To map available scientific evidence about the pediatric population with spina bifida submitted to transanal irrigation to manage signs and symptoms of neurogenic bowel.
Source of dataThis research was developed according to recommendations from the Joanna Briggs Institute Reviewers' Manual and the PRISMA Extension for Scoping Reviews. Searches were carried out in the databases: CINAHL, Medline/Pubmed, Scielo, Scopus, Web of Science, Embase, LILACS, Proquest, and the CAPES catalog of theses and dissertations. Quantitative and qualitative studies on the topic were included, as long as they dealt with this population. There was no predetermined time frame.
Summary of the findingsThe authors found 1.020 studies, selected 130 for close reading, and included 23 in the review, all of which had been published from 1989 to 2021. The authors mapped the characteristics of the studies, including their definitions of concepts and use of scales, criteria for the indication of transanal irrigation, training to carry out the procedure, devices and solutions used, number and frequency of transanal irrigations, health care actions, time spent, associated complications, complementary exams, adherence rate, follow-up, and outcomes, focusing on the benefits for bowel management.
ConclusionsDespite the variability of evaluation parameters and term definitions, evidence suggests that transanal irrigation is a safe and effective method to manage fecal incontinence. Studies in the field are likely to grow, using standardized scales and longitudinal follow-ups. The authors suggest further research on transanal irrigation in the pediatric population with spina bifida in the Latin American context.
Spina bifida (SB) is the most common non-lethal congenital malformation. It results from a defect in the closure of the neural tube during embryogenesis and has a multifactorial etiology.1-3 It is associated with conditions such as hydrocephaly and encephalic malformations, as well as with varying degrees of cognitive deficit and muscle weakness in lower limbs, orthopedic deformities, sensory alterations, and bladder and bowel dysfunctions.1-3 The incidence of SB in the world varies from <1 to 7 per 1,000 children born alive.3 In Brazil, from 2014 to 2018, its incidence was 0.7 for each 1,000 born alive.4
Neurogenic bowel, present in most individuals with SB,5 is characterized by slow colonic transit, rectal tone alteration, reduced elimination sensitivity, and compromised functioning of internal and external anal sphincters.5,6 These alterations culminate in constipation for approximately 85% of individuals and fecal incontinence (FI) for about 70%.5 These issues affect their health, and daily life activities, and prejudice the quality of life of individuals and their families.5-8
Considering this challenging condition, bowel retraining is a tool to regularly evacuate the bowels, promoting social fecal continence and guaranteeing independence in bowel management.5,6,9 Proactive and systematic approaches can lead to more functional lifestyles, and advances in treatment should start with less invasive strategies, only then progressing to more invasive ones, adapting them to the physical and cognitive strengths of the individual and to their family context.6,7,10,11
Studies warn about the challenge that is managing neurogenic bowel and, especially, FI.5,6,10 Early strategies of bowel management often fail, not to mention how time-consuming they are.7,12 In this context, research has highlighted the role of transanal irrigation (TAI) as a practice to achieve social fecal continence, reducing the time spent in bowel management and favoring autonomy and independence in self-care.9-11,13-15
The TAI, also called retrograde irrigation, is the administration of a large volume of water or saline into the rectum and colon using a catheter, often equipped with a pump or a cone and inserted through the anus, in order to completely evacuate feces from the bowel, thus allowing for programmed and regular eliminations.10,11,14,16,17 This method was cited in the 1980s as a possible tool to improve FI in children and adolescents with SB. One of the studies developed a special catheter for continence enemas (ECC; Cardiomed Supplies, Gormley, Ontário), for which, at first, a blood catheter with an inflatable pump was commonly used,18 in addition, there was the Willis system, which used a transanal irrigation cone.19
The goal of this study is to map available scientific evidence about the pediatric population with SB submitted to TAI, in order to manage signs and symptoms of neurogenic bowel.
MethodsThis is a scoping review whose goal is to map the extension and nature of evidence related to the use of TAI in the management of pathogenic bowel disorders in the pediatric population with SB. The guiding question of this research was: What is the evidence available about TAI or retrograde irrigation in the management of neurogenic bowel secondary to SB in the pediatric population?
This research was carried out according to recommendations from the Joanna Briggs Institute Reviewers’ Manual and the PRISMA Extension for Scoping Reviews.20 A preliminary search in MEDLINE and the Cochrane Database of Systematic Reviews was carried out, but no systematic or scoping reviews on the topic were found. The research protocol was registered at the OSF (https://osf.io/sx7fj/).
The authors used the PCC strategy, in which: Participants= children and adolescents with SB; Concept= transanal irrigation and retrograde irrigation; Context= management of neurogenic bowel dysfunctions, especially FI.
The authors considered children up to 12 years and adolescents up to 19 years, according to the definition provided by the Brazilian Ministry of Health and in accordance with the World Health Organization.21
The databases used in April 2022 were: Cumulative Index to Nursing and Allied Health Literature (CINAHL), Literatura Latino-Americana em Ciências de Saúde (LILACS), SciVerse Scopus, National Library of Medicine (PubMed/ MedLine), Web of Science, Scientific Electronic Library Online (SciELO), Embase, ProQuest, and the CAPES Catalog of Theses and Dissertations. The descriptors and related terms used were: spina bifida, dysraphism spinal, neurogenic bowel; meningomyelocele; fecal incontinence; constipation; bowel management; enema; transanal irrigation; children; adolescent, infant. They were crossed using the boolean operators “AND” and “OR”. As an example, the strategy used for the search in PubMed/MedLine was (“neurogenic bowel” OR “fecal incontinence” OR constipation) AND (enema OR "transanal irrigation" OR "enema kit") AND (pediatric OR child OR infant OR adolescent OR children) AND ("spina bifida" OR “spinal dysraphism” OR meningomyelocele).
