to evaluate associations between morphometric variables, cervical circumference (CC), and abdominal circumference (AC) with the presence of nocturnal desaturation in children and adolescents with sickle-cell anemia.
Methodsall patients were submitted to baseline polysomnography, oral cavity measurements (maxillary intermolar distance, mandibular intermolar distance, and overjet), and CC and AC measurements.
Resultsa total of 85 patients were evaluated. A positive correlation was observed between the height/age Z-score and CC measurement (r = 0.233, p = 0.031). The presence of nocturnal desaturation was associated with CC (59.2± 9.3 vs. 67.5 ± 10.7, p = 0.006) and AC measurements (27.0 ± 2.0 vs. 29.0± 2.1, p = 0.028). There was a negative correlation between desaturation and maxillary intermolar distance (r = -0.365, p = 0.001) and mandibular intermolar distance (r = -0.233, p = 0.037).
Conclusionsthe morphometric variables of CC and AC may contribute to raise suspicion of nocturnal desaturation in children and adolescents with sickle-cell anemia.
avaliar associações entre variáveis morfométricas e circunferências cervical (CC) e abdominal (CA) com a presença de dessaturação noturna em crianças e adolescentes com anemia falciforme.
Métodostodos os pacientes foram submetidos à polissonografia basal, medidas da cavidade oral (distância intermolar da maxila, distância intermolar da mandíbula e overje), CC e CA.
Resultadosforam avaliados 85 pacientes. Foi observada correlação positiva entre o escore Z altura/idade e a medida da circunferência cervical (r = 0,233 p = 0,031). A presença da dessaturação noturna associou-se com as medidas da circunferência cervical (59,2 + 9,3 vs 67,5 + 10,7; p = 0,006) e abdominal (27,0 + 2,0 vs 29,0 + 2,1; p = 0,028). Houve correlação negativa entre a dessaturação e a distância entre os segundos molares da maxila (r = - 0,365, p = 0,001) e da mandíbula (r = - 0,233, p = 0,037).
Conclusõesas variáveis morfométricas e circunferências cervical e abdominal podem contribuir para a suspeita da dessaturação noturna em crianças e adolescentes com anemia falciforme.
The main aspect of sickle-cell anemia (SCA) physiopathology is the vaso-occlusive crisis, also called a painful crisis, resulting from the polymerization of hemoglobin S that causes red blood cells to assume a “sickle” shape, resulting in the obstruction of small-caliber blood vessels, tissue hypoxia, necrosis, and severe pain.1
Among the consequences of red blood cell sickling are painful vaso-occlusive crises, stroke,2 and chronic hemolytic anemia.3 Pulmonary complications account for 20% to 30% of deaths in adults with SCA, followed the pulmonary lesions caused by upper airway (UA) obstruction.4
Regarding children with SCA, an important causal factor of airway obstruction is adenotonsillar hypertrophy (ATH). Salles et al.5 observed a prevalence of 55.3% of obstructive ATH in children and adolescents with SCA. When this UA obstruction is associated with obstructive sleep apnea syndrome (OSAS), it can precipitate episodes of hypoxemia,6 increasing the risk of vaso-occlusive crises.7
The nocturnal arterial oxyhemoglobin desaturation in SCA occurs in up to 83% of children with the disease, and may result from OSAS or pulmonary disease, or may be secondary to the decreased oxygen affinity of hemoglobin S.8 Oxyhemoglobin desaturation is common during sleep, which is associated with hypoventilation and is exacerbated by UA obstruction;6 in patients with SCA, there may be increased risk for airway obstruction due to ATH.9
Factors that worsen UA obstruction are ATH and the craniofacial consequences caused by obstructive ATH itself, such as predominant mouth breathing; vertical, horizontal, and transverse maxillary alterations, incompetent lip seal; and unbalanced orofacial muscles, mainly the mandibular elevator and depressor muscles.10,11
Thus, the present study aimed to evaluate associations between morphometric variables, cervical circumference (CC), and abdominal circumference (AC) with the presence of nocturnal desaturation in children and adolescents with SCA.
