To investigate the association between pacifier use and bottle-feeding and unfavorable behaviors during breastfeeding.
MethodA cross-sectional study was conducted with 427 babies/mothers. Socio-demographic, perinatal data, and information about the use of artificial nipples (pacifier and/or bottle) were collected through a questionnaire. The breastfeeding aspects regarding position, affectivity, sucking behavior, baby responses, and breast anatomy were evaluated through observation during breastfeeding. The chi-squared test and the multiple linear regression analysis were used to investigate the association between the variables.
ResultsThe aspects of breastfeeding that showed higher percentages of the category “poor” were sucking behavior (22.5%) and position (22.2%). The group of infants who used pacifiers and/or bottle showed higher percentages in the poor and fair categories when compared with the good category for all five breastfeeding aspects evaluated (p<0.001). The linear regression analysis revealed that the increase in the number of unfavorable behaviors regarding position, affectivity, sucking behavior, and baby responses were independently associated with both pacifier and bottle use (β positive, p<0.05), while breast anatomy was independently associated only with bottle use.
ConclusionThe findings suggest that the use of pacifiers and/or bottle-feeding may be associated with unfavorable behaviors during breastfeeding, especially the use of bottle-feeding.
Investigar a associação entre uso de chupeta e mamadeira e comportamentos desfavoráveis à amamentação durante as mamadas.
MétodosUm estudo transversal foi conduzido com 427 bebês/mães. Foram coletados dados sociodemográficos, perinatais e sobre o uso de bicos artificiais (chupeta e/ou mamadeira) através de questionário. Os aspectos de amamentação referentes à posição, afetividade, adequação da sucção, respostas do bebê e anatomia das mamas foram avaliados através da observação durante a mamada. O teste qui-quadrado e a análise de regressão linear múltipla foram usados para investigar associação entre as variáveis.
ResultadosOs aspectos de amamentação que apresentaram percentuais mais elevados da categoria ruim foram a adequação da sucção (22,5%) e posição (22,2%). O grupo de bebês que usavam chupeta e/ou mamadeira apresentou percentuais mais elevados nas categorias ruim e regular quando comparados com a categoria bom para todos os cinco aspectos da amamentação avaliados (p <0,001). A análise de regressão linear revelou que o incremento do número de comportamentos desfavoráveis referentes à posição, afetividade, adequação da sucção e respostas do bebê estavam associados de forma independente tanto ao uso de chupeta quanto ao uso de mamadeira (β positivo, p <0,05), enquanto que anatomia das mamas estava associado de forma independente apenas com o uso de mamadeira.
ConclusãoOs achados sugerem que o uso de chupeta e/ou mamadeira pode estar associado a comportamentos desfavoráveis durante amamentação, em especial, o uso de mamadeira.
Breastfeeding (BF) is recognized as the ideal strategy for infant feeding, particularly in the first six months of life, during which exclusive breastfeeding is recommended.1 In addition to the nutritional advantages, BF enhances the immune response, reducing the incidence of infections and other childhood morbidities. For the nursing mother, this practice is associated with a lower risk for the development of type 2 diabetes mellitus, breast cancer, and ovarian cancer.2
Estimates indicate a modest increase in the prevalence of exclusive breastfeeding (EBF) among infants aged under 6 months in developed countries, from 33% in 1995 to 39% in 2010.3 In Brazil, this prevalence was 41% in all Brazilian capitals in 2008, showing a very heterogeneous behavior among the different regions.4 According to the parameters of the World Health Organization (WHO), EBF prevalence rates below 50% are considered poor.1
Several factors are associated with poor adherence to BF, including: family characteristics, factors related to prenatal and postnatal care, offer of alternative artificial formulas, return to work/studies, and lack of legal protection for breastfeeding.5–7 In addition to the aforementioned factors, the use of pacifiers and bottles has also been considered a strong risk factor for early weaning.8–12 The biological plausibility of this association is based on the dysfunction of muscle dynamics caused by the use of these devices,13–15 leading the baby to inadequate sucking behaviors.12
In turn, some systematic reviews indicated that the pacifier use does not interfere with BF16,17; however, both studies analyzed only the duration and exclusiveness of the outcome. Moreover, the American Association of Pediatrics started to suggest the use of pacifiers as a form of prevention of sudden death syndrome in childhood,18 contrary to the recommendations made by the WHO and the United Nations Children's Fund (UNICEF), which expressly recommend not using these devices in breastfed infants, aiming to achieve BF success.19
Considering the lack of consensus on the effects of pacifier use and/or bottle-feeding on BF practice, the aim of the present study was to investigate the association between the use of these artificial devices and the presence of unfavorable BF behaviors.