The triage and selection of studies were carried out by two independent blinded researchers and were based on the information available in the titles and abstracts. The Rayyan software was used to store and organize the triage.22 In case of conflict, the decision was based on a consensus between the researchers and a third reviewer. The authors included complete publications, original studies, literature revisions, specialist consensus, theses and dissertations, and letters to the editor that addressed the use of TAI in the management of neurogenic bowel in children and adolescents with SB. The authors excluded publications in books or congress abstracts, as well as studies whose approach was associated with anterograde irrigation and surgeries.
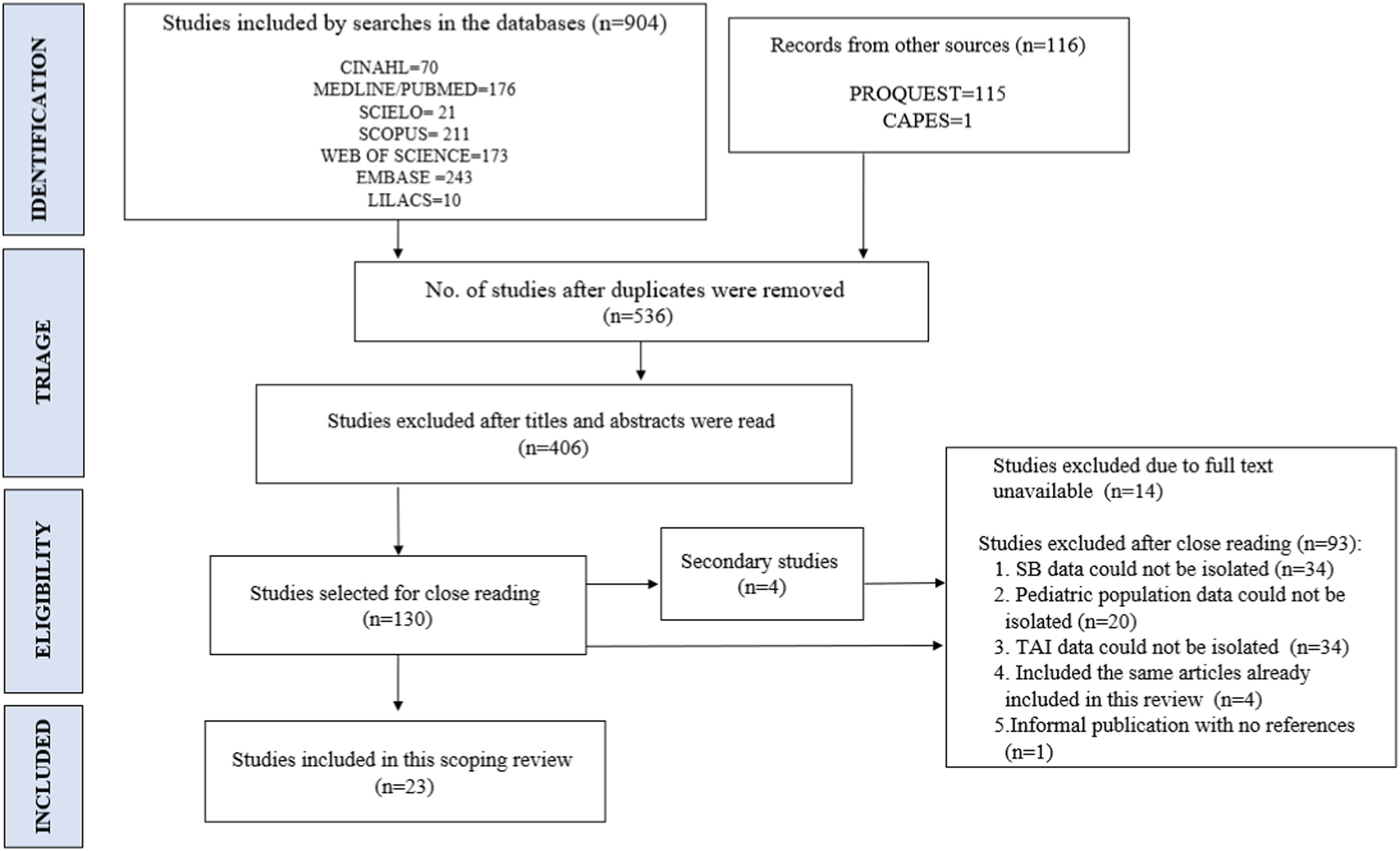
OutcomesThe authors found 904 articles in the databases and 116 from other sources (n = 1020). 484 articles were duplicates and 406 were not in accordance with the inclusion criteria after a reading of the titles and abstracts. They were excluded as a result. 130 studies were selected for close reading, 107 of which were excluded, as they did not meet inclusion criteria. As a result, 23 studies were included in this scoping review (Figure 1).