Material and MethodsThis was a cross-sectional, contemporary cohort study with sequential allocation of 85 patients with SCA enrolled in a referral center for hematology and transfusion medicine, between May of 2007 and May of 2008. The following inclusion criteria were used: diagnosis of SCA attained through the quantitative analysis of hemoglobin by hemoglobin electrophoresis or high-performance liquid chromatography (HPLC), performed with Variant II equipment (Bio-Rad, USA); age between 2 and 19 years; clinically stable; completed the questionnaire; allowing pediatric and otorhinolaryngological evaluation; and undergoing nocturnal polysomnography. The following exclusion criteria were used: other genetic syndromes, debilitating diseases, acute hepatitis, previous treatment for OSAS or recent craniofacial trauma; using hypnotic drugs; having been treated with corticosteroids; pregnancy; and presence of infection during the evaluation.
The PEPI-Sample program (Sagebush Press,USA) was used to calculate sample size, and the following parameters were used: a confidence level of 95%, and the prevalence of OSAS in children/adolescents of 5% (4.9% as an acceptable prevalence difference).
The sample was obtained from a population of approximately 1,000 children and adolescents with SCA, registered at a referral center for hematology and transfusion medicine. Therefore, to meet the objectives, the calculated sample size consisted of 71 patients. Considering 10% losses, the total (n) consisted of 78 patients.
Age was measured in full years, according to the birth date. Ethnicity was self-reported, according to the official nomenclature of demographic censuses, using skin color as reference (white, mixed-race, or black).
Weight was measured using a mechanical scale (model 131; Filizola - Brazil). Length was measured with a stadiometer. These measurements were compared to the growth charts of the National Center for Health Statistics and converted into Z-scores for body mass index (BMI), weight/age, and height/age based on age and gender, using the Epi-Info software (release 3.4.1;CDC- USA).
The oral cavity assessment was performed by a single otolaryngologist in the Frankfurt position, using a standard tool. The measures of the oral cavity, except the overjet (OJ), were made with the tongue in a relaxed position and with a mouth opening angle of 20° to the mandibular condyle. For that purpose, a dry-point, 20° fixed-aperture compass was used, which was placed on the topography of the temporomandibular joint, the tip of its upper leg aligned with the upper central incisors and the lower compass leg aligned with the lower central incisors, to yield the desired mouth opening.
Another compass was used to obtain the oral cavity measurements (maxillary intermolar distance, defined as the size of the maxilla; and mandibular intermolar distance, defined as mandibular size), which were then transposed to a ruler. To measure the OJ, a 40- mm ruler was used; to measure CC, a metric tape was placed at the cricothyroid membrane, and for AC, the same tape was used, after being placed at the umbilicus.10
Patients were submitted to polysomnography, accompanied by a parent or guardian, for at least 10h, in a quiet environment, with appropriate temperature and lighting for the examination. This was performed during spontaneous sleep, with no prior sedation or sleep deprivation, avoiding stimulating foods (coffee, chocolate, soda, and black tea). Polysomnography was conducted in a hospital setting, using Sonolab 620 computerized equipment (Medtron - Brazil), and the report was issued by the same observer. The following were recorded during the polysomnography: EEG (C4-A1, C3-A2, O2-A1, and O1-A2), electro-oculogram, electromyogram of anterior tibial and chin nerves, and electrocardiogram.
Respiratory movements were assessed through thoracic and abdominal band, and SpO2 by pulse oximetry. An oronasal cannula and thermistor were used to measure nasal airflow, in addition to a microphone placed in the neck to record snoring.
The American Thoracic Society11 provides the following definition and the following criteria for the apnea-hypopnea index (AHI) in children: it corresponds to the sum of the number of obstructive and mixed apneas, and obstructive and mixed hypopneas; it must be expressed in events per hour; to calculate this number, the total sleep time must be used, and it is considered abnormal when AHI ≥ 1 event per hour of sleep. Hypopnea was defined as a reduction > 50% of the flow amplitude associated with a microarousal and/or reduction > 3% of baseline oxygen saturation.
