To evaluate the accuracy of the simultaneous analysis of three radiographic anatomical landmarks – diaphragm, cardiac silhouette, and vertebral bodies – in determining the position of the umbilical venous catheter distal end using echocardiography as a reference standard.
MethodsThis was a cross-sectional, observational study, with the prospective inclusion of data from all neonates born in a public reference hospital, between April 2012 and September 2013, submitted to umbilical venous catheter insertion as part of their medical care. The position of the catheter distal end, determined by the simultaneous analysis of three radiographic anatomical landmarks, was compared with the anatomical position obtained by echocardiography; sensitivity, specificity, positive predictive value, negative predictive value, and accuracy were calculated.
ResultsOf the 162 newborns assessed by echocardiography, only 44 (27.16%) had the catheter in optimal position, in the thoracic portion of the inferior vena cava or at the junction of the inferior vena cava with the right atrium. The catheters were located in the left atrium and interatrial septum in 54 (33.33%) newborns, in the right atrium in 26 (16.05%), intra-hepatic in 37 (22.84%), and intra-aortic in-one newborn (0.62%). The sensitivity, specificity and accuracy of the radiography to detect the catheter in the target area were 56%, 71%, and 67.28%, respectively.
ConclusionAnteroposterior radiography of the chest alone is not able to safely define the umbilical venous catheter position. Echocardiography allows direct visualization of the catheter tip in relation to vascular structures and, whenever possible, should be considered to identify the location of the umbilical venous catheter.
Avaliar a acurácia da análise simultânea dos três marcos anatômicos radiográficos – diafragma, silhueta cardíaca e corpos vertebrais, na determinação da posição da extremidade distal do cateter venoso umbilical, utilizando ecocardiografia como padrão de referência.
MétodosEstudo transversal, observacional, com inclusão prospectiva de dados de todos os neonatos nascidos em uma maternidade pública de referência, entre abril de 2012 e setembro de 2013, submetidos à inserção de cateter venoso umbilical como parte do atendimento clínico. A posição da extremidade distal do cateter, determinada pela análise simultânea dos três marcos anatômicos radiográficos, foi comparada com a posição anatômica obtida pela ecocardiografia e sensibilidade, especificidade, valor preditivo positivo, valor preditivo negativo e acurácia foram calculados.
ResultadosDos 162 recém-nascidos avaliados por ecocardiografia, somente 44 (27,16%) estavam com o cateter em posição ótima, na porção torácica da veia cava inferior ou na junção da veia cava inferior com o átrio direito. Os cateteres foram localizados no átrio esquerdo e septo interatrial em 54 (33,33%), no átrio direito em 26 (16,05%), intra-hepático em 37 (22,84%) e na aorta em um recém-nascido (0,62%). A sensibilidade, especificidade e acurácia da radiografia para detectar cateter na zona alvo foi de 56%, 71% e 67,28%, respectivamente.
ConclusãoA radiografia anteroposterior de tórax isolada não é capaz de definir com segurança a posição do cateter venoso umbilical. A ecocardiografia permite a visibilização direta da ponta do cateter em relação às estruturas vasculares e, sempre que possível, deve ser considerada para localização do cateter venoso umbilical.
