To investigate, at school age, the metabolic profile of children born preterm.
MethodsA cross-sectional study of children 5 to 8 years old, born with gestational age (GA) < 34 weeks and/or weight ≤ 1,500 grams. Clinical and anthropometric data were assessed by a single trained pediatrician. Biochemical measurements were done at the organization's Central Laboratory using standard methods. Data on health conditions, eating, and daily life habits were retrieved from medical charts and through validated questionnaires. Binary logistic and linear regression models were built to identify the association between variables, weight excess, and GA.
ResultsOut of 60 children (53.3% female), 6.8 ± 0.7 years old, 16.6% presented excess weight, 13.3% showed increased insulin resistance markers and 36.7% had abnormal blood pressure values. Those presenting excess weight had higher waist circumferences and higher HOMA-IR than normal-weight children (OR = 1.64; CI = 1.035–2.949). Eating and daily life habits were not different among overweight and normal-weight children. The small-for-gestational-age (SGA) and appropriate-for-gestational-age (AGA, 83.3%) birth weight children did not differ regarding clinical (body weight, blood pressure) or biochemical variables (serum lipids, blood glucose, HOMA-IR).
ConclusionSchoolchildren born preterm, regardless of being AGA or SGA, were overweight, and presented increased abdominal adiposity, reduced insulin sensitivity, and altered lipid profile, justifying longitudinal follow-up regarding adverse metabolic outcomes in the future.
Pre and perinatal conditions are associated with an increased risk of developing metabolic syndrome and cardiometabolic disorders later in life. Adverse metabolic outcomes have been reported among children or young adults born preterm infants.1 Adults who were born prematurely may present elevated blood pressure, abnormalities in glucose tolerance profiles, higher total body fat mass, and increased risk for obesity in comparison with the ones who were born after a full-term pregnancy.2 Low birth weight is a consequence of either a compromised environment during intrauterine life or preterm interruption of gestation. An imbalance in intrauterine conditions would trigger an adaptive process aiming at survival in the short term, which may have deleterious impacts in the future. Preterm infants face an adverse postnatal environment. The body composition of infants has been associated with diseases later in life. Males born preterm presented with decreased body fat and fat-free mass in childhood but higher fat mass in adulthood than those born full-term.3 In a large national cohort, persons born preterm had increased risks of new-onset heart failure from childhood into adulthood, and gestational age (GA) at birth was inversely associated with the heart failure risk4. In addition, low birth weight in born preterm children presented an increased risk of cardiometabolic disorders in childhood and adulthood, including insulin resistance and increased blood pressure5. However, there is still controversy regarding identifying markers of metabolic disorders at school age in children born preterm,2 and this knowledge is essential for adopting preventive measures. Therefore, we aimed to investigate the metabolic profile of children between 5 and 8 years old, born preterm, to contribute to this subject.
MethodsA cross-sectional study was conducted with children aged between 5 and 8 years, born with a GA < 34 weeks and/or weighing less than 1500 g, followed up at ACRIAR, an outpatient clinic for risk children of a university hospital (Hospital das Clínicas da Universidade Federal de Minas Gerais – HC-UFMG). The study was approved by the Research Ethics Committee of the Institution (CAAE 65937717.2.0000.5149) and children whenever possible, and their legal guardians signed the informed written consent. All the patients came from the neonatal unit of the HC- UFMG, which is a child-friendly hospital. The neonatal unit has Neonatal Intensive Care Unit, Neonatal Semi-Intensive Care Unit, and Kangaroo Care Unit. There is free access for the parents of hospitalized preterm infants. After hospital discharge, children born weighing less than 1500 g and/or GA less than 34 weeks are followed up until school age by a multidisciplinary team at ACRIAR, where 800 consultations are carried out per year, and 60 new cases annually. All children monitored at ACRIAR in 2017 and 2018, who met the age criteria, were eligible for the study and were contacted by phone or mail and invited to participate.
All patients who agreed to participate underwent clinical evaluation by the same examiner, with emphasis on life habits, current health conditions, and anthropometry. Children presenting malformations, genetic syndromes, or cerebral palsy were not included. A final sample consisted of 60 children (see sample selection flowchart in supplement 1).