MethodsA cross-sectional observational study was carried out in the city of São Luís, MA, Brazil, between February and October 2016. The study was approved by the Research Ethics Committee of Universidade Federal do Maranhão, under Opinion No. 1,412,752. All mothers were informed about the study objectives and procedures and signed the free and informed consent form.
The representative sample was calculated considering the following parameters: the number of live births in the Health District of São Luís (22,669 in 2015), the prevalence rate of bottle feeding in the city of São Luís (42.7%),4 a sample error of 5%, confidence level of 95%, and a loss rate of 15%. Thus, the required size comprised 427 babies/mothers.
Infants born at full term, aged between 5 and 120 days, treated for the first time at a Childcare Service at Hospital Universitário da Universidade Federal do Maranhão (HUUFMA) were included in the study. The exclusion criteria comprised infants who had craniofacial anomalies, congenital neuropathies, and twin pregnancies, as well as mothers who were unable to breastfeed due to some disease or mammillary traumas that made sucking impossible.
Data collection was performed prior to childcare consultation, to avoid a possible influence after the guidelines received from the healthcare team. The initial interview consisted of questions asked verbally based on a semi-structured questionnaire, which included the following variables: baby's gender and age; maternal age, marital status, occupation, and schooling; family income (in Brazilian minimum wages); pregnancy data, such as primiparity, type of delivery (cesarean section or vaginal), prenatal care, place of delivery, and information received on BF; and the use of pacifiers and/or bottle-feeding.
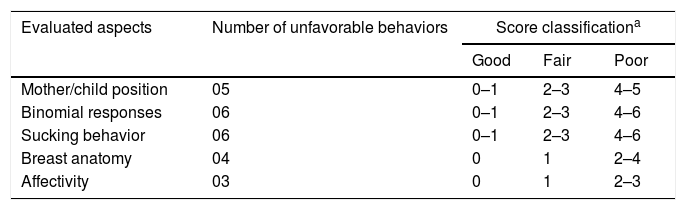
BF was assessed by a single trained examiner (CLCB) using the adapted B-R-E-A-S-T-Feeding Observation Form.20 The tool evaluates the binomial (baby/mother) through direct observation of favorable behaviors or those suggesting difficulties during BF, regarding the aspects of position, baby's responses, establishment of affective ties, breast anatomy, and sucking behaviors. These five aspects of BF were ordinally classified (as good, fair, or poor) according to the number of unfavorable behaviors observed (Table 1), considering the previously used methodology.20
Criteria for classification of the scores used in the breastfeeding assessment according to each evaluated aspect.
| Evaluated aspects | Number of unfavorable behaviors | Score classificationa | ||
|---|---|---|---|---|
| Good | Fair | Poor | ||
| Mother/child position | 05 | 0–1 | 2–3 | 4–5 |
| Binomial responses | 06 | 0–1 | 2–3 | 4–6 |
| Sucking behavior | 06 | 0–1 | 2–3 | 4–6 |
| Breast anatomy | 04 | 0 | 1 | 2–4 |
| Affectivity | 03 | 0 | 1 | 2–3 |
At this stage, the mothers were advised to breastfeed in the usual way. The BF episode was considered to be the one starting from the maternal intention to breastfeed, by placing the baby in her lap, trying to get the baby to latch, whereas the baby demonstrates the first characteristic oral reflexes of latching aptitude, followed by effectively latching and stabilization of the BF. The babies were assessed with an active level of awareness. All data collections were carried out in the morning.
Data were analyzed using the SPSS (SPSS Statistics for Windows, version 17.0, IL, USA). Descriptive statistics were performed using measures of absolute frequency, percentages, means, and standard deviation. The chi-squared test was used to analyze the distribution of classification scores regarding the aspects of BF observation between the groups with or without pacifier and/or bottle-feeding.
Multiple linear regression analysis was used to investigate the influence of the independent variables baby's age (in days), maternal age (in years), mother's number of children, information on BF (no=0, yes=1), previous experience of BF (no=0, yes=1), bottle-feeding (no=0, yes=1), and pacifier use (no=0, yes=1), on the dependent variables represented by the number of negative behaviors observed during BF regarding position, affectivity, sucking behavior, baby's responses, and breast anatomy. The dependent variables included in the regression model showed a normal distribution, measured through the D’Agostino-Pearson test. A significance level of 5% was used for all the analyses.
