to estimate the prevalence of infection by respiratory viruses in pediatric patients with cancer and acute respiratory infection (ARI) and/or fever.
Methodscross-sectional study, from January 2011 to December 2012. The secretions of nasopharyngeal aspirates were analyzed in children younger than 21 years with acute respiratory infections. Patients were treated at the Grupo em Defesa da Criança Com Câncer (Grendacc) and University Hospital (HU), Jundiaí, SP. The rapid test was used for detection of influenza virus (Kit Biotrin, Inc. Ireland), and real-time multiplex polymerase chain reaction (FTD, Respiratory pathogens, multiplex Fast Trade Kit, Malta) for detection of influenza virus (H1N1, B), rhinovirus, parainfluenza virus, adenovirus, respiratory syncytial virus, human parechovirus, bocavirus, metapneumovirus, and human coronavirus. The prevalence of viral infection was estimated and association tests were used (χ2 or Fisher's exact test).
Results104 samples of nasopharyngeal aspirate and blood were analyzed. The median age was 12 ± 5.2 years, 51% males, 68% whites, 32% had repeated ARIs, 32% prior antibiotic use, 19.8% cough, and 8% contact with ARIs. A total of 94.3% were in good general status. Acute lymphocytic leukemia (42.3%) was the most prevalent neoplasia. Respiratory viruses were detected in 50 samples: rhinoviruses (23.1%), respiratory syncytial virus AB (8.7%), and coronavirus (6.8%). Co-detection occurred in 19% of cases with 2 viruses and in 3% of those with 3 viruses, and was more frequent between rhinovirus and coronavirus 43. Fever in neutropenic patients was observed in 13%, of which four (30.7) were positive for viruses. There were no deaths.
Conclusionsthe prevalence of respiratory viruses was relevant in the infectious episode, with no increase in morbidity and mortality. Viral co-detection was frequent in patients with cancer and ARIs.
estimar a prevalência da infecção pelos vírus respiratórios em pacientes pediátricos com câncer e infecção respiratória aguda (IRA) e/ou febre.
Métodosestudo transversal, de janeiro de 2011 a dezembro de 2012. Foram analisadas secreções de aspirado da nasofaringe de menores de 21 anos, com quadro respiratório agudo, atendidos nos hospitais Grendacc e HU, Jundiaí, SP. Foi aplicado o teste rápido para detecção dos vírus influenza (Kit Biotrin®) e a reação em cadeia da polimerase multiplex em tempo real (Kit multiplex/Fast Trade®) para detecção dos vírus: influenza (A, H1N1, B), rinovírus, parainfluenza, adenovírus respiratório, vírus respiratório sincicial, parechovírus, bocavírus, metapneumovírus humano e coronavírus humano. Foi estimada a prevalência de infecção viral e usados testes de associação (χ2 ou teste exato de Fisher).
Resultadosforam analisadas 104 amostras de aspirado de nasofaringe e sangue. A mediana para a idade foi 12±5,2 anos; masculino (51%); cor branca (68%); IVAS de repetição (32%); uso prévio de antibiótico (32%); tosse (19,8%); e contato com IVAS (8%). Apresentavam-se em bom estado geral 94,3% dos pacientes. A leucemia linfocítica aguda (42,3%) foi mais prevalente. Foram detectados vírus respiratórios em 50% das amostras: rinovírus (23,1%), vírus sincicial respiratório A/B (8,7%) e coronavírus (6,8%). Ocorreu codetecção em 19% entre dois vírus, e de 3% entre três vírus, sendo a mais frequente entre rinovírus e coronavírus 43. Febre em neutropênicos foi de 13%, sendo quatro (30,7%) com vírus positivo. Não houve óbitos.
Conclusõesa prevalência de vírus respiratórios foi importante no episódio infeccioso, sem aumento da morbimortalidade. As codetecções foram frequentes em pacientes com câncer e IRA.