Brazilian Food and Nutrition Surveillance System (Sisvan) guideddiet recall.6 The anthropometric parameters were assessed according to the World Health Organization (WHO) criteria,7 using a digital platform scale to the nearest 0.1 kg for weight, and a wall-mounted stadiometer to the nearest 0.1 cm for height.
For evaluation of anthropometric measurements at birth, the Fenton curve was used to classify children as SGA (Small for Gestational Age), AGA (Appropriate for Gestational Age), or LGA (Large for Gestational Age).8 Growth up to the age of two years and at school age was monitored by the Intergrowth 219 program and the World Health Organization - WHO Anthro Plus program (weight and height for age),10 respectively. The Z score for body mass index (BMI) was classified according to the WHO criteria.7
Waist circumference was measured at the midpoint between the last rib and the anterosuperior iliac crest, after a normal expiration, using a non-extendable measuring tape. The waist-to-height ratio was calculated and analyzed according to parameters for age and sex, defined for Brazilian children.11 The pubertal stage was evaluated using the Tanner criteria.12
Systemic blood pressure was measured in the supine position, using an aneroid sphygmomanometer with an appropriate cuff for each patient, and analyzed according to the Pediatric Hypertension Guidelines updated from The Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescent.13
After an 8-hour fast, blood samples were collected between 7 a.m. and 9 a.m. for biochemical evaluation and processed at the Central Laboratory of HC-UFMG. Total cholesterol and fractions (LDL-C, HDL-C, VLDL-C) in addition to triglyceride levels were measured by colorimetric method and analyzed according to the recommendations of the Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents, 2012.14 Fasting glucose and insulin were evaluated by colorimetric and chemiluminescence methods, respectively. Blood glucose was evaluated according to the guidelines of the Brazilian Society of Diabetes 2017–2018.15 The Homeostatic Model Assessment Insulin Resistance Index (HOMA-IR) was calculated to assess insulin resistance with a reference value ≤ 2.5.16
Clinical data at birth were retrieved from medical charts.
Statistical analysisThe absolute and relative frequencies for qualitative variables and mean ± standard deviation (SD) for quantitative variables are presented. The Shapiro-Wilk test was applied to assess the normality of the distribution of quantitative variables. The association between categorical variables was assessed using Fisher's and chi-square tests of independence. Student´s or Wilcoxon Mann-Whitney tests were used to compare independent samples, and Spearman or Pearson correlation coefficients to verify the association between quantitative variables.
