To analyze access to surgical care for congenital heart diseases in public specialized centers in the state of São Paulo before and during the COVID-19 pandemic and availability of surgical care in specialized hospitals, to identify bottlenecks in the care path for neonatal cardiac surgery.
MethodsThis study included 1,437 children, under one year old, with congenital heart disease and formal referral to heart surgery between February 1, 2019, and February 28, 2021. Quantitative data analysis was performed using t-tests or the Mann-Whitney test.
ResultsApproximately 30 % of children with urgent congenital heart disease could not access recommended care, mainly those needing complex surgeries (categories RACHS 4 to 6). The main diagnoses of neonates accessing care were patency of the ductus arteriosus (10.5 %) and coarctation of the aorta (10.1 %). Referral time for children in RACHS 1 to 3 was 4 days (median), while for those in categories 4 to 6, it was 7 days (p < 0.001). Longer referral time (20 days) was associated with court orders. During the pandemic, referral time decreased to 3 days, compared to 5 days (median) in the pre-pandemic period (p < 0.001).
ConclusionThe emergency surgical treatment supply for congenital heart diseases is insufficient compared to the current demand. Future research should evaluate if access to care in publicly funded hospitals could be improved by better access to prenatal care for pregnant women, increased diagnostic and therapeutic capacity in pediatric cardiology, and financial incentives for complex cardiac surgeries.
Brazil records approximately 2.8 million live births per year, and almost 29,000 new cases per year of congenital heart disease. The incidence of this condition is estimated at around 1 %, in Brazil as well as in other Latin American countries.1 Even though the Millennium Development Goal - infant mortality reduction – was achieved in the year of 2015, national infant mortality rates remain relatively high.2 The neonatal infant mortality accounts for approximately 52 % of deaths,3 of which 25 % occur in the first 24 hours after delivery.4
Early diagnosis of congenital heart disease is essential for treatment and includes the use of diagnostic techniques during prenatal care and clinical examination of the newborn. Fetal echocardiography is a valuable prenatal diagnostic tool for heart disease, but there is still no clear evidence in the literature in favor of its use in low-risk pregnant women. The morphological ultrasound performed by the obstetrician has an estimated sensitivity of 43 % for detecting congenital heart disease. Early diagnosis in prenatal care allows for better care and treatment outcomes.4
The “pulse oximetry screening” is the recommended neonatal screening tool post-delivery, and it consists of measuring the peripheral oxygen saturation in the limbs.5 The negative predictive value of this test for severe cardiomyopathy is 99 %. If the test is positive, an echocardiogram is recommended before hospital discharge and approximately 25 % of children with a positive test do not have heart disease.4 It is worth noting that a few heart diseases, such as coarctation of the aorta, might not be diagnosed by the “pulse oximetry screening”, which in turn results in a diagnostic delay and increased chances of complications. Postnatal echocardiography in children is the gold standard diagnostic method for congenital heart disease.6
One of the issues experienced in the Unified Health System (SUS) is the lack of investment in infrastructure and in maintaining health professionals, evidenced by the low rates of detection of congenital heart diseases in prenatal care and delays in diagnosis. Postnatal echocardiography is not easily accessible, and this is made worse by regional inequalities.6 Fetal echocardiography is far from reality in the public healthcare sector;7 even those patients with a prenatal diagnosis of heart disease might not have access to the corresponding specialized care and surgery, due to lack of capacity.4
The development of a safe congenital cardiac care system includes a well-defined and structured care pathway, as well as the corresponding funding for these services.8 Currently, complex procedures do not receive special funding in the public sector, which leads to a low capacity to perform neonatal surgical procedures for heart diseases.9 A 2010 study estimated that 54 % of children under 1 year of age do not have access to cardiac surgery through the public healthcare system in the state of São Paulo.1
In the State of São Paulo, every child with congenital heart disease that requires a surgical procedure in the public sector is registered with CROSS (Central de Regulação de Ofertas e Serviços de Saúde), created in 2010, it regulates access to publicly funded hospitals and outpatient services in the State.10 Regulatory processes aim to increase efficiency and effectiveness in the use of resources in the emergency pediatric care system.
The congenital cardiac care pathway has faced major challenges because of the COVID-19 pandemic, such as a reduced number of health professionals and the reallocation of resources to boost the pandemic effort.11 The availability of operating rooms and intensive care unit beds was reduced, as well as the number of elective pediatric and neonatal cardiac surgical procedures. It is worth noting that urgent cases, defined as those that cannot be postponed for more than a month, continued to receive care in almost all health services.12
The objective of this study was to analyze the access to surgical care for congenital heart diseases in specialized centers in the public sector of the state of São Paulo before and during the COVID-19 pandemic. The specific objectives were the description of congenital heart pathologies in this population; analysis of the availability of surgical care in specialized hospitals; and the identification of possible bottlenecks in the emergency neonatal pediatric cardiac surgery care pathway.