The care of increasingly younger premature infants is a constant challenge for the clinical team. An effective vascular access that is as safe as possible is of utmost importance when caring for these children. The use of the umbilical vein, first reported in 1947 by Diamond,1 constitutes a fast and easy option to obtain access to the systemic circulation.2–6
There are several complications resulting from the use of the umbilical venous catheter (UVC), including cardiac arrhythmia, infection, intracardiac and portal venous system thrombosis, embolism, myocardial perforation, pericardial and pleural effusion, pulmonary infarction and hemorrhage, hepatic erosion and necrosis, and portal hypertension.2,5,7–10 The incidence of reported complications ranges from 20% to 35%, especially if the catheter is poorly positioned,9 as it is essential to ensure the correct positioning of the catheter in the thoracic portion of the inferior vena cava (IVC) or at the junction of the IVC with the right atrium (RA).2,5,7,11–13
The catheter position is routinely assessed by anteroposterior chest radiograph, using the cardiac silhouette, the diaphragm, and the vertebral bodies as anatomical landmarks.2,4,7,9,11–14 The catheter should be at the diaphragm level or slightly above,4 or between the vertebral bodies T8 and T9,12 or at the cavoatrial junction obtained by extrapolating the curve of the RA medial border up to its intersection with the IVC or with the right border of the vertebral bodies.9 However, various studies using imaging methods such as ultrasound and echocardiography to evaluate the UVC position have demonstrated the low accuracy of radiographic anatomical landmarks.2,4,7,9,12,14
It has been observed, when performing echocardiograms and especially in premature infants a significant number of catheters placed in the left atrium (LA), even though they were considered to be in the ideal position at the radiographic analysis. Catheters poorly positioned in the LA, is associated with thrombus formation.7
The aim of this study was to evaluate the accuracy of the anteroposterior chest radiography in determining the UVC position, performing a simultaneous analysis of the catheter projection in relation to the cardiac silhouette, the diaphragm, and the vertebral bodies. The authors also evaluated the performance of the vertebral level method in predicting the UVC position and the association of birth weight and gestational age with catheter positioning. The echocardiographic image was considered as the reference standard, as in previous studies.2,7,14
MethodsThis was a cross-sectional, observational study, with the prospective inclusion of data from all newborns submitted to UVC insertion, regardless of birth weight and gestational age, born in a public reference hospital from April 2012 to September 2013. Newborns with malformations that altered the heart and/or liver position, critically-ill neonates and with no other indication for echocardiography, and those with a chest radiography to be compared with echocardiography with a time interval greater than 36h were excluded from the study. The sample consisted of newborns who met the eligibility criteria during the study period.
The study protocol was approved by the Research Ethics Committee of Fundação Hospitalar do Estado de Minas Gerais, opinion No. 597196-0, CAAE 08220212.7.3001.5119, and subsequently approved by the Research Ethics Committee of Universidade Federal de Minas Gerais, opinion No. 205460, CAAE 08220212.7.0000.5149 to obtain the Master's Degree in Health Sciences. Informed consent was obtained from the parents or legal guardians of all participants.
The variables of interest, namely birth weight, gestational age, gestational age classification in relation to birth weight, clinical diagnosis, and catheter repositioning after chest radiograph analysis were collected from the hospital medical records.
The umbilical catheters were inserted by the medical team according to standard techniques for catheter insertion, using known body references to estimate the length, such as the shoulder-umbilicus length graph and regression equation based on birth weight.2 After insertion, chest radiography in the anteroposterior view was requested and based on the interpretation made by the neonatologist, the UVC was pulled back, when necessary. Repeated radiographic images were obtained every time the catheter position was changed.
After the UVC position was considered appropriate by the neonatologist, a two-dimensional echocardiographic study was performed by one of the researchers, without knowledge of the radiographic assessment of the catheter. The tests were performed using a portable ultrasound device (Logic E, General Electric Healthcare®, USA) equipped with a microconvex transducer of 4–10MHz and the images were obtained in the subcostal, apical four-chamber, and parasternal long- and short-axis views. A small volume of saline solution (0.5mL) was injected through the catheter as contrast medium, to determine the exact position of the tip. The position of the tip was considered adequate if it was identified in the target area – thoracic portion of the IVC or IVC/RA junction – and the UVC was pulled under direct visualization, when echocardiographic assessment showed an intracardiac positioning.
All chest radiographies were analyzed by a radiologist of the institution, who was unaware of the evaluation by the pediatrician and also the location of UVC by the echocardiography. The chest radiographies selected for analysis were those performed at the nearest temporal relation to the echocardiographic study.
Catheter position was simultaneously estimated by analyzing the tip projection in relation to the diaphragm, the vertebral bodies, and the heart silhouette.
The collected data analysis was performed using the program Epi Info 7.1.1.3. (Epi Info, CDC, USA). Initially, a descriptive analysis of data was performed by analyzing measures of central tendency and dispersion of continuous variables.
A comparative analysis of continuous variables, mean gestational age, and mean birth weight with the need for UVC repositioning was performed using analysis of variance (ANOVA), according to Bartlett's test.