Linear and binary logistic regression models were built to identify associations between excess weight and clinical data, IG (weeks), AIG, PIG, and biochemical data (TGL, VLDL-C, HOMA-IR).
The analyses were performed using the free software R, version 3.4.3, with a significance level of 5%.
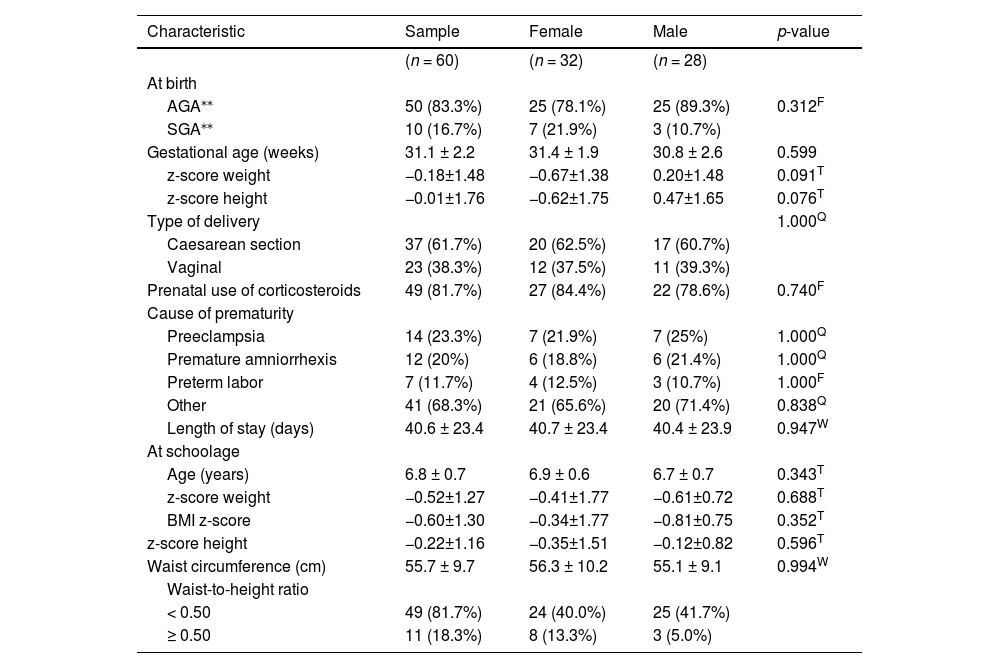
ResultsThe sample consisted of 60 children (53.3% female), aged 6.8 ± 0.7 years, and with similar low socioeconomic levels. There was no significant difference between males and females in terms of both birth and current characteristics, and therefore the sample was evaluated together. The subjects’ clinical features are summarized in Tables 1 and 2.
Clinical characteristics of 60 schoolchildren born preterm and followed-up at an outpatient clinic for children at risk (ACRIAR/UFMG) from June 2017 to July 2018.
| Characteristic | Sample | Female | Male | p-value |
|---|---|---|---|---|
| (n = 60) | (n = 32) | (n = 28) | ||
| At birth | ||||
| AGA⁎⁎ | 50 (83.3%) | 25 (78.1%) | 25 (89.3%) | 0.312F |
| SGA⁎⁎ | 10 (16.7%) | 7 (21.9%) | 3 (10.7%) | |
| Gestational age (weeks) | 31.1 ± 2.2 | 31.4 ± 1.9 | 30.8 ± 2.6 | 0.599 |
| z-score weight | −0.18±1.48 | −0.67±1.38 | 0.20±1.48 | 0.091T |
| z-score height | −0.01±1.76 | −0.62±1.75 | 0.47±1.65 | 0.076T |
| Type of delivery | 1.000Q | |||
| Caesarean section | 37 (61.7%) | 20 (62.5%) | 17 (60.7%) | |
| Vaginal | 23 (38.3%) | 12 (37.5%) | 11 (39.3%) | |
| Prenatal use of corticosteroids | 49 (81.7%) | 27 (84.4%) | 22 (78.6%) | 0.740F |
| Cause of prematurity | ||||
| Preeclampsia | 14 (23.3%) | 7 (21.9%) | 7 (25%) | 1.000Q |
| Premature amniorrhexis | 12 (20%) | 6 (18.8%) | 6 (21.4%) | 1.000Q |
| Preterm labor | 7 (11.7%) | 4 (12.5%) | 3 (10.7%) | 1.000F |
| Other | 41 (68.3%) | 21 (65.6%) | 20 (71.4%) | 0.838Q |
| Length of stay (days) | 40.6 ± 23.4 | 40.7 ± 23.4 | 40.4 ± 23.9 | 0.947W |
| At schoolage | ||||
| Age (years) | 6.8 ± 0.7 | 6.9 ± 0.6 | 6.7 ± 0.7 | 0.343T |
| z-score weight | −0.52±1.27 | −0.41±1.77 | −0.61±0.72 | 0.688T |
| BMI z-score | −0.60±1.30 | −0.34±1.77 | −0.81±0.75 | 0.352T |
| z-score height | −0.22±1.16 | −0.35±1.51 | −0.12±0.82 | 0.596T |
| Waist circumference (cm) | 55.7 ± 9.7 | 56.3 ± 10.2 | 55.1 ± 9.1 | 0.994W |
| Waist-to-height ratio | ||||
| < 0.50 | 49 (81.7%) | 24 (40.0%) | 25 (41.7%) | |
| ≥ 0.50 | 11 (18.3%) | 8 (13.3%) | 3 (5.0%) |
*Variables expressed as mean±SD and n = sample size.