In both developed and developing countries, respiratory diseases contribute to the high proportion of morbidity and mortality in childhood. It is estimated that 25% to 33% of deaths observed in children younger than five years are caused by acute respiratory infections (ARIs) and their complications.1
In Brazil, the expectation of new cases of childhood cancer is 9,300 cases per year in children younger than 15 years. Among these, the most common are acute lymphoblastic leukemia (ALL) and central nervous system (CNS) tumor, followed by Hodgkin's lymphoma (HL) and non-Hodgkin's lymphoma (NHL).2 The very presence of the disease may be a factor of immunosuppression, especially in ALL and lymphomas. Conversely, treatment with chemotherapy interferes with patients’ immune response capacity;3 infection is the most common complication associated with cancer and its treatment, representing the main cause of death rather than the cancer itself.2
Acute viral respiratory infections are the most common causes of febrile episodes in children younger than five years, even in children treated with antineoplastic drugs.4,5
Many studies, concepts, and protocols are well established for the management of fever episodes in children with cancer. However, there are still doubts regarding the true incidence and the role of viral agents in respiratory infections in these patients.6–10 Few studies have been published on this subject in the past; little attention has been given in the literature to new viruses such as human coronavirus (hCoV) and metapneumovirus (hMPV A/B) in immunocompromised pediatric patients.10,11
This study aimed to determine the frequency of infection caused by respiratory viruses in patients younger than 21 years with cancer and acute respiratory infection, and to identify whether there is a subgroup that has severe ARI.
MethodsAn observational, cross-sectional study was performed. Nasopharyngeal aspirate samples from patients younger than 21 years with cancer and fever (measured or reported) and respiratory symptoms of ARI were collected using a standardized protocol. The clinical records were collected from medical records by one of the authors.
Patients were treated in the children's hospital Grendacc (HG) and at Hospital Universitário da Faculdade de Medicina de Jundiaí (HUJ) in the city of Jundiaí, São Paulo, Brazil, both funded by the Brazilian Unified Health System (Sistema Único de Saúde - SUS), from January of 2011 to December of 2012. The HUJ is maternal and child hospital, a regional referral center for eight cities, and offers secondary care to a population of approximately 900,000 inhabitants of Jundiaí and surrounding area. The HG is a day-hospital and referral outpatient clinic that offers assistance for cancer treatment in childhood.
The study was approved by the Research Ethics Committee of the Faculdade de Medicina de Jundiaí (N. 366/2009).
DefinitionsStudy subjects: cancer patients younger than 21 years with acute respiratory infections (ARIs). A new episode of ARI was considered when there was an interval > 15 days during the study period.
ARI: a history of respiratory prodrome, with at least one or more of the following signs or symptoms: fever, coryza, cough, sore throat, and/or gastrointestinal symptoms.
Fever: at least one episode of fever, measured or reported, with axillary temperature > 38°C (based on one measurement) or 37.8°C (based on two measurements with a 1-hour interval).
Hypothermia: temperature < 37.5°C.
Clinical aspects: good overall status, sick, and toxemic.12 Good overall status was defined when the child, at the initial appointment, showed no change in overall appearance and was active, without distress or pain. The patient was considered sick when he/she was irritable, anxious, or had a fatigued or suffering appearance.
Toxemic: patient had difficulty breathing, toxemia, lethargy, or alteration of consciousness.
Anemia: (Hb < 10mg/dL)
Neutropenia (absolute neutrophil count [ANC] <500 cells/mm3.13
Thrombocytopenia: total platelet count < 150.000/uL.13
Suspicion of invasive bacterial infection: in the absence of a negative culture, the following clinical criteria were observed: clinical or laboratory findings of sepsis, or hemodynamically unstable child with poor general status.
Proven invasive bacterial infection: occurrence of bacteremia (one or more positive blood cultures for bacterial pathogen). Sepsis by coagulase-negative Staphylococcus requires two or more positive blood cultures collected on the same day; probable sepsis is indicated if there are two blood cultures for coagulase-negative Staphylococcus within a four-day interval, or three blood cultures within seven days, or four blood cultures within ten days.
Patient selection proceduresThe sample size required for the study (n = 108 episodes of respiratory infection) was based on the estimated prevalence of the studied viruses obtained from the review of several studies (35%), considering a sampling error of 9% in 95% of possible samples.