The position of the distal end of the UVC, determined by simultaneous analysis of three radiographic anatomical landmarks performed by the radiologist, was compared to the anatomical position obtained by echocardiography. Based on these data, sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and radiographic examination accuracy were calculated.
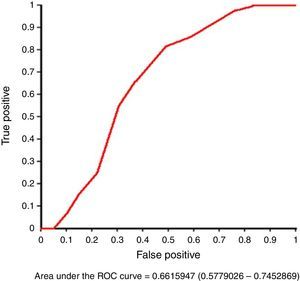
A receiver operating characteristic (ROC) curve was constructed to evaluate the performance of the vertebral level method in predicting the UVC position. The area under the ROC curve with a confidence interval was also determined, using the classification proposed by Hosmer and Lemeshow (2000), in which an area between 0.7 and 0.8 represents an acceptable discriminatory capacity, between 0.8 and 0.9 an excellent discrimination, and above 0.9 an exceptional discrimination.
The statistical significance level was set at p<0.05, with a confidence interval (CI) of 95%.
ResultsOne hundred and sixty-eight venous umbilical catheters were assessed in 167 newborns. Six evaluations were lost due to poor quality of the radiographic examination, preventing adequate analysis. A total of 162 infants were evaluated, with gestational ages ranging from 23 to 41 weeks (32.19±4.23) and birth weight of 405 to 4630g (1809.05±897.46). Most had adequate weight for gestational age (86.42%). The most common clinical diagnoses, which determined their admission to the neonatal intensive care unit, were prematurity (75.93%) and respiratory distress syndrome (12.96%).
The catheters were positioned correctly in the target area in only 44 (27.16%) newborns, as documented by the echocardiography. They were located in the left atrium and interatrial septum in 54 (33.33%) cases, in the RA in 26 (16.05%) cases, intra-hepatic in 37 (22.84%) cases, and intra-aortic in one newborn (0.62%).
The UVC tip identification in the target area by radiographic image, using the three radiographic anatomical landmarks – diaphragm, cardiac silhouette, and vertebral bodies – as reference, had a diagnostic accuracy of 67.28%. Twenty-five of 59 catheters thought to be in the target zone according to the radiographic interpretation were found in the target zone by the echocardiography (PPV of 42.37% for the detection of target area location). Of the 103 catheters interpreted as being outside the target area by the radiograph, 19 were visualized at the target zone on the echocardiography (NPV of 81.55%). This results in a sensitivity of 56% and specificity of 71% for radiographs in the evaluation of UVC target area positioning (Table 1).
Assessment of the anteroposterior chest X-ray capacity in detecting a well-positioned umbilical venous catheter when compared with echocardiography.
| UVC in the target zone by echocardiography | ||||
|---|---|---|---|---|
| YES | NO | |||
| UVC in the target zone by radiographic image | YES | 25 | 34 | 59 |
| NO | 19 | 84 | 103 | |
| 44 | 118 | 162 | ||
UVC, umbilical venous catheter.
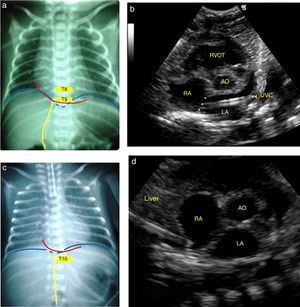
Fig. 1 shows two examples of discordance between assessments of UVC position by anteroposterior chest radiography and the corresponding echocardiographic image. The catheters that were appropriately positioned in the target area were projected into a wide range of vertebral bodies (between T7 and T8 and between T11 and T12), as determined by the echocardiography. The performance of the vertebral level method alone in predicting the UVC position was considered below acceptable, as demonstrated by the area under the ROC curve of 0.66, with 95% CI of 0.57–0.74 (Fig. 2).
Anteroposterior chest X-ray showing the umbilical venous catheter in T9, just above the diaphragm and cavoatrial junction, interpreted as well positioned (a) and corresponding echocardiographic image (b) demonstrating the distal end of the catheter in the left atrium, after crossing the interatrial septum (*). In another newborn, the radiographic image showed the catheter between T9 and T10, below the diaphragm and cavoatrial junction, suggesting it is positioned in the liver (c), but its end was correctly identified in the inferior vena cava junction with the right atrium by the echocardiography (d). LA, left atrium; RA, right atrium; AO aorta; UVC, umbilical venous catheter; RVOT, right ventricular outflow tract.