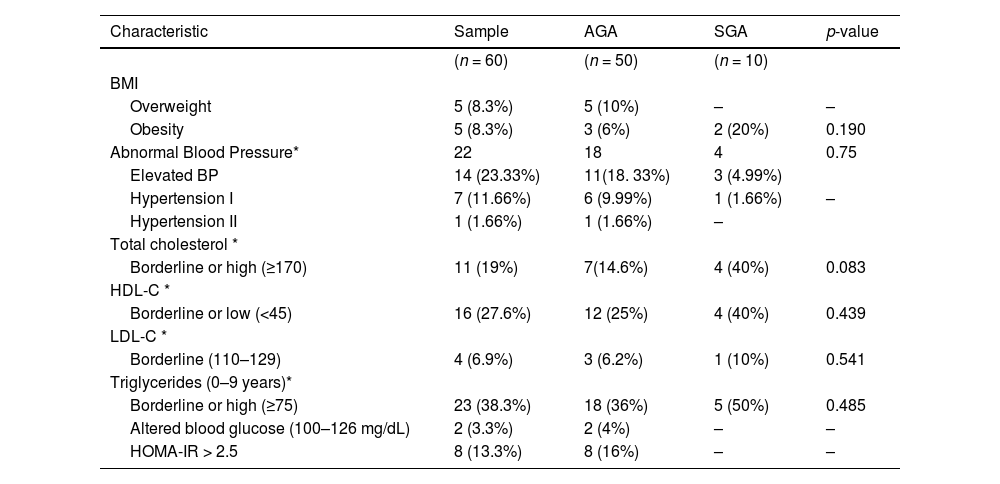
Clinical and biochemical characteristics of 60 schoolchildren born preterm and followed-up at the outpatient clinic for children at risk (ACRIAR/UFMG) from June 2017 to July 2018, according to Fenton's classification.
| Characteristic | Sample | AGA | SGA | p-value |
|---|---|---|---|---|
| (n = 60) | (n = 50) | (n = 10) | ||
| BMI | ||||
| Overweight | 5 (8.3%) | 5 (10%) | – | – |
| Obesity | 5 (8.3%) | 3 (6%) | 2 (20%) | 0.190 |
| Abnormal Blood Pressure* | 22 | 18 | 4 | 0.75 |
| Elevated BP | 14 (23.33%) | 11(18. 33%) | 3 (4.99%) | |
| Hypertension I | 7 (11.66%) | 6 (9.99%) | 1 (1.66%) | – |
| Hypertension II | 1 (1.66%) | 1 (1.66%) | – | |
| Total cholesterol * | ||||
| Borderline or high (≥170) | 11 (19%) | 7(14.6%) | 4 (40%) | 0.083 |
| HDL-C * | ||||
| Borderline or low (<45) | 16 (27.6%) | 12 (25%) | 4 (40%) | 0.439 |
| LDL-C * | ||||
| Borderline (110–129) | 4 (6.9%) | 3 (6.2%) | 1 (10%) | 0.541 |
| Triglycerides (0–9 years)* | ||||
| Borderline or high (≥75) | 23 (38.3%) | 18 (36%) | 5 (50%) | 0.485 |
| Altered blood glucose (100–126 mg/dL) | 2 (3.3%) | 2 (4%) | – | – |
| HOMA-IR > 2.5 | 8 (13.3%) | 8 (16%) | – | – |
Total cholesterol and fractions and Triglycerides: mg/dL.
Ten children (16.6%), two classified as SGA at birth, had excess weight; 8.3% were overweight and 8.3% were obese (Table 2). Ten children (16.6%) had a waist circumference above the expected limit, and seven were overweight. Three of eleven children (one SGA) with a waist-to-height ratio above the expected limit had an adequate BMI.
Twenty-two children (36.7%) were classified in one of the abnormal BP categories (Table 2), five were overweight, and three were SGA at birth. There is neither evidence of an association between abnormal BP and overweight (p = 0.34) nor to having born SGA (p = 0.75).