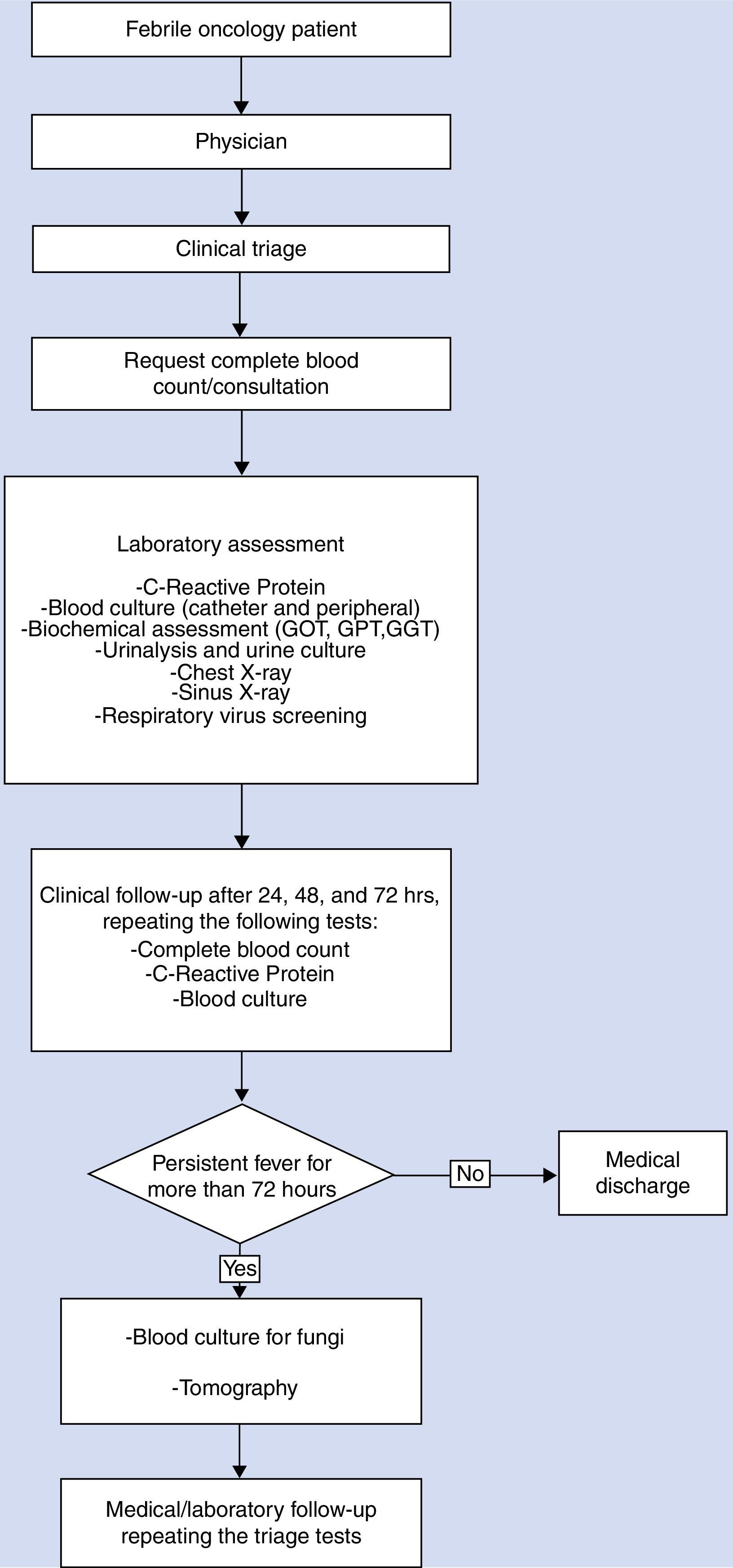
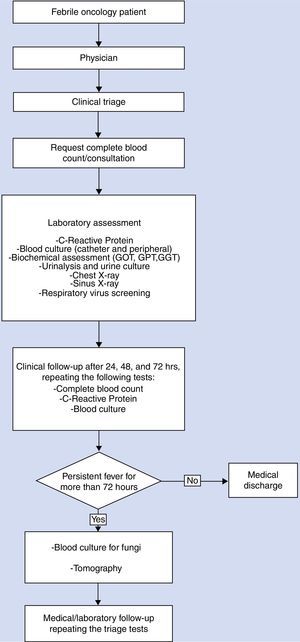
Patients were selected consecutively at the outpatient clinic of HG, from Monday through Friday, from 8:00 AM to 5:00 PM, and from the hospital admission and emergency unit of the Hospital Universitário on the other days and times. Fig. 1 shows the flowchart of patient selection, investigation, and follow-up of patients.