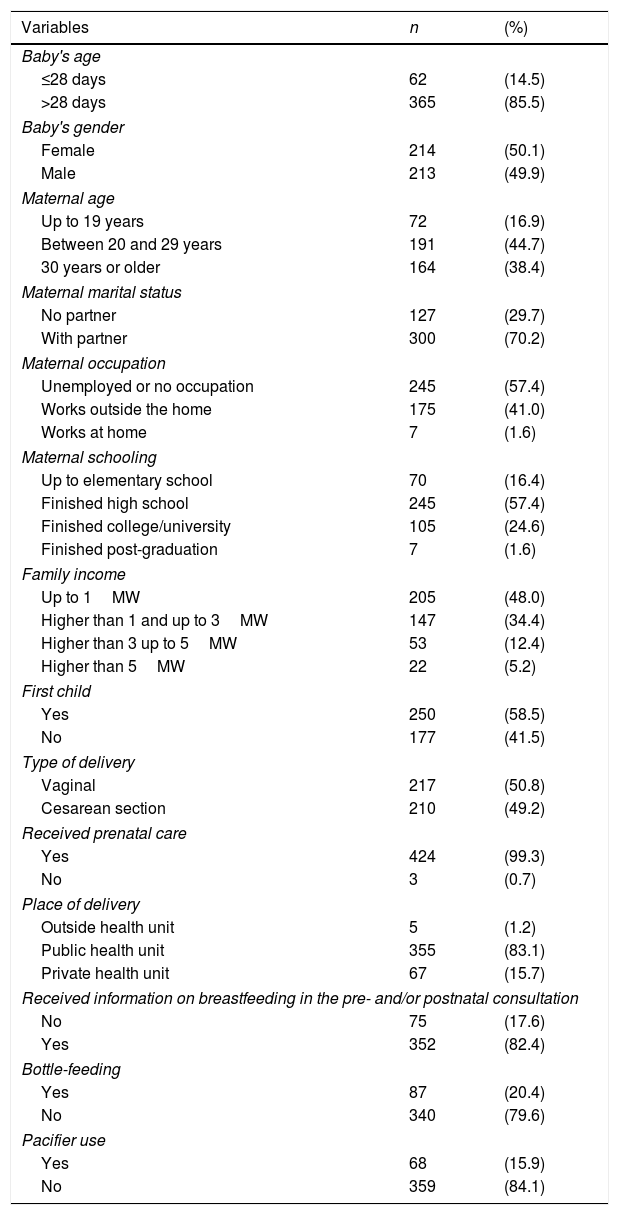
ResultsTable 2 shows the characteristics of the babies/mothers included in the study. Most infants were older than 28 days (85.5%). Maternal age ranged from 13 to 47 years, and 44.7% of them were in the age range between 20 and 29 years. Most mothers (85.5%) reported they received information about BF during prenatal and/or postnatal visits. It was observed that, in this sample, 20.4% used bottle-feeding and 15.9% used pacifiers.
Distribution of variables of general characterization, pacifier use, and bottle-feeding.
| Variables | n | (%) |
|---|---|---|
| Baby's age | ||
| ≤28 days | 62 | (14.5) |
| >28 days | 365 | (85.5) |
| Baby's gender | ||
| Female | 214 | (50.1) |
| Male | 213 | (49.9) |
| Maternal age | ||
| Up to 19 years | 72 | (16.9) |
| Between 20 and 29 years | 191 | (44.7) |
| 30 years or older | 164 | (38.4) |
| Maternal marital status | ||
| No partner | 127 | (29.7) |
| With partner | 300 | (70.2) |
| Maternal occupation | ||
| Unemployed or no occupation | 245 | (57.4) |
| Works outside the home | 175 | (41.0) |
| Works at home | 7 | (1.6) |
| Maternal schooling | ||
| Up to elementary school | 70 | (16.4) |
| Finished high school | 245 | (57.4) |
| Finished college/university | 105 | (24.6) |
| Finished post-graduation | 7 | (1.6) |
| Family income | ||
| Up to 1MW | 205 | (48.0) |
| Higher than 1 and up to 3MW | 147 | (34.4) |
| Higher than 3 up to 5MW | 53 | (12.4) |
| Higher than 5MW | 22 | (5.2) |
| First child | ||
| Yes | 250 | (58.5) |
| No | 177 | (41.5) |
| Type of delivery | ||
| Vaginal | 217 | (50.8) |
| Cesarean section | 210 | (49.2) |
| Received prenatal care | ||
| Yes | 424 | (99.3) |
| No | 3 | (0.7) |
| Place of delivery | ||
| Outside health unit | 5 | (1.2) |
| Public health unit | 355 | (83.1) |
| Private health unit | 67 | (15.7) |
| Received information on breastfeeding in the pre- and/or postnatal consultation | ||
| No | 75 | (17.6) |
| Yes | 352 | (82.4) |
| Bottle-feeding | ||
| Yes | 87 | (20.4) |
| No | 340 | (79.6) |
| Pacifier use | ||
| Yes | 68 | (15.9) |
| No | 359 | (84.1) |
n, absolute frequency; %, relative frequency; MW, Brazilian minimum wage.