Article selection flowchart. Source: Elaborated by the authors according with the PRISMA flowchart.20
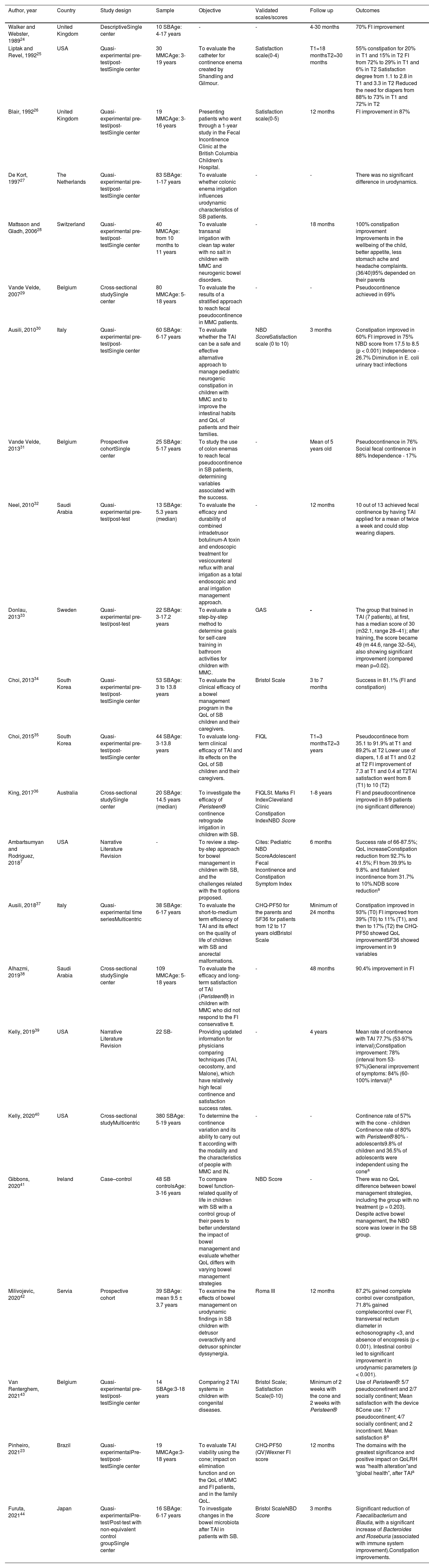
The characteristics of the studies, including their clinical outcomes, follow-up, and clinical evaluations, are described in Table 1. 22 studies selected were articles published in scientific journals, while 1 was an MS dissertation.23-44
Study characterization, scales used, follow up, and main results.
| Author, year | Country | Study design | Sample | Objective | Validated scales/scores | Follow up | Outcomes |
|---|---|---|---|---|---|---|---|
| Walker and Webster, 198924 | United Kingdom | DescriptiveSingle center | 10 SBAge: 4-17 years | - | - | 4-30 months | 70% FI improvement |
| Liptak and Revel, 199225 | USA | Quasi-experimental pre-test/post-testSingle center | 30 MMCAge: 3-19 years | To evaluate the catheter for continence enema created by Shandling and Gilmour. | Satisfaction scale(0-4) | T1=18 monthsT2=30 months | 55% constipation for 20% in T1 and 15% in T2 FI from 72% to 29% in T1 and 6% in T2 Satisfaction degree from 1.1 to 2.8 in T1 and 3.3 in T2 Reduced the need for diapers from 88% to 73% in T1 and 72% in T2 |
| Blair, 199226 | United Kingdom | Quasi-experimental pre-test/post-testSingle center | 19 MMCAge: 3-16 years | Presenting patients who went through a 1-year study in the Fecal Incontinence Clinic at the British Columbia Children's Hospital. | Satisfaction scale(0-5) | 12 months | FI improvement in 87% |
| De Kort, 199727 | The Netherlands | Quasi-experimental pre-test/post-testSingle center | 83 SBAge: 1-17 years | To evaluate whether colonic enema irrigation influences urodynamic characteristics of SB patients. | - | - | There was no significant difference in urodynamics. |
| Mattsson and Gladh, 200628 | Switzerland | Quasi-experimental pre-test/post-testSingle center | 40 MMCAge: from 10 months to 11 years | To evaluate transanal irrigation with clean tap water with no salt in children with MMC and neurogenic bowel disorders. | - | 18 months | 100% constipation improvement Improvements in the wellbeing of the child, better appetite, less stomach ache and headache complaints. (36/40)95% depended on their parents |
| Vande Velde, 200729 | Belgium | Cross-sectional studySingle center | 80 MMCAge: 5-18 years | To evaluate the results of a stratified approach to reach fecal pseudocontinence in MMC patients. | - | - | Pseudocontinence achieved in 69% |
| Ausili, 201030 | Italy | Quasi-experimental pre-test/post-testSingle center | 60 SBAge: 6-17 years | To evaluate whether the TAI can be a safe and effective alternative approach to manage pediatric neurogenic constipation in children with MMC and to improve the intestinal habits and QoL of patients and their families. | NBD ScoreSatisfaction scale (0 to 10) | 3 months | Constipation improved in 60% FI improved in 75% NBD score from 17.5 to 8.5 (p < 0.001) Independence - 26.7% Diminution in E. coli urinary tract infections |
| Vande Velde, 201331 | Belgium | Prospective cohortSingle center | 25 SBAge: 5-17 years | To study the use of colon enemas to reach fecal pseudocontinence in SB patients, determining variables associated with the success. | - | Mean of 5 years old | Pseudocontinence in 76% Social fecal continence in 88% Independence - 17% |
| Neel, 201032 | Saudi Arabia | Quasi- experimental pre-test/post-test | 13 SBAge: 5.3 years (median) | To evaluate the efficacy and durability of combined intradetrusor botulinum-A toxin and endoscopic treatment for vesicoureteral reflux with anal irrigation as a total endoscopic and anal irrigation management approach. | - | 12 months | 10 out of 13 achieved fecal continence by having TAI applied for a mean of twice a week and could stop wearing diapers. |
| Donlau, 201333 | Sweden | Quasi- experimental pre-test/post-test | 22 SBAge: 3-17.2 years | To evaluate a step-by-step method to determine goals for self-care training in bathroom activities for children with MMC. | GAS | - | The group that trained in TAI (7 patients), at first, has a median score of 30 (m32.1, range 28–41); after training, the score became 49 (m 44.6, range 32–54), also showing significant improvement (compared mean p=0.02). |
| Choi, 201334 | South Korea | Quasi-experimental pre-test/post-testSingle center | 53 SBAge: 3 to 13.8 years | To evaluate the clinical efficacy of a bowel management program in the QoL of SB children and their caregivers. | Bristol Scale | 3 to 7 months | Success in 81.1% (FI and constipation) |
| Choi, 201535 | South Korea | Quasi-experimental pre-test/post-testSingle center | 44 SBAge: 3-13.8 years | To evaluate long-term clinical efficacy of TAI and its effects on the QoL of SB children and their caregivers. | FIQL | T1=3 monthsT2=3 years | Pseudocontinece from 35.1 to 91.9% at T1 and 89.2% at T2 Lower use of diapers, 1.6 at T1 and 0.2 at T2 FI improvement of 7.3 at T1 and 0.4 at T2TAI satisfaction went from 8 (T1) to 10 (T2) |