Laboratory investigation for respiratory virus detectionSamples drawn from each nostril aspirate and one from nasopharyngeal swabs were obtained from all patients enrolled in the study, in the supine position with head positioned on the midline. At the time of collection, the sample swab was submitted to the rapid test for detection of influenza A, H1N1, and B (Influenza H1N1 Pandemic test, Bioeasy, Brazil). The result was reported immediately to the physician for treatment decision.
Within a maximum period of 4hours after collection, the samples were mixed and added to a Ringer lactate solution to a total of 4mL. After homogenization, the samples (approximately 1mL) were separated into aliquots in cryotubes, previously identified and stored in liquid nitrogen and stored at -80°C. In the Pediatric Infectious Disease Research Laboratory of the FMJ, the DNA and total RNA nucleic acids were extracted from samples using the extraction Kit (RTP DNA/ RNA Virus Mini Kit, Molecular, STRATEC, Germany).
The sensitivity and specificity were monitored by standard quality control for molecular diagnostics. The qualitative detection of 20 respiratory viruses (influenza [A, H1N1, and B]; coronavirus [NL63, 229E, OC43, and HKU1]; parainfluenza [PIV1, 2, 3, and 4]; rhinovirus [HRV], respiratory syncytial virus [RSV A/B]; human metapneumovirus [hMPV A/B]; adenovirus [ADV]; enterovirus; parechovirus; and bocavirus [hBoV]) was performed by real-time multiplex polymerase chain reaction (FTD - Fast Track Diagnostics - Belgium).
Bacteriological AssessmentAll blood cultures (peripheral and central samples) were performed using the kit BACTEC/Alert (BioMérieux Inc. -United States). Urinalysis and urine culture were obtained on admission, as well as other cultures from different sites, if necessary.
Analysis of peripheral blood was performed by automated hematology analyzer (Sysmex®, Model: KX 21N, USA) within 2hours after collection.
All laboratory investigations strictly followed the manufacturers’ specifications.
Data AnalysisMeasures of central tendency and dispersion were used to describe the study sample. The prevalence of viral infections with their respective 95% confidence interval was estimated. To compare proportions, the chi-squared or Fisher's exact tests were used. The software used was SPSS, release 17 (SPSS - Chicago, IL, United States).
ResultsA total of 48 patients undergoing cancer treatment agreed to participate in the study, totaling 104 episodes with fever and/or respiratory symptoms. The median age was 12 ± 5.1 years, and the youngest patient was 1 year old. The sample consisted of 82 (78.8%) male children; 82 (78.8%) were white, followed by 17 mixed-race (16.7%); and 32 (31%) patients were from the city of Jundiaí.
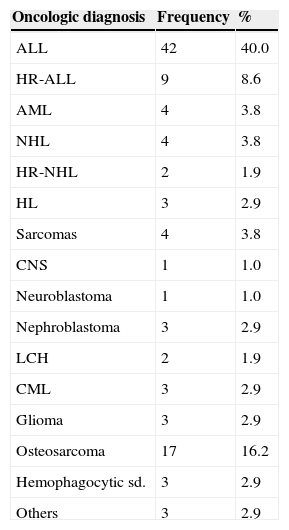
ALL was the most prevalent cancer, identified in 53 patients (51.9%, p = 0.043), and the age range between 5 and 8 years was the most frequent, with 36 patients (34.6%, p = 0.046) (Table 1). Metastatic disease was observed in 23 cases, of which eight (7.7%) had recurrence of the underlying disease.
Total number and percentage of major types of cancer in patients with ARI. Grendacc and HUJ/Department of Pediatrics, Faculdade de Medicina de Jundiaí, 2012.
| Oncologic diagnosis | Frequency | % |
|---|---|---|
| ALL | 42 | 40.0 |
| HR-ALL | 9 | 8.6 |
| AML | 4 | 3.8 |
| NHL | 4 | 3.8 |
| HR-NHL | 2 | 1.9 |
| HL | 3 | 2.9 |
| Sarcomas | 4 | 3.8 |
| CNS | 1 | 1.0 |
| Neuroblastoma | 1 | 1.0 |
| Nephroblastoma | 3 | 2.9 |
| LCH | 2 | 1.9 |
| CML | 3 | 2.9 |
| Glioma | 3 | 2.9 |
| Osteosarcoma | 17 | 16.2 |
| Hemophagocytic sd. | 3 | 2.9 |
| Others | 3 | 2.9 |
ALL, acute lymphoblastic leukemia; HR-ALL, high-risk acute lymphoblastic leukemia; AML, acute myeloid leukemia; NHL, non-Hodgkin lymphoma; HR-NHL, high-risk non-Hodgkin lymphoma; HL, Hodgkin's lymphoma; CNS, central nervous system; LCH, Langerhans cell histiocytosis; CML, chronic myeloid leukemia; sd, syndrome.