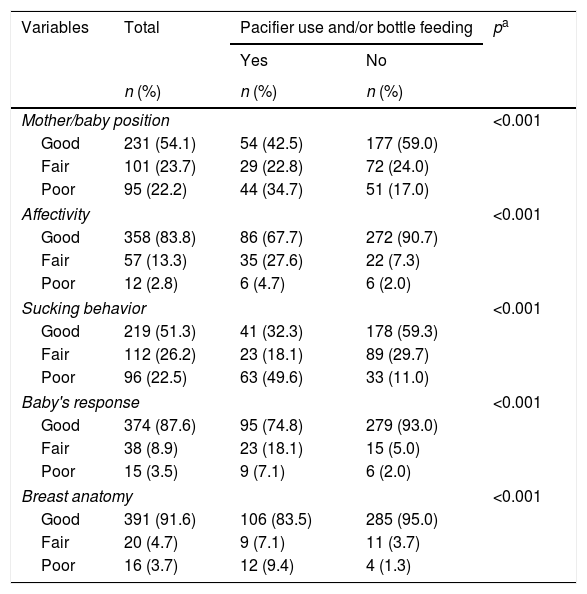
The distribution of the observed aspects of BF and association with pacifier use and/or bottle-feeding is shown in Table 3. The aspects that showed a higher percentage classified as poor in the total sample were the sucking behavior (22.5%) and position (22.2%). The group of babies who used pacifiers and/or were bottle-fed showed higher poor scores for all five BF aspects analyzed (p<0.001), with emphasis on sucking behavior; almost 50% of the babies in this group presented poor scores in the latter aspect.
Distribution of breastfeeding evaluation criteria between groups with or without pacifier use and/or bottle-feeding.
| Variables | Total | Pacifier use and/or bottle feeding | pa | |
|---|---|---|---|---|
| Yes | No | |||
| n (%) | n (%) | n (%) | ||
| Mother/baby position | <0.001 | |||
| Good | 231 (54.1) | 54 (42.5) | 177 (59.0) | |
| Fair | 101 (23.7) | 29 (22.8) | 72 (24.0) | |
| Poor | 95 (22.2) | 44 (34.7) | 51 (17.0) | |
| Affectivity | <0.001 | |||
| Good | 358 (83.8) | 86 (67.7) | 272 (90.7) | |
| Fair | 57 (13.3) | 35 (27.6) | 22 (7.3) | |
| Poor | 12 (2.8) | 6 (4.7) | 6 (2.0) | |
| Sucking behavior | <0.001 | |||
| Good | 219 (51.3) | 41 (32.3) | 178 (59.3) | |
| Fair | 112 (26.2) | 23 (18.1) | 89 (29.7) | |
| Poor | 96 (22.5) | 63 (49.6) | 33 (11.0) | |
| Baby's response | <0.001 | |||
| Good | 374 (87.6) | 95 (74.8) | 279 (93.0) | |
| Fair | 38 (8.9) | 23 (18.1) | 15 (5.0) | |
| Poor | 15 (3.5) | 9 (7.1) | 6 (2.0) | |
| Breast anatomy | <0.001 | |||
| Good | 391 (91.6) | 106 (83.5) | 285 (95.0) | |
| Fair | 20 (4.7) | 9 (7.1) | 11 (3.7) | |
| Poor | 16 (3.7) | 12 (9.4) | 4 (1.3) | |
n, absolute frequency; %, relative frequency.