| King, 201736 | Australia | Cross-sectional studySingle center | 20 SBAge: 14.5 years (median) | To investigate the efficacy of Peristeen® continence retrograde irrigation in children with SB. | FIQLSt. Marks FI IndexCleveland Clinic Constipation IndexNBD Score | 1-8 years | FI and pseudocontinence improved in 8/9 patients (no significant difference) |
| Ambartsumyan and Rodriguez, 20187 | USA | Narrative Literature Revision | - | To review a step-by-step approach for bowel management in children with SB, and the challenges related with the tt options proposed. | Cites: Pediatric NBD ScoreAdolescent Fecal Incontinence and Constipation Symptom Index | 6 months | Success rate of 66-87.5%; QoL increaseConstipation reduction from 92.7% to 41.5%; FI from 39.9% to 9.8%. and flatulent incontinence from 31.7% to 10%.NDB score reductiona |
| Ausili, 201837 | Italy | Quasi-experimental time seriesMulticentric | 38 SBAge: 6-17 years | To evaluate the short-to-medium term efficiency of TAI and its effect on the quality of life of children with SB and anorectal malformations. | CHQ-PF50 for the parents and SF36 for patients from 12 to 17 years oldBristol Scale | Minimum of 24 months | Constipation improved in 93% (T0) FI improved from 39% (T0) to 11% (T1), and then to 17% (T2) the CHQ-PF50 showed QoL improvementSF36 showed improvement in 9 variables |
| Alhazmi, 201938 | Saudi Arabia | Cross-sectional studySingle center | 109 MMCAge: 5-18 years | To evaluate the efficacy and long-term satisfaction of TAI (Peristeen®) in children with MMC who did not respond to the FI conservative tt. | - | 48 months | 90.4% improvement in FI |
| Kelly, 201939 | USA | Narrative Literature Revision | 22 SB- | Providing updated information for physicians comparing techniques (TAI, cecostomy, and Malone), which have relatively high fecal continence and satisfaction success rates. | - | 4 years | Mean rate of continence with TAI 77.7% (53-97% interval);Constipation improvement: 78% (interval from 53-97%)General improvement of symptoms: 84% (60-100% interval)a |
| Kelly, 202040 | USA | Cross-sectional studyMulticentric | 380 SBAge: 5-19 years | To determine the continence variation and its ability to carry out tt according with the modality and the characteristics of people with MMC and IN. | - | - | Continence rate of 57% with the cone - children Continence rate of 80% with Peristeen® 80% - adolescents9.8% of children and 36.5% of adolescents were independent using the conea |
| Gibbons, 202041 | Ireland | Case–control | 48 SB controlsAge: 3-16 years | To compare bowel function-related quality of life in children with SB with a control group of their peers to better understand the impact of bowel management and evaluate whether QoL differs with varying bowel management strategies | NBD Score | - | There was no QoL difference between bowel management strategies, including the group with no treatment (p = 0.203). Despite active bowel management, the NBD score was lower in the SB group. |
| Milivojevic, 202042 | Servia | Prospective cohort | 39 SBAge: mean 9.5 ± 3.7 years | To examine the effects of bowel management on urodynamic findings in SB children with detrusor overactivity and detrusor sphincter dyssynergia. | Roma III | 12 months | 87.2% gained complete control over constipation, 71.8% gained completecontrol over FI, transversal rectum diameter in echosonography <3, and absence of encopresis (p < 0.001). Intestinal control led to significant improvement in urodynamic parameters (p < 0.001). |
| Van Renterghem, 202143 | Belgium | Quasi-experimental pre-test/post-testSingle center | 14 SBAge:3-18 years | Comparing 2 TAI systems in children with congenital diseases. | Bristol Scale; Satisfaction Scale(0-10) | Minimum of 2 weeks with the cone and 2 weeks with Peristeen® | Use of Peristeen®: 5/7 pseudoconetinent and 2/7 socially continent; Mean satisfaction with the device 8Cone use: 17 pseudocontinent; 4/7 socially continent; and 2 incontinent. Mean satisfaction 8a |
| Pinheiro, 202123 | Brazil | Quasi-experimentalPre-test/post-testSingle center | 19 MMCAge:3-18 years | To evaluate TAI viability using the cone; impact on elimination function and on the QoL of MMC and FI patients, and in the family QoL. | CHQ-PF50 (QV)Wexner FI score | 12 months | The domains with the greatest significance and positive impact on QoLRH was “health alteration”and “global health”, after TAIa |
| Furuta, 202144 | Japan | Quasi-experimentalPre-test/Post-test with non-equivalent control groupSingle center | 16 SBAge: 6-17 years | To investigate changes in the bowel microbiota after TAI in patients with SB. | Bristol ScaleNBD Score | 3 months | Significant reduction of Faecalibacterium and Blautia, with a significant increase of Bacteroides and Roseburia (associated with immune system improvement).Constipation improvements. |
We could not isolate data on the pediatric population in the other outcomes.