Sixty-eight (41.98%) catheters, considered to be intracardiac, were pulled back by neonatologists before the echocardiography was performed, requiring more than one radiographic image. Of these 68 pulled catheters, 14 (20.59%) were visualized in the liver through the echocardiography and were removed. A lower mean gestational age (30.77±4.38 vs. 33.21±3.82 weeks, p<0.01, ANOVA) and a lower mean birth weight (1566.29±924.73 vs. 1984.67±839.06g, p<0.01, ANOVA) were statistically significant risk factors for poor UVC positioning, after a preliminary assessment of the chest radiography.
Although saline contrast was injected into all catheters, it was useful in only 56 (34.57%) cases to determine the exact position of the tip, more often when the tip was in the ductus venosus or hepatic vessels (36 patients). In the other cases, the echocardiographic image alone was enough to clearly identify the catheter location.
The mean time interval between the radiographic and echocardiographic studies was 14h (ranging from 5min to 31h).
DiscussionRadiographic control for UVC position assessment was introduced by Peck and Lowman15 in 1967, and the technique remains the most often used.2,4,9,11,16 After the 1980s, various studies that evaluated the catheter by ultrasonography5,9,12,17 or echocardiography2,4,7,14 showed that the chest anteroposterior radiography alone is not capable of ensuring a reliable UVC positioning.
In 1995, Greenberg et al.12 demonstrated that 90% of catheters positioned between T8 and T9 and 100% of those at T9 were correctly positioned in the IVC/RA junction. However, other studies have identified a poor correlation between the thoracic level and echocardiographic or ultrasonographic location.2,9,13 Catheters that are well-positioned in the target area may be located in a wide range of vertebral bodies, from T6 to T112 or even at T4.13 The present study also showed a lower capacity of the vertebral body method to differentiate between well-positioned catheters and poorly positioned ones (area under the ROC curve of 0.66).
According to the case-control study carried out by Raval et al.,7 the detection of a poorly positioned UVC in the left atrium through a radiograph showed a sensitivity, specificity, and accuracy of 45%, 87%, and 66%, respectively. These findings are similar to those found by Ades et al.2 (32%, 89%, and 63%, respectively). Michel et al.13 evaluated the radiography capacity to determine the adequate positioning of the UVC and concluded that it was inefficient in determining the catheter tip position (sensitivity 66% and specificity 63%). In the present study, the radiography accuracy in detecting a well-positioned catheter was 67%, i.e., the method was not able to identify malposition at approximately 33% of the time.
In 2014, Hoellering et al.9 recommended that, if the assessment of the UVC by ultrasonography is not available, the position should be determined by the cardiac silhouette method. This method, unlike the vertebral body method, was able to accurately predict catheter position; however, it was located in the target area in only 35 (18%) of 200 assessments. In this study, the catheters were found adequately positioned in the target area in 27% of the assessments, as documented by echocardiography, even when simultaneously analyzing the vertebral body, cardiac silhouette, and diaphragm methods.
A high need for UVC repositioning after radiographic control was identified (41.98%), significantly higher in newborns with lower mean gestational age and lower mean birth weight, similar to the findings of Harabor and Soraisham.16 Michel et al.13 found an accuracy of the chest radiography to define UVC position that was significantly higher in newborns with low birth weight. However, the study was carried out with a different reference standard (joint interpretation of the results of radiography and ultrasonography), which does not allow for an adequate comparative analysis with the present study.