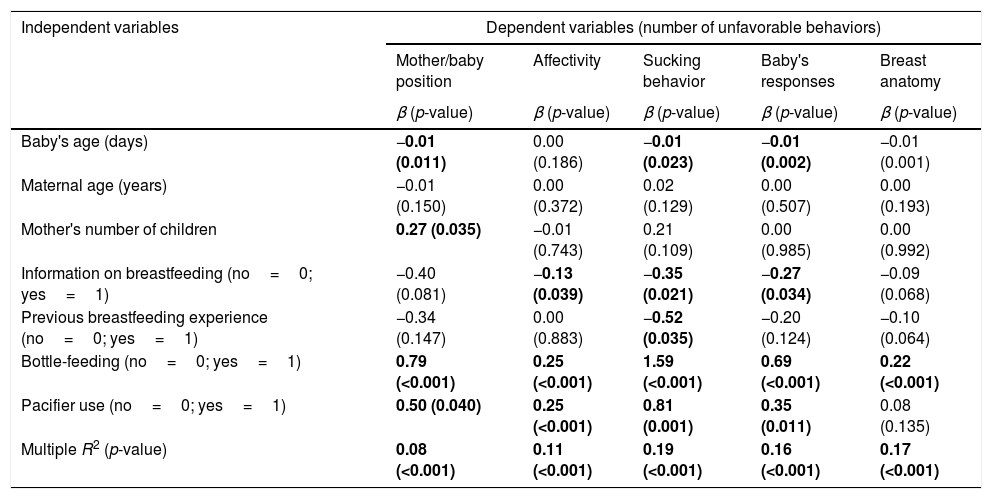
Moreover, the influence of independent variables on the number of unfavorable behaviors observed during BF (Table 4) was tested. It was observed that the increase in the baby's age, number of children, information on BF, and previous experience of BF were factors that reduced some unfavorable aspects of BF (negative β, p<0.05).
Simple and multivariate linear regression analysis of factors associated with the number of unfavorable behaviors observed during breastfeeding.
| Independent variables | Dependent variables (number of unfavorable behaviors) | ||||
|---|---|---|---|---|---|
| Mother/baby position | Affectivity | Sucking behavior | Baby's responses | Breast anatomy | |
| β (p-value) | β (p-value) | β (p-value) | β (p-value) | β (p-value) | |
| Baby's age (days) | −0.01 (0.011) | 0.00 (0.186) | −0.01 (0.023) | −0.01 (0.002) | −0.01 (0.001) |
| Maternal age (years) | −0.01 (0.150) | 0.00 (0.372) | 0.02 (0.129) | 0.00 (0.507) | 0.00 (0.193) |
| Mother's number of children | 0.27 (0.035) | −0.01 (0.743) | 0.21 (0.109) | 0.00 (0.985) | 0.00 (0.992) |
| Information on breastfeeding (no=0; yes=1) | −0.40 (0.081) | −0.13 (0.039) | −0.35 (0.021) | −0.27 (0.034) | −0.09 (0.068) |
| Previous breastfeeding experience (no=0; yes=1) | −0.34 (0.147) | 0.00 (0.883) | −0.52 (0.035) | −0.20 (0.124) | −0.10 (0.064) |
| Bottle-feeding (no=0; yes=1) | 0.79 (<0.001) | 0.25 (<0.001) | 1.59 (<0.001) | 0.69 (<0.001) | 0.22 (<0.001) |
| Pacifier use (no=0; yes=1) | 0.50 (0.040) | 0.25 (<0.001) | 0.81 (0.001) | 0.35 (0.011) | 0.08 (0.135) |
| Multiple R2 (p-value) | 0.08 (<0.001) | 0.11 (<0.001) | 0.19 (<0.001) | 0.16 (<0.001) | 0.17 (<0.001) |
β, coefficient of regression; R2, coefficient of determination.
Statistically significant measurements indicated in bold.
Regarding the association between pacifier use and bottle-feeding and unfavorable BF behaviors, the main objective of this study, the analysis showed that bottle-feeding increased the number of negative behaviors for all five BF aspects investigated, while the use of pacifiers also was associated with an increase in four aspects, although at lower values when compared with bottle-feeding. The multivariate analysis suggested that sucking behavior was the aspect most often influenced by the variables included in the model (R2=0.19, p<0.001).