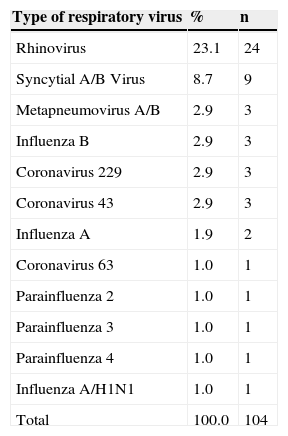
A respiratory viral pathogen was obtained in 50% (52/104) of the analyzed cases for at least one type of respiratory virus. HRV was the most common pathogen, found in 23.1% (24/105) of infectious episodes (Table 2).
Distribution of respiratory virus types in positive cases of patients with ARI. Grendacc and HUJ/Department of Pediatrics of Faculdade de Medicina de Jundiaí, 2012.
| Type of respiratory virus | % | n |
|---|---|---|
| Rhinovirus | 23.1 | 24 |
| Syncytial A/B Virus | 8.7 | 9 |
| Metapneumovirus A/B | 2.9 | 3 |
| Influenza B | 2.9 | 3 |
| Coronavirus 229 | 2.9 | 3 |
| Coronavirus 43 | 2.9 | 3 |
| Influenza A | 1.9 | 2 |
| Coronavirus 63 | 1.0 | 1 |
| Parainfluenza 2 | 1.0 | 1 |
| Parainfluenza 3 | 1.0 | 1 |
| Parainfluenza 4 | 1.0 | 1 |
| Influenza A/H1N1 | 1.0 | 1 |
| Total | 100.0 | 104 |
The analysis of 104 samples by rapid test for IFA (indirect fluorescent antibody), IFAH1N1, and IFB (monoclonal antibody pools, one specific for type A influenza viruses and one specific for type B influenza viruses, are provided for use in IFA assays) resulted in six samples positive for influenza virus (four influenza A and two influenza B).
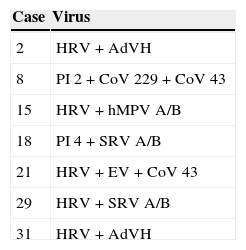
Regarding the number of viruses, 51 cases (49%) had one type. The number of cases of co-detection of respiratory viruses was 17% (18/104) with two, and 3% (3/104) with three; the most frequently observed were rhinovirus and coronavirus 43 (Table 3).
Cases of co-detection of more than one respiratory virus in the same episode.
| Case | Virus |
|---|---|
| 2 | HRV + AdVH |
| 8 | PI 2 + CoV 229 + CoV 43 |
| 15 | HRV + hMPV A/B |
| 18 | PI 4 + SRV A/B |
| 21 | HRV + EV + CoV 43 |
| 29 | HRV + SRV A/B |
| 31 | HRV + AdVH |
HRV, human rhinovirus; AdVH, adenovirus; PI 2, Parainfluenza 2; PI 4, Parainfluenza 4; CoV 229, coronavirus 229; CoV 43, coronavirus 43; EV, enterovirus; SRV A/B, syncytial respiratory virus A/B; hMPV A/B, human metapneumovirus A/B.
The presence of fever and respiratory virus positivity was observed in 17.6% of the episodes (p = 0.332), with at least one peak of fever in 41 (39.4%), and respiratory symptoms in 53 (51%) cases, at the time of the consultation.
Statistical significance was found between the presence of fever and severe neutropenia in the analyzed episodes (p < 0.001).
Among the severe neutropenic cases, 30.7% (4/13) were positive for some type of respiratory virus, two with respiratory syncytial virus A and B, one with coronavirus 229, and one with rhinovirus. However, when considering the mild to moderate neutropenic cases (5.9%), there was no statistical association (p = 0.169). It was observed that the majority of cases had only mild respiratory symptoms, in 38.4% (20/52).