MethodologyThis retrospective cohort study included data from 1,437 children, younger than one year of age, diagnosed with congenital heart disease and with a referral to heart surgery, registered with CROSS in the period from February 1, 2019 to February 28, 2021. Children whose reason for referral was clinical treatment only were excluded.
The 7 independent variables analyzed were gender, place of origin, referral hospital, main diagnosis, other diagnoses, presence or absence of a court order, and child's ordinal classification on the RACHS surgical risk adjustment scale. The dependent variable was the time since referral, i.e., from registration with CROSS to transfer to hospital or end of care. The date considered as the start of the COVID-19 pandemic was March 17, 2020. Quantitative data analysis was performed using t-tests or the Mann-Whitney test. The normality test was based on the Kolmogorov-Smirnov test. For the statistical tests, a significance level of 5 % was adopted. The calculations presented were performed using the R 4.0.5 software.13
This research was reviewed and approved by the Research Ethics Committee of the Instituto de Ensino e Pesquisa Armenio Crestana (IEPAC) from Serviço Social da Construção Civil do Estado de São Paulo, CAAE 42691521.3.0000.0083 and opinion number PlatBr: 4.578.062, in accordance with the norms of Resolution 466/12 of the Brazilian National Health Council.
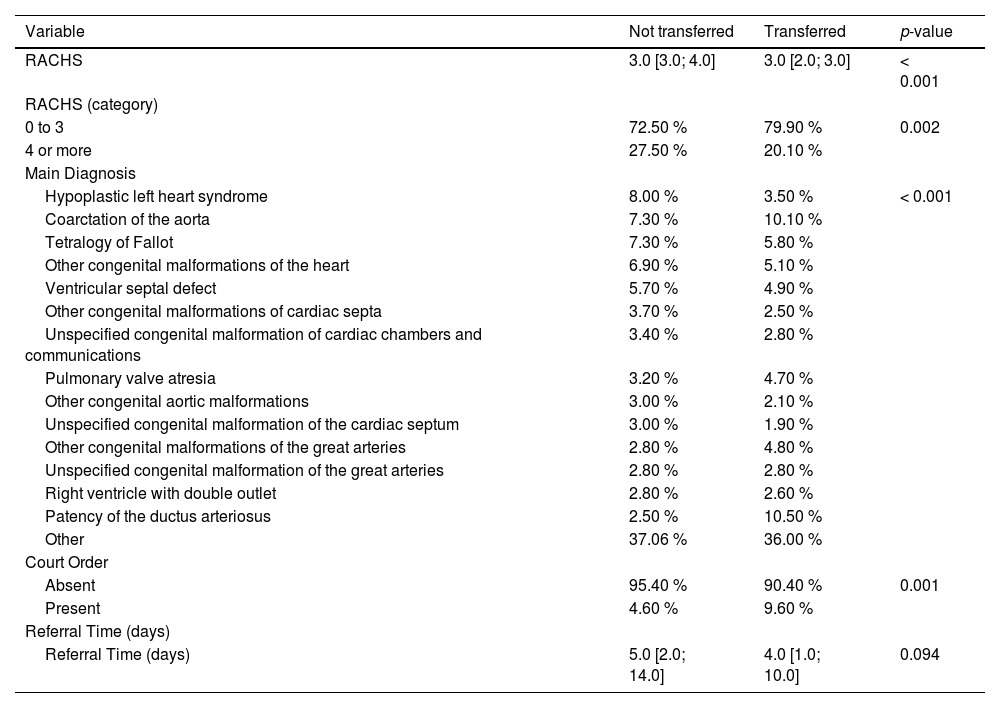
ResultsApproximately 30 % of children with urgent congenital heart disease registered with CROSS could not be transferred. The comparison of not transferred vs. transferred children (Table 1) shows that there is a difference between groups by RACHS category (p < 0.001). Categories RACHS 4 to 6, indicating more complex surgeries, are associated with a higher number of transfer failures. Failure to transfer to a hospital means that the child did not have access to surgical treatment and most likely died.
Comparative analysis of newborns referred to treatment of congenital heart diseases in the period from February 01, 2019 to February 28, 2021 (RACHS, ICD, Court Order and Time since Request).