SB, spina bífida; FI, fecal incontinence; MMC, myelomeningocele; QoLRH, quality of life as related to health; TT, treatment; FIQL, the fecal incontinence quality of life scale of life; NBD Score, neurogenic bowel dysfunction score; CHQ-PF50, child health questionnaire; GAS, goal attainment scale.
The FI was defined as fecal loss that takes place at least once a month38,40,42,43 or as the involuntary loss of feces at least once a week.29,34,35 Fecal pseudo continence was defined as no loss of feces in the last 6 months31,36,43 or as fecal loss less frequently than once a week, during TAI.29,35 Social fecal continence was defined as fecal loss less frequent than once a month,28,31,40,43 while fecal continence indicates no fecal loss while not undergoing treatment.29,35 Except for a study that used ROMA III and transrectal echography criteria42 to determine cases of intestinal constipation, most were not based on ROMA IV criteria for this diagnosis in the pediatric population. Internal constipation was mostly identified by the studies in a more homogeneous manner, being understood as indicating eliminations less frequent than three times a week and/or hard, large stools, difficult to eliminate by those with high sensitivity and/or requiring laxatives to evacuate.25,29,31,34,35,38
The term “retrograde irrigation” was used by 11 studies7,24-27,29,31,36,40-42 while 10 used the name “transanal irrigation”.28,30,32-35,37-39,43,44 Both referred to the insertion of large volumes of water or saline through the anus using a cone or pump to empty the intestines. One study used the term high-volume enema for the use of cones and the term transanal irrigation to refer to the use of the Peristeen®40 system. Another used these terms as synonyms, choosing the expression high-volume enema.7
Outcome evaluation parametersFour studies30,34,41,44 used the Neurogenic Bowel Dysfunction Score (NBD-S) to evaluate the neurogenic bowel. One of them7 cited the Pediatric Neurogenic Bowel Dysfunction Score, the Adolescent Fecal Incontinence, and the Constipation Symptom Index as promising scales.
Two articles used specific scales to evaluate anal incontinence. One of them23 used Wexner's Incontinence Index, also known as Cleveland Index, while the other36 used the St. Mark Fecal Incontinence Index as well as the Cleveland Clinic Constipation Index. The Bristol Scale was used to characterize the feces34,37,43,44 and semistructured questionnaires were used to evaluate symptoms related to the neurogenic bowel.24,26,28,29,31,34,35,37,40 Journals to keep track of eliminations and symptoms after TAI were used as parameters for clinical evaluation and adjustments in technique.30,37,43
To evaluate the quality of life, the studies used The Fecal Incontinence Quality of Life Scale – FIQL,35,36 the Child Health Questionnaire - CHQ-PF50,23,37 which evaluates the quality of life from the perspective of the caregiver, and the Quality of Life Questionnaire SF-3637 for adolescents.
The satisfaction with the TAI was evaluated according to graduation scales that varied from 0 to 5,26 0 to 4,25 and 0 to 10.30,43 One study used the Goal Attainment Scale GAS to verify whether it had reached its goals.33
Criteria for the recommendation of TAI, training, and healthcare actionsThe main condition that recommended TAI was FI.23,24,26-28,30-32,34,37,43 Other criteria were failed earlier neurogenic dysfunction treatment,23,25,29,30,34-38 untreatable chronic constipation,27,30,35,43 and dissatisfaction caused by the elimination dysfunction.23,25,30,37 One study24 mentioned the motivation of the individual/caregiver, while others indicated their age, corroborating indication criteria starting with children age,23,25 4-6,35 5 or older,29 and 6 or older.30
Complementary exams of rectum manometry and rectoscopy were carried out,28 as well as laboratory exams with sodium serum dosage,30 but no issues were found after TAI treatment.
The TAI training was carried out while the individual was hospitalized24,25,39,43 or in outpatient clinics23,26,28,38 or at home.33 One study mentioned that the urotherapist provided a verbal and visual explanation about the use of the irrigation device, phoning the patient after 24-48h to clarify any doubts.32 A single study detailed the protocol for training the use of the technique.23 Training for two25 or three23 days was mentioned, with technical instructions provided at the moment of training.