Catheters identified by radiographic assessment as intracardiac may be in the appropriate position, as suggested by Ades et al.2 If unnecessarily pulled back, they will be displaced into the liver, as documented by echocardiography in 14 (20%) assessed infants. This resulted in loss of venous access, increased patient handling, and exposure to radiation. Fleming described the same: “Every catheter manipulation has a risk of vessel trauma, infection, or thrombosis”.17
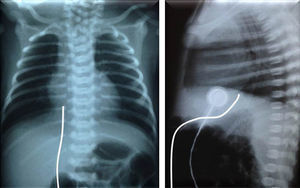
In 1969, Baker et al.18 were the first to emphasize the importance of using lateral radiographic projections. The last portion of the ductus venosus runs in the sagittal plane and, therefore, it is only correctly visualized in a lateral projection, and poor positioning can be easily identified.5,11,19,20 The UVC appears in the frontal projection as a straight line or slightly curved to the right; at the lateral projection, it is seen anteriorly crossing the liver and as an S-shaped curve before it reaches the heart5,18–23 (Fig. 3). The lateral projection increases the chest radiography accuracy in predicting the UVC location; on the other hand, it results in greater exposure of the newborn to radiation.
The radiographic image formation is also a limiting factor of the chest radiography performance and, similarly to the duct anatomical position, it is not amenable to correction. The catheter image projected on different anatomical landmarks undergoes changes according to the degree of image distortion, lung aeration, and the newborn's position.24,25 As the catheter is inserted into the umbilical vein and blindly advanced to the predetermined length, the alignment and correct use of the central radius cannot be guaranteed. Given the short length of the target area9 and the children's small sizes, particularly those who require umbilical access, a small rotation or inclination and catheter exposure to the diverging radiuses may result in images with significantly different findings, which do not accurately reflect their position.
During a UVC study using ultrasonography, Fleming and Kim17 observed a mean of catheter migration to the heart of 5.4mm (max 18mm) with lower-limb movement. This distance becomes very relevant when considering the target zone length of 4–11mm (median 6mm), according to the study by Hoellering et al.,9 and may explain the low accuracy of the anteroposterior chest radiograph.
During repositioning under direct visualization of poorly positioned catheters, it was observed with interest that simply removing the fixing bandage was sometimes enough to place it in an acceptable position. That is, a simple pressure on the fixing bandage can lead to an inadvertently deeper catheter positioning.
After the UVC insertion, it is important to ensure its correct positioning in order to prevent potentially fatal complications. Complications were not systematically assessed in this study. However, three cases of thrombus were identified, two intracardiac and one at the IVC/RA junction, two liver lacerations with fluid overflow into the hepatic parenchyma, and two pericardial effusions. The lesions spontaneously regressed after the UVC withdrawal, except for one intracardiac thrombus that showed progressive increase in size, for which the child was treated with enoxaparin.
The major limitation of this study was the mean time of 14h (range 5min to 31h) between the radiography and the echocardiography, which cannot guarantee the constancy of catheter positioning. Hoellering et al.9 described that catheter migration after a few hours is not unusual in clinical practice, but the displacement is verified through serial chest radiographies. However, radiographic images obtained with different exposure settings and with the patient in different positions may result in catheter tip projections at different locations. During this study, the authors re-evaluated three infants with suspected catheter migration, which was not confirmed by echocardiography. Therefore, to quantitate the degree of UVC migration, it would be necessary to carry out prospective studies using imaging methods that allow a direct visualization of the tip, such as ultrasound or echocardiography.
The authors conclude that the anteroposterior chest radiography, a method routinely used to assess catheter positioning, is not reliable in identifying the exact anatomical location of the distal end of the UVC. Echocardiography allows direct visualization of the catheter tip in relation to vascular structures, reduces handling of the newborn and exposure of the newborn and medical staff to radiation and, more importantly, prevents the complications associated with a poorly-positioned catheter, and should therefore be considered as a reference standard for location of the UVC. After a training protocol in echocardiography or functional ultrasound, insertion of the UVC with direct visualization is more adequate and can be performed by the neonatologist in charge of the procedure.4
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Guimarães AF, Souza AA, Bouzada MC, Meira ZM. Accuracy of chest radiography for positioning of the umbilical venous catheter. J Pediatr (Rio J). 2017;93:172–8.
Study conducted at the Postgraduate Program in Health Sciences, Child and Adolescent Health Area, Faculdade de Medicina, Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brazil.
Part of Adriana Furletti Machado Guimarães’ Master's Degree Dissertation.