At the time of evaluation, no child had started puberty, and only one girl had isolated pubarche.
The mean duration of exclusive breastfeeding was 2.3 ± 2.6 months, and it did not differ between children with an appropriate BMI for their age (2.44 ± 2.55 months) and those overweight (2.24 ± 2.64 months; p = 0.832). Weekly consumption of fried foods, candy, and soft drinks is part of the routine of 48.3%, 56.7%, and 43.3% of children, respectively, as well as daily intake of fruits (86.7%), vegetables (88.3%), and grains (93.3%), with no significant difference between normal-weight and overweight. Most children (71.7%) had their meals while watching television and were accompanied by family members or caregivers (98.3%).
All children were physically active, played at home, at school, or on a regular schedule: 83.3% up to three times a week and 16.7% more than this. On the other hand, 62.7% spent 1–2 h/d watching TV and/or on video games, while 30.5% reported 3 to 5 h/d of screen time.
Clinical and biochemical characteristics of SGA and AGA children showed no differences at the evaluation time (Table 2).
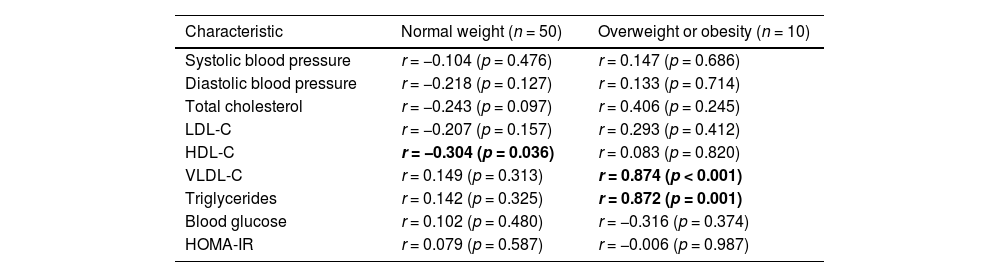
There was a positive correlation between GA and triglyceride and VLDL-C levels in overweight children, and a weak negative correlation with HDL-C in normal-weight children, at the time of evaluation (Table 3).
Association between gestational age (weeks) and clinical-biochemical characteristics of 60 preterm schoolchildren according to the BMI classification*, followed-up at the outpatient clinic for children at risk (ACRIAR/UFMG) from June 2017 to July 2018.
Multivariate analysis showed no association between GA and any studied variables.
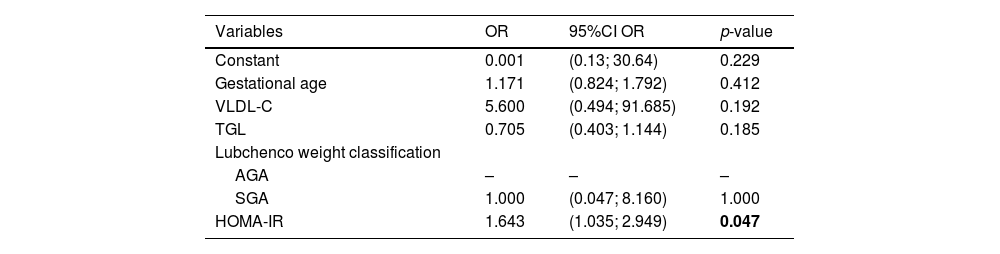
The insulin resistance index was high in eight children (13.3%); they were all born AGA, and three (37.5%) presented neither excess weight, nor altered waist-to-height ratio. Overweight children had a higher rate of insulin resistance when compared to those with an appropriate BMI for their age (p = 0.002). The addition of one HOMA-IR unit increased the chance of the patient being overweight by 1.64 times (Table 4).
Variables associated with overweight or obesity in 60 preterm schoolchildren and followed-up at the outpatient clinic for children at risk (ACRIAR/UFMG) from June 2017 to July 2018.
Variables: Gestational age (weeks), VLDL-C, TGL (continuous), HOMA-IR (continuous).