The most commonly cited device to carry out TAI was the rectal catheter with an inflatable pump,24-26,30,36-39,44 followed by its application using a cone23,27-29,31,33, some studies cite both7,34,35,40,41,43, with a single study mentioning the use of tube rectal irrigation.41 Some studies followed recommendations to use the cone for those below 6 years old and the catheter with the pump (Peristeen®) for older patients.34,35 The most common solution for irrigation was water,7,23,27-31,34-39,43 lukewarm23,24,28,29,31 and in volumes from 10 to 20 mL/kg,7,23-27,37,39,43 adjusted according to patients’ needs. The use of the saline solution, homemade or not, was also cited,7,24-26,36 as well as that of saline with glycerin.42
The TAI was carried out daily after training sessions on how to do it.28,29,31,34,35,37,39,42,43 Then, its frequency decreased to once every 48h24-27,29,31,34,35,37-39,43,44 or even three times a week,26,34,35,37,38,43 depending on the results. Most individuals spent less than 30 minutes carrying out the procedure.24,26-28,30,31,37
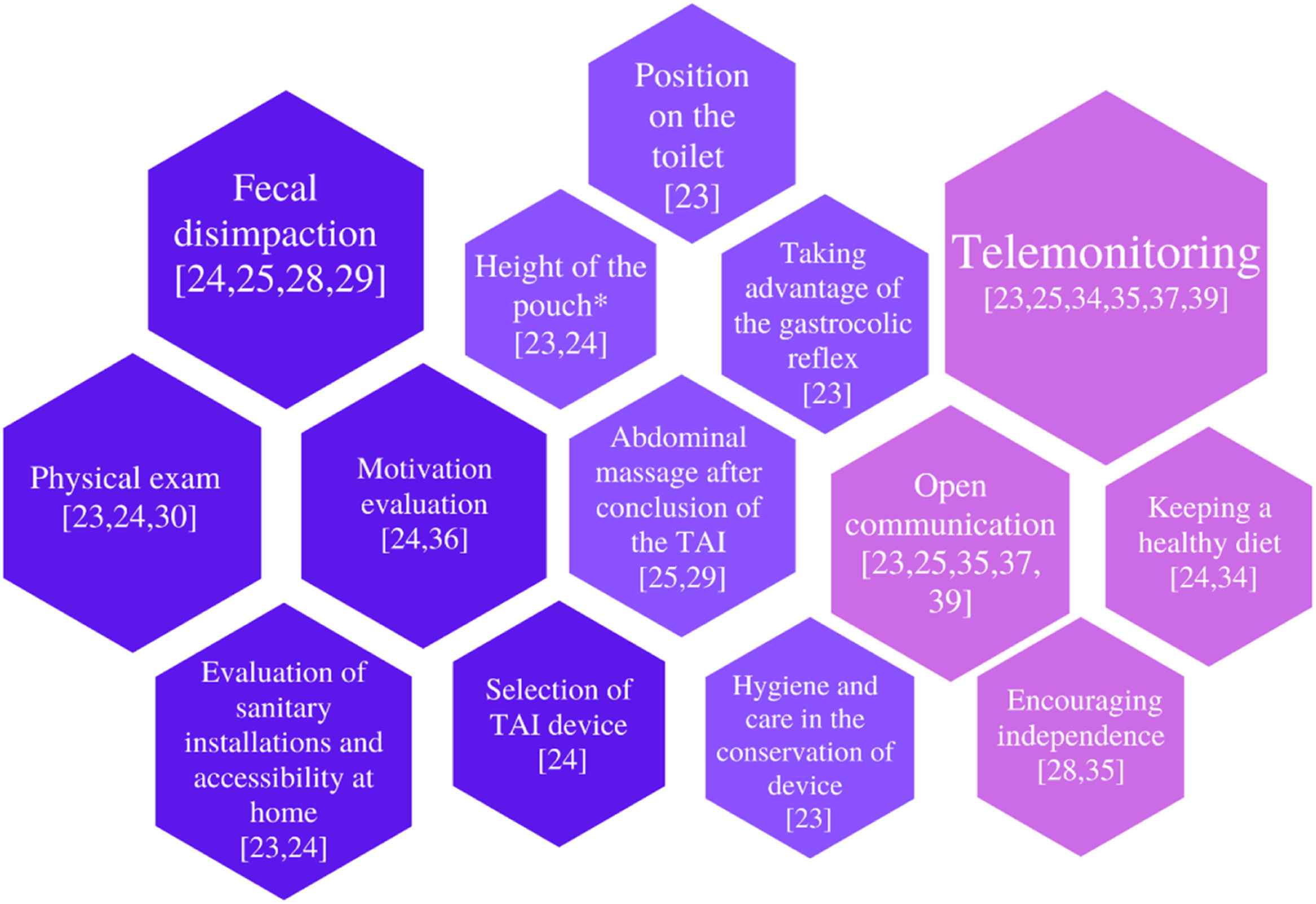
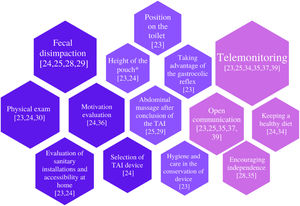
Health care actions listed in the studies were separated into three groups, according to the trajectory of the patient: preparation for training (dark purple); care actions during the procedure, in addition to volume, irrigation solution, and temperature (light purple); and follow up health care (pink). These are shown in Figure 2. The importance of long-term longitudinal follow-up, in person or remotely, was cited.