In São Paulo, only six publicly funded healthcare services are able to perform complex cardiac pediatric surgeries. The main diagnosis (Table 1) corroborates the analysis by RACHS category, showing a difference in the frequency of diagnosis between groups (p < 0.001). In the not transferred group, the most frequent conditions were: hypoplastic left heart syndrome (8 %), coarctation of the aorta (7.3 %) and tetralogy of Fallot (7.3 %). Among those transferred, the most frequent were patency of the ductus arteriosus (10.5 %) and coarctation of the aorta (10.1 %). Coarctation of the aorta has a high incidence in both groups. Although this diagnosis is classified in category 1 of the RACHS scale, for simpler surgical correction, children who have a delayed closure of the ductus arteriosus may have late clinical repercussions of this disease, delaying the diagnosis and consequently delaying appropriate care. Statistical significance was verified in the analysis of the child's main and secondary diagnoses. The main and secondary diagnoses associated with longer referral time were hypoplastic left heart syndrome (13 days) double-outlet right ventricle (8.5 days) and pulmonary atresia (17 days).
In the analysis of court orders, the longest time since referral is associated with the presence of a court order (median of 20 days), while the absence of it is related to the median of 4 days. The study design does not allow the determination of the direction of this association, as the request for a court order could be both a result of the delay in referral for surgical treatment or the cause for such delay. The referral of children categorized in RACHS 1 to 3 took a median of 4 days, while those in categories 4 to 6 took 7 days (p < 0.001), once again demonstrating the interaction with the variable surgical risk/complexity.
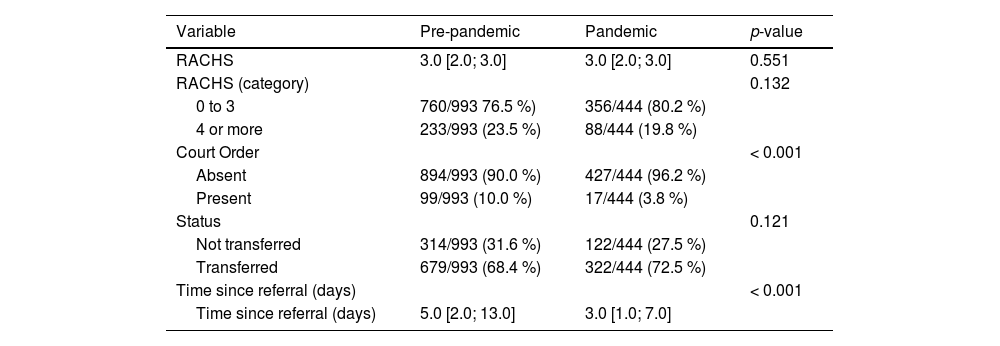
Comparisons between the pre-pandemic and during the pandemic periods are shown in Table 2. The referral time decreased during the pandemic, going down from 5 days (median) in the pre-pandemic period to 3 days during the pandemic (p < 0.001).
Comparative analysis of access to surgical treatment for congenital heart disease during pre-pandemic and pandemic periods.
This data suggests that the current supply of surgical procedures is insufficient, evidenced both by the number of children who do not receive treatment and by the number of interventions by the justice system in health care. Therefore, access to complex surgical treatment for heart conditions such as pulmonary atresia and hypoplastic left heart syndrome should be expanded. The prioritization of severely ill patients on the “waiting list” can increase the efficiency of the system, but this has proven to be a palliative measure in a healthcare system with a historical lack of access to life-saving procedures.
The stubbornly high frequency of patients with coarctation of the aorta among those who could not be referred is a reminder of the need for better prenatal care, improved diagnostic capacity, and clear evidence-based criteria for the indication of fetal echocardiography.
Due to the COVID-19 pandemic, children in the public sector with a referral to urgent cardiac surgery had a shorter waiting time compared to the pre-pandemic period. This seems counterintuitive but it can probably be attributed to increased capacity due to the cancellation of elective surgeries. Yet, another evidence in favor of the need for more capacity for surgical treatment of congenital heart diseases.
In conclusion, the supply of emergency surgical treatment for congenital heart diseases is insufficient compared to the current demand. Due to study design limitations, it is not possible to evaluate the causes of poor access to care, the authors suggest future research should evaluate if access to care in publicly funded hospitals could be improved by better access to prenatal care for pregnant women, increased diagnostic and therapeutic capacity in pediatric cardiology, and financial incentives for complex cardiac surgeries.
Authors’ contributionsMaira Marasca de Oliveira: Conceptualization, data curation, formal analysis, investigation, methodology, project administration, resources, software, visualization, original draft, review and editing.
Gonzalo Vecina Neto: Conceptualization, data curation, formal analysis, investigation, methodology, project administration, supervision, validation, visualization, original draft.
Ana Maria Malik: Formal analysis, project administration, resources, supervision, validation, visualization, original draft, review and editing.
Reinaldo Sérgio Hamamoto: Formal analysis, project administration, supervision, validation, visualization, original draft, review and editing.
Funding sourceNo financiers.
Educational Institution: Fundação Getúlio Vargas - Escola de Administração de Empresas de São Paulo – FGV EAESP.