We observed metabolic disorders parameters in children born preterm when evaluated at school age. Excess weight was present in 16.6% of children, 13.3% had reduced insulin sensitivity, and 36.7% presented abnormal BP. Therefore, approximately one-third of preterm children had altered metabolic profiles and excess weight.
Adverse metabolic outcomes have been reported among children or young adults born preterm, and in very preterm or extremely preterm infants, cardiometabolic changes typically begin during infancy or school age1. However, controversies stillremain on the subject.
There are few reports regarding the occurrence of obesity and overweight at school age associated with premature birth. In a French follow-up of very preterm infants, it was found, at five years old, a prevalence of excess weight of 10.8% (95% CI 9.5% to 12.2%) and 6.6% (95% CI 5.2% to 8.3%) in two cohorts, EPIPAGE2 and LIFT, and 13.9% (95% CI 10.5% to 18.3%) in another cohort, EPIPAGEADO.17
The occurrence of overweight and obesity of 16.6% (8.3% overweight and 8.3% obese) found in our study was higher than that of the two French cohorts when the children were evaluated at five years of age, even though the GA of children was similar. However, it was lower than the findings of 388 preterm newborns with GA < 28 weeks, of which 22% were overweight and 10% obese when evaluated at age 6–7 years.18 These high rates of overweight or obesity in extremely preterm newborns (< 28 weeks) raise the question of whether they are comparable to newborns with higher GA.
Being overweight is influenced by multiple genetic, environmental, and epigenetic factors. The “advanced” age of our group, which ranged from 6.1 to 7.5 years, compared to the three previous cohorts, that was around five years older, may explain this difference in overweight and obesity, in addition to socioeconomic differences, eating habits and other epigenetic factors that could be involved.
The maternal BMI at enrollment and a trajectory of infant BMI Z-score change during the first year of corrected age were the most critical associated factors to the development of 12.9% overweight or obesity at age 4–7 years in a study involving 2125 preterm infants.19 The introduction of solid foods after six months of corrected age compared to introduction with less than three months of corrected age was significantly associated with 11% lower risk (risk ratio, 0.89; 95% CI, 0.82 to 0.97) of an unfavored pattern of BMI Z-score change.19 None of the factors such as the mother`s BMI and the pattern of the infants’ weight gain had been studied in our series. However, too rapid postnatal weight gain, increased risk for insulin resistance, and increased adiposity in children and adults have been linked.20 The first years of life are a window of opportunity to prevent these adverse outcomes in the future. Early weaning, as observed in children in the current series, is associated with excessive weight gain, while breastfeeding is increasingly potent in preventing childhood diseases. Exclusively breastfed preterm and SGA children showed more significant catch-up growth with no increase in adiposity or insulin resistance, compared to AGA children at two years of age.21
It is essential to note that preventive measures should already be adopted during pregnancy, since prenatal factors, such as maternal obesity, are associated with unfavorable metabolic outcomes for the child. However, perinatal and postnatal factors are of great relevance.22 Preterm children are particularly susceptible to programming unfavorable health conditions related to intrauterine growth restriction. Adaptive mechanisms, potentially deleterious in the long term, lead to permanent morphological and functional changes in organs and systems and increase the risk for chronic non-communicable diseases. In addition, programming can continue into the early postnatal period, and both periods are critical for developing organs and systems.5
Bad eating habits and a sedentary lifestyle are part of the current context of the global obesity epidemic.23 We observed that 80% of children reported inadequate eating habits. The overweight children studied may reflect what has been observed in 33.5% of Brazilian children between 5 and 9 years of age, and in the general population.24 Furthermore, overweight children in this series presented alterations typically found in metabolic syndrome. Dyslipidemia, specifically increased triglycerides, and low HDL is often associated with obesity.25 Nonetheless, the eating habits of overweight children did not differ from those of normal weight and were not associated with BMI.