Of the 33 blood cultures collected, three (9.1%) were positive, and the bacterial pathogens associated with febrile episode were: one case of Klebsiella pneumoniae, one case of multi-resistant Klebsiella pneumoniae, and one case of Gram-negative bacilli. Of the 104 episodes studied, empirical antibiotic therapy was case of in 36 (34.2%) cases. Of the patients with respiratory viral infection, none had positive blood or urine culture, and 34.6% (18/52) received antibiotic therapy.
A total of 102 episodes were analyzed regarding the hematological characteristics, with leukopenia observed in 23.5% (24/102) of patients, neutropenia in 20.5% (21/102), and severe neutropenia in 16.7% (17/102), of which 52.9% of patients had ALL. Lymphopenia was present in 41% (42/102) cases. It was also observed that 30.6% (30/102) of patients had anemia and 11.7% (12/102) had thrombocytopenia.
Although it was observed that 99% (103/104) of patients had good general health status, hypothermia was observed in 15% (16/104) and anemia in 43% (44/104) of the sample. Only one individual had a clinical picture of bacteremia; however, no deaths were attributed to the studied episodes.
Regarding the epidemiology of the ARI episode, it was observed that most patients had no previous history of contact with ARIs (8/104). Although not statistically significant (p = 0.282), the correlations between the total number of virus positive patients versus season were 7.7% (8/104) for summer, 18.3% (19/104) for spring, 32.7% (34/104) for winter, and 41.3% (43/104) for fall.
DiscussionMany concepts of viral respiratory diseases in healthy children during infancy have been recently modified.14 In patients with cancer, although studies in the last decade have demonstrated the importance of ARIs,4–6 the actual role of these infections remains unclear.
In this series of respiratory infection and/or fever, a prevalence of respiratory viruses of 50% was observed, showing that these pathogens were the most often detected in ARIs in children undergoing chemotherapy. The findings of this study are consistent with those in the literature, when compared with studies that used the same laboratory method by qPCR technique. Koskenvuo et al.4 documented the presence of respiratory infection in 44% of the cases of children and adolescents with leukemia and fever, and Srinivasan et al.15 observed rates of 75% in their study.
HRV was the most common viral pathogen, followed by coronavirus, RSV, and metapneumovirus, demonstrating the importance of these pathogens in the studied population. Most studies on HRV were performed in immunosuppressed patients after bone marrow or solid organ transplantation, and with human immunodeficiency virus (HIV) carriers.16 Although there is increasing evidence of the possible involvement of this pathogen in lower respiratory tract infections in this group, the pathogenesis remains unclear.
In the present study, the clinical picture was mild; the authors did not observe lower respiratory tract infections in patients affected by this type of virus and the others, although the HRV may remain in the airways of healthy children after resolution of acute symptoms. It has been discussed whether direct viral damage occurs, or if there is a predisposition to secondary invasion with worsening of severity and clinical prognosis.17 Other authors found a higher frequency of respiratory viruses for SRV, HRV, PIV, and ADV, although the clinical aspects have been little explored in publications.4,5 Torres et al. reported the presence of 31% SRV and of 23% HRV, with only episodes of fever and neutropenia.18
It was observed that PIV was present in 3% of episodes, with serotypes 2, 3, and 4 showing similar frequency, contrary to the studies in which PIV-3 has been the most prevalent in immunocompromised children. An emphasis on lower airway infection and increased morbidity and mortality has been attributed to this pathogen in recent years.
Maeng et al.,19 in a retrospective study of 1,554 pediatric patients with cancer, found positive results for 6.4% of cases, and 54% of these had PIV, with mortality of 18.5%, whereas Srinivasan et al.20 verified that complications occurred in lower respiratory tract infection in young children.
The epidemic of influenza A/H1N1 raised new questions about early treatment and time of use of antiviral drugs based on clinical criteria and the presence of risk factors for complications from the disease, such as immunosuppression. In the present series, antiviral drugs were rarely used by pediatric oncologists. This fact might be explained by the lack of previous experience in handling these drugs, by disregarding the importance of this viral pathogen and timely access to the drugs for treatment initiation. The impact of such a measure on viral resistance to drugs in children with cancer remains unknown.