Many studies pointed to the level of dependence of the caregiver to carry out the TAI7,23,28,30,31,35,37,39,40 and suggested encouraging their independence.28,35 Two studies indicated that they started TAI early to improve long-term results.23,39 One study provided TAI home training for children and adolescents in order to help them become independent in the performance of the procedure. The study used individualized goals assessed by the Goal Attainment Scale (GAS) and resulted in a significant increase in independence.33
TAI adherence rateThe adherence rate to the procedure was above 75%,7,26,28-32,35,37-39 often surpassing 80%.7,28-30,32,35,37,38,42 The four studies with the longest follow-up period, a mean of five years, reported an adherence rate above 75%.31,35,38,39
Collateral effects and problems with techniqueThe main problems with the procedure were liquid leakage,26,39 difficulties in managing the pump, including early extrusion and ruptures,26,35-37,39,43 difficulties in inserting and removing the catheter25 and the high cost of the material (Peristeen®).35,36
The most common adverse effect was discomfort/abdominal pain and/or anorectal pain,7,23-26,28,30,35-37 followed by sudoresis, nausea, trembling, headaches, facial flushing, vagal episodes,23,36,37 incomplete or inefficient eliminations after TAI,25,28,30 emotional suffering and/or fear related to the procedure.7,31,43 Signs of chemical colitis (bloody and mucous feces, with or without abdominal pain) were associated with the use of soap or glycerin, and a study suggested being careful when choosing additives to the base irrigation solution.7
In no study the complication most commonly associated with TAI was mentioned, that is, intestinal perforation.7,39 This complication has been reported in literature reviews7,39 from a global audit, which found 2 perforations for every 1 million procedures among all ages in populations using TAI.45 They highlighted some contraindications, including anal or colorectal stenosis, active irritable bowel syndrome, being within three months of postoperative anal or colorectal surgery, and ischemic colitis.39
DiscussionDespite the increase in the number of publications on the topic, studies about TAI in the pediatric population with SB are still scarce, considering such a relevant problem as FI, which can have devastating effects on the health and quality of life of these individuals and their families. Many studies that were excluded from this research involved data from other grouped diagnoses, such as anorectal malformations and Hirschsprung disease, so as not to favor the peculiarities associated with the individual with SB, potentially interfering in the interpretation of the results.36
Most publications come from developed countries with a single one from Brazil, showing how scarce access to devices to carry out TAI.23 This Brazilian work, a dissertation, mentions Brazilian articles17,46 that use the same technique and device, that is, the cone and the regulating pouch with an integrated thermometer, which are sold in Brazil and recommended for the irrigation of ostomies. The studies show the use of these devices to be safe and effective.17,23,46
No studies had a qualitative approach, which corroborates Sanders,47 according to whom publications are limited in regard to the perception of parents and individuals about the use of TAI in the management of neurogenic bowel in their children. Most studies aim to evaluate the effectiveness of TAI, as indicated by the fact that most are intervention studies. Nonetheless, qualitative and quantitative research approaches are complementary, leading to a deeper and multifaceted understanding of the phenomenon at hand. Qualitative studies can help understand the processes and phenomena involved in the acceptance and adherence to the procedure by children and their relatives, providing support to improve the experience of those involved. Furthermore, the scarcity of multicentric studies, also mentioned by Ausili,37 may limit the applicability of TAI evidence in different contexts.
The variety of definitions of terms and parameters impacts the identification of these issues by health workers, the recommendations for the procedure, and on the comparative analysis of the results.6,48 It is well known that the International Continence Society (ICS)49 refers to FI as any involuntary loss of feces associated with prejudice in quality of life, which, as a quantitative parameter, is not sensible to fecal loss improvement. On the other hand, social fecal continence is a term that could be used more often in results, since it reflects the satisfaction of individuals with the control of fecal losses in the environment they are inserted, despite the fact the term still needs standardization. It stands out that it was not possible to use the ROMA IV criteria to diagnose constipation, since this is a neurogenic dysfunction. Starting in 2010, the use of scales and indexes validated in all intervention studies has been validated, showing higher methodological rigor in the quantitative evaluation of TAI outcomes.
The use of scales non-specific for the pediatric population, such as the NBD score,50 was the most common. This particular score evaluates constipation and fecal incontinence symptoms correlated with quality of life. It is yet to be translated into Brazilian Portuguese. In 2014, the Pediatric NBD score51 was published. Nonetheless, as Ambartsumyan7 states, it still needs to be tested in studies with larger samples. The Bristol Scale,52 despite not being specific for neurogenic dysfunction, provides graphic representations of the consistency of feces, which is an important tool for diagnosis, therapeutic monitoring, and research. It also has a pediatric version created more than 10 years ago and validated for Brazilian Portuguese in 2019.53 The use of this version, however, was not found in the studies included. Few indexes or scales translated and validated for Brazilian Portuguese are related to neurogenic bowel. Wexner Index54 is the most commonly used parameter among Brazilian proctologists to evaluate the severity of anal incontinence.55 The FIQL is a parametrical option validated to evaluate the impact of fecal incontinence on quality of life,56 however, it is not aimed for use in the pediatric population. The questionnaire CHQ-PF5057 is an option to evaluate the perception of the parents about the quality of life of their children. There is a quality-of-life questionnaire specific to the SB population, which includes the influence of urinary incontinence and intestinal habits. It is a short, valid instrument, with a version for children aged 8 through 12 named Quality of Life Assessment in Spina Bifida for Children (QUALAS-C),58,59 and a version for adolescents aged 13 through 17, named Quality of Life Assessment in Spina Bifida for Teenagers (QUALAS-T).60 However, these scales were not used in the publications found in the present research.