As for the apnea index (AI), the following assumptions were followed: the number of obstructive and mixed apneas (mixed apneas are initially central and can become obstructive at the end of the event), lasting at least two respiratory cycles, which was expressed as events per hour; for the calculation, the total sleep time must be used, and it is considered abnormal when AI ≥ 1 event per hour of sleep. Microarousal was defined as an abrupt change in the electroencephalogram frequency lasting 3 s, preceded by at least 10 s of sleep. Nocturnal desaturation was defined as patients who had more than 30% of total sleep time with peripheral oxygen saturation (SpO2) < 90%.
The project was approved by the research ethics committee of the institution (Protocol 197; Opinion 98/2006). Parents or guardians signed the informed consent after agreeing to participate in the study.
Statistical AnalysisThe SPSS statistical program (released 2012,USA) was used for data tabulation and analysis. Quantitative variables were expressed as mean ± standard deviation or median and interquartile range. Qualitative variables were expressed as absolute and relative frequencies. Student's t-test for independent samples or the Mann-Whitney test was used to compare two means. Spearman's test was used to test the correlation between variables. The level of significance was set at 5% (p < 0.05).
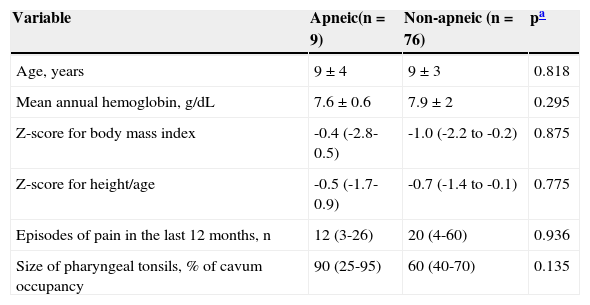
ResultsA total of 85 patients were evaluated, of whom 58.8% were males. Regarding ethnicity, 71.8% self-reported as mixed-race, 20% as black, and 8.2% as white. Table 1 shows the clinical profile of children and adolescents with SCA. There was no statistically significant difference between the mean ages, as it was 9 ± 4 years in the apneic group and 9 ± 3 years in the non-apneic group. The classification of pharyngeal and palatine tonsils in this sample, as well as their frequencies, are described by Salles et al.5
Comparison of clinical data of apneic and non-apneic children and adolescents with sickle-cell anemia.
| Variable | Apneic(n = 9) | Non-apneic (n = 76) | pa |
|---|---|---|---|
| Age, years | 9 ± 4 | 9 ± 3 | 0.818 |
| Mean annual hemoglobin, g/dL | 7.6 ± 0.6 | 7.9 ± 2 | 0.295 |
| Z-score for body mass index | -0.4 (-2.8-0.5) | -1.0 (-2.2 to -0.2) | 0.875 |
| Z-score for height/age | -0.5 (-1.7-0.9) | -0.7 (-1.4 to -0.1) | 0.775 |
| Episodes of pain in the last 12 months, n | 12 (3-26) | 20 (4-60) | 0.936 |
| Size of pharyngeal tonsils, % of cavum occupancy | 90 (25-95) | 60 (40-70) | 0.135 |
Data shown as mean ± standard deviation or median (interquartile range).
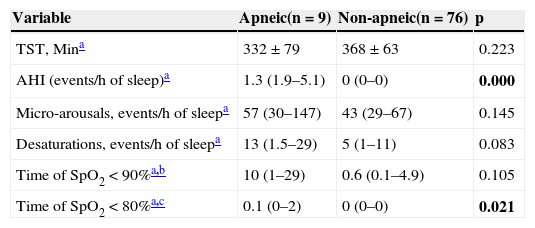
The distribution of polysomnographic data is shown in Table 2. There was no association between OSAS and the variables: ethnicity, gender, age, BMI Z-score, and height/age Z-score.