Other relevant aspects, such as the impact of seasonal influenza or its variants in children with cancer are not well understood, as these children can shed the virus for weeks or months.21 In a study involving children with cancer or children undergoing bone marrow transplantation, Tran et al.22 observed infection of the lower airways in 10% of cases of influenza A/H1N1; however, there was no association with increased mortality. Further investigations with children with hematological malignancies have also reinforced this observation, although there was an increase in the number of hospitalizations, chemotherapy delay, and increased antimicrobial use. Deaths were rare in all studies. 23–25
Infection by RSV can cause death in approximately 1.1% of transplanted patients, confirming the impression of worsening of cases in recent years. In the present study, the patients improved, and there were no deaths or complications related to RSV. This can be explained in part by greater involvement of patients at the two-year age range, in which these infections are less severe.
Although human coronavirus (hCoV) is recognized as a common cause of infections of the upper respiratory tract and, to a lesser extent, in the lower tract of immunocompetent patients, its impact is unknown in immunocompromised children.26
No cases of bocavirus were observed, contrary to findings in the literature. This fact might be explained by the non-circulation of this pathogen in the study period, limitations of multiplex molecular identification methods, or characteristics of the study population. The real role of this virus in children with cancer is unknown.
The use of the qPCR technique27 allows for the co-detection of more than one virus in the same sample. However, some questions need further clarification. Does it represent a coinfection, co-detection, or asymptomatic elimination? What is the impact of co-detection on the clinical severity of respiratory disease in patients with cancer?
The co-detection observed in the present study was 17% between HRV and hCoV. Similar rates were observed in studies in children without immunosuppression, 14% to 44%, with HRV being the second or third most frequent virus.14 In children with cancer, Koskenvuo et al.4 found a co-detection rate of 19.7%, especially between HRV and RSV. In the present cohort, co-detection was not associated with case severity, as the initial clinical presentation of patients was mild, most children were initially in good general health status, with rare complications in the lower airways, and there were no deaths. De Paulis et al.28 observed no impact on clinical severity with co-infection in hospitalized infants.
In contrast, other studies also carried out in hospitalized infants without immunosuppression showed that an increase in the number of co-detections may result in increased clinical severity in young children.14 This fact may be attributed to the accidental finding of these viruses in the materials, without important clinical significance in the severity of cancer patients that excrete the virus for long periods.
A viral infection may increase susceptibility to bacterial co-infection. In a multicenter study of children with leukemia and fever, Koskenvuo et al.4 found 13% bacterial sepsis in patients with ARI. In a study of febrile neutropenia, Avadhanula et al.29 found an association with bacterial infection in one-third of cases, suggesting that the RSV infection can increase the expression of receptors for Streptococcus pneumoniae and Haemophilus influenza in primary bronchial epithelial cells, facilitating bacterial colonization and disease.
In the present study, no bacterial complications at clinical examination were observed, with favorable outcome similar to those patients without cancer. The authors emphasize the finding of hypothermia in 15% of children, but without progression to sepsis. Blood cultures were positive in only 9.1% of cases, similar to other studies.18,30
Therefore, the detection of a viral pathogen may provide the physician with a safer therapeutic approach, appropriate antimicrobial use, reducing unnecessary costs imposed on the health system, and providing direct improvement in morbidity and mortality of children with cancer.
Although seasonality for respiratory viruses showed more prevalence in the fall and winter, it was observed that this pattern was not homogeneous for all studied viruses, and a longer period of observation would be necessary to establish a seasonal pattern for this group of children.
Respiratory viruses are pathogens found in most pediatric cancer patients receiving chemotherapy, demonstrating that their presence may be a causative factor for the infectious episode. Their co-detections were frequent in cancer patients with ARI. It was not possible to identify whether the severe acute infection was directly related to the type of cancer or viral pathogen.
FundingProjeto Regular de Pesquisa Fapesp No. 2009/17326-0.
Conflicts of interestThe authors declare no conflicts of interest.
To Fundação de Amparo à Pesquisa do Estado de São Paulo – FAPESP, source of funding for this study, as well as for the implementation of the Laboratory of Molecular Biology of Faculdade de Medicina de Jundiaí.
Please cite this article as: Benites EC, Cabrini DP, Silva AC, Silva JC, Catalan DT, Berezin EN, et al. Acute respiratory viral infections in pediatric cancer patients undergoing chemotherapy. J Pediatr (Rio J). 2014;90:370–6.