The criteria for TAI recommendations are basically focused on FI and constipation, which are both resistant to conventional management. Few studies cited how relevant it is to consider the motivation of the individual/caregiver to improve intestinal dysfunction. Although the age when TAI began to be used varied between studies,23,25,30,31,35 Caponcelli et al.14 suggested that the procedure could be recommended regardless of age when it is necessary to improve satisfaction with bowel management.
Daily TAIs aid in the process of fecal disimpaction and can be carried out, according to results, on alternate days, or, at least, three times a week, to avoid fecal impaction and the need for oral laxatives. The time spent in TAI, less than 30 minutes in most cases, is reasonable, especially considering that intestinal management using other measures (toilet training and manual maneuvers for intestinal evacuation) can take even longer and be less effective.4 Although the frequency, the type of irrigation solution used, and the volume of liquid were mentioned, the procedure itself was scarcely described. This could affect the safety and comfort of the individual, as well as the confidence of parents, who are essential actors for the continuity of care.
Although most studies cited the use of the catheter with a pump, notably of the brand Peristeen®, this device has been associated with issues with technique, including the rupture of the pump, not to mention its high price,43 despite the fact it was also associated with more independence. On the other hand, the cone was associated with less discomfort, more acceptance, and lower cost.34,43 These results are in consonance with a study about the intestinal management program that compares TAI devices and states that the cone is preferable for use in younger children.9 Nevertheless, it is important for children and families to have options, being able to make a decision considering the context in which each device is the best, according to access, comfort, and preferences. Everyone should have access to the best option possible, compatible with their desires and values, so the challenging condition that is FI can be managed.
There were no issues in complementary exams (rectal manometry and rectoscopy), carried out before and after the TAI.28 Therefore, these could be used, in case of diagnostic doubt, to recommend or clarify complications after the beginning of TAI.
Although the TAI is a simple technique, especially when using the cone, most studies highlighted the degree of dependence of the caregiver in this management process. This fact may be explained by the complexity of cognitive and behavioral issues of individuals with spina bifida, who could present associated malformations or encephalic lesions.1,2 In these cases, some degree of intellectual deficiency and/or difficulties planning and executing the actions can interfere, leading to a dependency on a caregiver. This is also true for motor difficulties. Home training with individual goals can be a beneficial strategy to reach independence in the execution of the TAI.33
The high adherence rate, above 75%, was related to the high efficiency and safety of the procedure. Bildstein61 determined in a study that the success of the first training session was the only predictive factor about adherence to the procedure in the medium term. Nonetheless, longitudinal follow-up is essential to provide support and the adjustments in technique needed, favoring therapeutic success and long-term adherence. In this study, telehealth stood out as an instrument to monitor, support, and provide longitudinal follow-up.
In the pediatric population with SB, the TAI was shown to reduce FI, improve constipation, and increase general satisfaction, as well as the quality of life of individuals. It was also associated with changes in the intestinal flora, favoring improvements in constipation, the immune system, and reducing urinary tract infections.44 Bowel management using the TAI led to improved urodynamic parameters: increased vesical capacity decreased maximum detrusor pressure, and increased bladder compliance (p < 0.001). There were also significant decreases in leak point pressure and post-micturition dribble (p < 0.001).42
The most common adverse effect to TAI was abdominal and/or anorectal discomfort/pain, which is one of the main causes of people abandoning the procedure. The main issues related to the technique were the leakage of liquid and/or feces, and difficulties managing devices, especially the catheter with a pump. These could be minimized if the individual/caregiver had more access to the intestinal rehabilitation team and had a closer bond with them.24 The most serious potential complication, intestinal perforation,45 did not take place among the individuals studied here. It would be relevant to know the main contraindications of the technique.
ConclusionDespite the variety in evaluation parameters and outcomes, the authors found scientific evidence according to which the TAI is a safe and effective method that can promote high rates of success in the management of the neurogenic bowel.
The strengths found include an increasing trend in the number of publications related to the topic; the use of standardized and validated scales that can facilitate the production of more robust evidence; and the safety and efficacy of the procedure in long-term studies. In addition, evidence highlighted the importance of longitudinal follow-up and support from the health team involved in the procedure.
The shortcomings to be addressed are associated with the current scarcity of individual-focused studies to investigate the needs and perceptions of those who are experiencing the condition, not to mention the little standardization of training protocols. The authors recommend the production of further comparable multicentric studies, addressing health care more in-depth to improve the experience of individuals and their families in the process of teaching and learning the TAI procedure. Other issues that should be investigated are factors related to non-adherence, cases of abdominal and anorectal pain, and cases in which the sensitivity was improved.
There is a pressing need for studies about TAI in the Latin American pediatric population with SB, especially in Brazil, so the population that is suffering from neurogenic bowel can have access to the best options for bowel management, including a greater variety of devices for TAI.
To all children, adolescents, and families that inspired us to search for the best solutions to improve the quality of life of this population. The authors would also like to thank the SARAH Network of Rehabilitation Hospitals for the support and encouragement to produce the best evidence-based practices.
Study conducted at the University of Brasilia (UnB) and SARAH Network of Rehabilitation Hospitals, Brasília/DF, Brazil.