There is still controversy regarding the association between prematurity and the risk of being overweight later in life. A systematic review and meta-analysis comparing metabolic syndrome markers between preterm and full-term newborns had not found a high-fat mass in adulthood.5 Another systematic review and meta-analysis showed a high-fat mass, and increased blood pressure, cholesterol levels, fasting glucose, insulin, and insulin resistance index to be associated with premature birth, but not overweight.2
The association between metabolic syndrome parameters and prematurity has mainly been demonstrated for preterm SGA infants, and the evidence is less strong regarding the link between preterm birth and the development of the syndrome components.2 Prepubertal children born very preterm and AGA showed a lower proportion of HDL-C higher than 40 mg/dl and a higher proportion of BP > 90th percentile than children born at term.25,26 Although it is still not a defined diagnosis, the finding of abnormal BP in the present series, draws attention. Increased blood pressure is a relevant metabolic syndrome marker reported in many series comparing individuals born preterm and full-term in adulthood.2,4
Another relevant parameter, increased abdominal adiposity was predominant in overweight children, in the present series, although we also observed it in normal-weight subjects. Excess abdominal adiposity is a recognized independent risk factor for cardiovascular events in adulthood and has already been reported in children, even without increased BMI. Serial waist circumference measurements in preterm children, at ages 2 and 5, showed an increase in waist circumference at two years, despite a normal BMI, pointing to an adverse outcome.27 Despite the difficulties in standardizing reference values in childhood, waist circumference is used to complement risk assessment in pediatric patients, since it is an easily accessible tool.11 Some authors have suggested substituting the waist circumference measurement for the waist/height ratio, but it seems both index are good to evaluate central adiposity.11 We found a similar percentage of alterations using both methods in our series.
A significant percentage of the children evaluated here showed evidence of insulin resistance, especially - but not exclusively - those with excess weight. Those presenting excess weight had higher waist circumferences and higher HOMA-IR than normal-weight children. Changes in carbohydrate metabolism have also been reported in preterm and SGA children, related to lower insulin-secreting capacity, and reduced peripheral sensitivity, which can manifest in the neonatal period and later in childhood and adolescence. Therefore, being born SGA or preterm is an added risk factor for developing type 2 diabetes in adulthood.28 In a retrospective evaluation at 6–8 years of age, 60 children born < 30 weeks or with birth weight < 1500 g showed higher values of fasting glucose, insulin, and insulin resistance (HOMA-IR) compared to children born at term.1
In the present study, we showed that 16.7% of SGA children, despite reflecting data for preterm infants in the general population,28 did not differ from AGA regarding clinical (body weight, blood pressure) or biochemical variables (serum lipids, blood glucose, HOMA-IR).
In a multicentre retrospective cohort study to evaluate the prevalence and risk factors for childhood excess weight in 911 children born < 1500 g or < 29 weeks gestation at 3-year corrected age, it was found that 2.4% had overweight or obesity, and no association between SGA with these variables.29 In a systematic review and meta-analysis, the association between SGA with overweight and obesity was also not found, despite a strong association with other components of the metabolic syndrome and/or additional indicators of increased cardiovascular risk in adult life.2
The excess weight combined with increased abdominal adiposity, reduced insulin sensitivity, and lipid profile with alterations characteristic of the metabolic syndrome suggests a percentage of children in the present series, may be at increased risk for adverse metabolic outcomes in the future. Moreover, bad eating habits can decisively contribute to this risk phenotype. Finally, it is worth remarking that many children presented altered parameters of the metabolic profile despite not having excess weight.
We are aware the present study has some limitations, mainly concerning the relatively small sample size, from a single center, which precludes the generalization of our findings.
The prevalence of preterm births is relatively high in developing countries, accounting for 11.7% in Brazil.30 Therefore, establishing the risk factors for developing overweight/obesity or other morbidities in this population is crucial to implement prevention and treatment interventions.
In conclusion, an expressive number of school children born with GA <34 weeks, regardless of being AGA or SGA, were overweight and presented increased abdominal adiposity, reduced insulin sensitivity, altered blood pressure, and lipid profile. Therefore, these findings for this specific group of children should be confirmed.
We would like to thank Dra. Maria de Fátima Sabino Viana for her contribution to this work.
Institution: Universidade Federal de Minas Gerais. Belo Horizonte, Minas Gerais, Brazil.