Comparison of polysomnographic data using quantitative variables of apneic and non-apneic children and adolescents with sickle-cell anemia.
| Variable | Apneic(n = 9) | Non-apneic(n = 76) | p |
|---|---|---|---|
| TST, Mina | 332 ± 79 | 368 ± 63 | 0.223 |
| AHI (events/h of sleep)a | 1.3 (1.9–5.1) | 0 (0–0) | 0.000 |
| Micro-arousals, events/h of sleepa | 57 (30–147) | 43 (29–67) | 0.145 |
| Desaturations, events/h of sleepa | 13 (1.5–29) | 5 (1–11) | 0.083 |
| Time of SpO2 < 90%a,b | 10 (1–29) | 0.6 (0.1–4.9) | 0.105 |
| Time of SpO2 < 80%a,c | 0.1 (0–2) | 0 (0–0) | 0.021 |
Data shown as median (interquartile range).
AHI, apnea-hypopnea index.
Of the 85 patients who were submitted to polysomnography, only nine had AHI ≥ 1 (events per hour of sleep), characterizing OSAS. Nocturnal desaturation was observed in 69 patients (81.2%), as reported in a previous study.12 The number of events per hour of sleep showed a mean of 13, ranging from 1.5 to 29 in the group of patients with apnea, and a mean of five, ranging from one to 11 events per hour of sleep in the non-apneic group.12
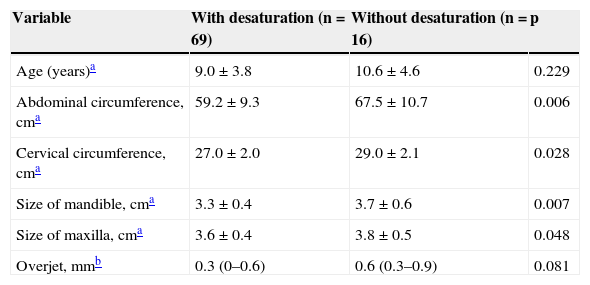
Table 3 shows the association between nocturnal desaturation and CC and AC, as well as maxillary and mandibular measurements.
Comparison of the morphometric variables between children with and without desaturation.
| Variable | With desaturation (n = 69) | Without desaturation (n = 16) | p |
|---|---|---|---|
| Age (years)a | 9.0 ± 3.8 | 10.6 ± 4.6 | 0.229 |
| Abdominal circumference, cma | 59.2 ± 9.3 | 67.5 ± 10.7 | 0.006 |
| Cervical circumference, cma | 27.0 ± 2.0 | 29.0 ± 2.1 | 0.028 |
| Size of mandible, cma | 3.3 ± 0.4 | 3.7 ± 0.6 | 0.007 |
| Size of maxilla, cma | 3.6 ± 0.4 | 3.8 ± 0.5 | 0.048 |
| Overjet, mmb | 0.3 (0–0.6) | 0.6 (0.3–0.9) | 0.081 |
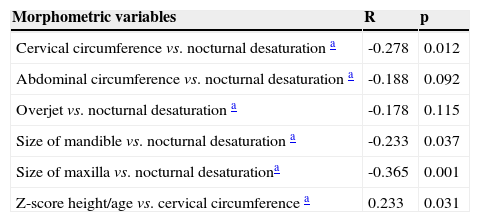
In this sample, measurements of CC and AC, as well as maxillary, mandibular, and overjet measurements were correlated with nocturnal desaturation values obtained during the polysomnography using Spearman's test (Table 4).
Correlation between morphometric variables and nocturnal desaturation in children and adolescents with sickle-cell anemia.
| Morphometric variables | R | p |
|---|---|---|
| Cervical circumference vs. nocturnal desaturation a | -0.278 | 0.012 |
| Abdominal circumference vs. nocturnal desaturation a | -0.188 | 0.092 |
| Overjet vs. nocturnal desaturation a | -0.178 | 0.115 |
| Size of mandible vs. nocturnal desaturation a | -0.233 | 0.037 |
| Size of maxilla vs. nocturnal desaturationa | -0.365 | 0.001 |
| Z-score height/age vs. cervical circumference a | 0.233 | 0.031 |
The positive correlation between height/age Z-score and CC observed in the present study is in agreement with the literature, since studies have demonstrated that sickle-cell anemia patients younger than 18 have height deficit, when compared to normal children;13,14 the growth curve alterations in these children may be associated with UA obstruction and obstructive events during sleep, and, consequently, with the decrease in growth hormone release.15 Bar et al.16 compared the insulin-like growth factor I in children with UA obstruction due to ATH, before and after submitting them to adenotonsillectomy. Prior to surgery, insulin-like growth factor I showed a mean value of 146.3 ng/mL and after surgery, it increased to 210.3 ng/mL (p < 0.01), while the disordered breathing index was within the normal range.