DiscussionThe main findings of this study suggest that infants who use pacifiers and/or are bottle-fed have a higher frequency of indicators of BF difficulties when compared with those who do not use these devices. Furthermore, bottle-feeding was associated with a significant increase in unfavorable behaviors for all five aspects of BF assessed, while pacifier use was associated with an increase in negative behaviors observed for all BF aspects but breast anatomy.
In the present study, the aspects most often affected by bottle-feeding were the mother/baby position and breast suction. The authors of a longitudinal study that evaluated BF at the maternity hospital and at 30 days also suggested that bottle-feeding influences the BF technique, emphasizing the causality direction, since the worsening of the indicators related to the positioning and the latching in the group of infants who were bottle-fed occurred only in the second assessment time.21 This interaction is supported by evidence that demonstrates that bottle-feeding interferes with the orofacial development, mainly due to the dysfunction of position and muscle action of lips and tongue.13–15
Additionally, infants receiving mixed feeding (breast and bottle) position the tongue as a piston when sucking the breast, a behavior that is common when sucking the bottle, but not when sucking the breast (represented by undulatory movements), emphasizing the muscle pattern change after the introduction of the bottle.22
The association of bottle-feeding with negative behaviors regarding breast anatomy can be explained mainly by the presence of mammillary traumas,23 which together with the inadequate latching and position, may favor irregular and insufficient milk extraction.24 Breast problems such as those indicated in the breast anatomy assessment form (e.g., abrasions and fissures), are also commonly reported as risk factors for early weaning.25
In the present study, pacifier use increased the number of unfavorable behaviors regarding the aspects of the mother/baby position, affectivity, baby's response, and sucking behaviors. Kronborg and Væth26 also observed that the use of pacifiers was associated with an inefficient BF technique, especially regarding the latching and position aspects. The results of this study corroborate the hypothesis that the use of artificial nipples may imply unfavorable behaviors to milk withdrawal from the mother's breast, causing complications for the baby's oral skills.
Oral dysfunction in healthy neonates is indicated as one of the factors that interferes with the onset of lactation.27 The increase in the number of negative behaviors associated with affectivity and the baby's response observed in the present study can be explained by evidence suggesting that the use of pacifiers decreases milk production, since babies request the breast less often, causing lesions to the mother due to inadequate latching, which even interferes with their own weight gain,14 a fact that may increase the risk of early weaning.9
It is worth mentioning that most babies in this study were assessed during the period of BF onset or stabilization, which occurs in the first weeks of life and are crucial for the overcoming of difficulties associated with the correct latching technique. Healthy full-term infants are able to locate the nipple even without assistance when placed at the breast or on the mother's abdomen. In this process, the correct sucking pattern is necessary to ensure that the child has a good configuration of the oral components to facilitate milk descent,28 since the babies show different sucking patterns depending on the type of nipple or on whether or not food is offered to them.29
Some procedures used in this study are noteworthy. For instance, the choice of the UNICEF/WHO data collection form, a measure used due to its broad spectrum of observable attitudes, thus providing a better picture of BF. Furthermore, this tool is used to train health teams in units accredited as “Baby-Friendly.”19 Another positive point was the calculation of the representative sample size for the São Luís Health District, which allows inferring the results observed for this population. A study limitation was its cross-sectional design, which does not allow excluding the reverse-causality bias; however, França et al.21 had already suggested, in a longitudinal study, that the use of bottle-feeding influences the BF technique, not the opposite, which was used in the present study.
The results of this study indicate that babies who used pacifiers and/or were bottle-fed showed a deficit in the aspects considered adequate for the practice of ideal BF, especially regarding the aspects of suction, mother/baby position, affectivity, and baby responses to the breast. New studies should be planned for new approaches to the subject, using longitudinal designs and tools that evaluate oral dysfunction and quantifying the time of pacifier use and bottle-feeding.
Moreover, studies indicate that health education, advice provided by professionals, and management assistance promoted by health professionals result in a better BF practice.29 Thus, it is important that educational actions be directed to these objectives, aiming to preventing problems related to BF.
Conflicts of interestThe authors declare no conflicts of interest.
To all the mothers who voluntarily participated in this research. To Hospital Universitário da Universidade Federal do Maranhão (HUUFMA) for the logistic support.
Please cite this article as: Batista CL, Ribeiro VS, Nascimento MD, Rodrigues VP. Association between pacifier use and bottle-feeding and unfavorable behaviors during breastfeeding. J Pediatr (Rio J). 2018;94:596–601.
Study carried out at Universidade Federal do Maranhão (UFMA), University Hospital, São Luís, MA, Brazil.