened pubertal growth spurt by an average of one year also contribute to the final height deficit.6,7 Thyroid dysfunctions, meanwhile, do not seem to play a significant role in growth impairment, subclinical hypothyroidism is the most prevalent form (15-30%) and it generally occurs in early childhood, in most cases presenting with TSH levels lower than 10 mIU/L and requiring no treatment.6
The present work has limitations in obtaining data from medical records, and therefore rigorous data processing was performed to minimize such effect. The sample was restricted to three large teaching, research, and care centers in the state of São Paulo, which, although comprising a substantial and diverse population, does not represent the total population of children and adolescents with WBS in Brazil. In the age group from 0 to 23 months, it is recommended to draw time-interval charts in months, the shortage of data possibly occurred due to the rarity of the disease and the late diagnosis that leads to specialized follow-ups starting after the infant period. In the case of data from 19 to 20 years old, the lack of data was possibly due to loss of follow-up caused by stabilization of the condition, reinforcing the need to expand this study in order to include these age groups.
However, this work presents the Brazilian growth charts for WBS patients aged 2 to 18 years. In Brazil, the authors still do not have official health protocols to guide health professionals in the assistance to WBS patients, thus, the developed charts are important tools and can contribute to improving the attention to this population,3,6 as it is done in other countries, and resulting in good outcomes.3 The use of growth charts for WBS patients promotes more assertive treatment by adjusting it to the expected growth targets for this population. By doing so, they can reduce unnecessary investigations, or the delay in investigating growth deviations, improving the health care and quality of life of these patients.3
In conclusion, this study presents the first Brazilian growth charts from 2 to 18 years for WBS patients, and it is the first Brazilian reference of weight-for-age, height-for-age, and BMI-for-age for WBS boys and girls from 2 to 18 years. It is expected that these charts can guide parents and improve the assistance provided by health professionals in the caretaking of children and adolescents with WBS.