In the present study, nocturnal desaturation in children and adolescents with SCA was associated with CC. One of the key structures for breathing is the laryngeal tract, which is located in the cervical region and, in the child, is shaped like a funnel, narrowing from the vocal folds to the subglottic region.17 As the child grows, there is an expansion of the subglottic area,15 and the thyroid cartilage, which appears adjacent to the hyoid bone at birth, will move away from the latter in the craniocaudal direction.17 Therefore, the younger the age and the lower the height of the child, the smaller the neck circumference, the smaller the airway, and the greater the chance that a child with sickle-cell anemia will have oxyhemoglobin desaturation at night, which, combined with the fact that 55.3% of these children had obstructive ATH,5 contribute to the obstruction of the UAs and corroborate the finding that up to 83% of children with sickle-cell anemia have nocturnal desaturation.18
In this study, obesity was not a contributing factor to airway obstruction. Children and adolescents with sickle-cell disease are not characterized by obesity or overweight; on the contrary, most children were within the normal weight range. The literature has drawn attention to the measurement of CC in children ≥ 29cm at the prepubertal age, which is associated with overweight and obesity.19 The degree of desaturation in an apnea event is known to be correlated with the degree of obesity expressed as BMI.20 As children and adolescents with SCA did not have such characteristics, but showed nocturnal desaturation, there is a clear need to perform future studies with imaging and polysomnography assessment to evaluate the characteristics of the cervical region in this population.
In the present study, children and adolescents with SCA who had nocturnal desaturation also had lower maxillary and mandibular measures, demonstrating a positive correlation between the maxilla and mandible with nocturnal desaturation. It is known that obstructive ATH can alter the oral cavity anatomy and that it is the main cause of UA obstruction in children.21
Studies have demonstrated that at birth, the craniofacial skeleton of a North-American individual corresponds to 60% of the adult head size; at 8 months, it corresponds to 80%; at 3 years, to 90%; and at 9 years, it reaches 95% of the adult size.22 As a consequence, the individual may develop high palate, narrow dental arches, and mandibular retraction. These structures start to occupy the tongue space and force the tongue back toward the posterior oropharynx.23 Moreover, patients with reduced mandibular and maxillary dimensions have a tendency to have UA lumen restriction, as the tongue moves toward the posterior pharyngeal wall, as well as the soft palate and tissues in the oral cavity,24 resulting in the collapse of the UAs when in a state of hypotension of the pharyngeal abductor muscles during sleep, favoring oxyhemoglobin desaturation.24
AC is usually used as an indicator of central obesity, which is typically observed in adults with OSAS.21 However, in this study, children and adolescents with nocturnal desaturation had lower AC measurements. As the evaluated sample was not characterized by obesity or overweight, AC measurement may be influenced by the increased liver and spleen volumes, characteristic of SCA.
It is known that, in patients with SCA, oxyhemoglobin desaturation does not necessarily means hypoxemia, as it may correspond to decreased arterial oxygen content, probably due to the presence of carboxyhemoglobin and methemoglobin, as well as decreased affinity of Hb S for oxygen, even with normal SpO2.25
Although the present study did not aim to evaluate patients with SCA by polysomnography and blood gas analysis, it draws attention to future studies involving this association.
Finally, it was observed that the morphometric variables and CC may contribute to raise the suspicion of nocturnal desaturation in children and adolescents with sickle-cell anemia.
FundingFundação de Amparo à Pesquisa do Estado da Bahia – FAPESB.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Salles C, Bispo M, Trindade-Ramos RT. Association between morphometric variables and nocturnal desaturation in sickle-cell anemia. J Pediatr (Rio J). 2014;90:420–5.