This was a systematic review of studies that examined the impact of epidemics or social restriction on mental and developmental health in parents and children/adolescents.
Source of dataThe PubMed, WHO COVID-19, and SciELO databases were searched on March 15, 2020, and on April 25, 2020, filtering for children (0–18 years) and humans.
Synthesis of dataThe tools used to mitigate the threat of a pandemic such as COVID-19 may very well threaten child growth and development. These tools — such as social restrictions, shutdowns, and school closures — contribute to stress in parents and children and can become risk factors that threaten child growth and development and may compromise the Sustainable Development Goals. The studies reviewed suggest that epidemics can lead to high levels of stress in parents and children, which begin with concerns about children becoming infected. These studies describe several potential mental and emotional consequences of epidemics such as COVID-19, H1N1, AIDS, and Ebola: severe anxiety or depression among parents and acute stress disorder, post-traumatic stress, anxiety disorders, and depression among children. These data can be related to adverse childhood experiences and elevated risk of toxic stress. The more adverse experiences, the greater the risk of developmental delays and health problems in adulthood, such as cognitive impairment, substance abuse, depression, and non-communicable diseases.
ConclusionInformation about the impact of epidemics on parents and children is relevant to policy makers to aid them in developing strategies to help families cope with epidemic/pandemic-driven adversity and ensure their children’s healthy development.
There are scarce data about the impact of epidemics on children’s growth and development. Preserving children’s well-being during stressful times such as pandemics needs greater attention in the medical literature. Children’s health is one of the most important issues in the Sustainable Development Goals (SDGs), and science has shown that genetic predispositions are modified by environmental influences, such as those experienced during a pandemic, and affect learning capacities, adaptive behaviors, lifelong physical and mental health, and adult productivity.
Epidemics or pandemics, such as COVID-19, produce potential risks to child development due to the risk of illness, protective confinement, social isolation, and the increased stress level of parents and caregivers. This situation becomes an adverse childhood experience (ACEs) and may generate toxic stress, with consequent potential losses for brain development, individual and collective health, and the long-term impairment of cognition, mental and physical health, and working capacity of future adults.
Studies to improve the understanding of the impact of epidemics and pandemics such as COVID-19 on children’s mental health and development can help to guide strategies to prevent damage to children’s growth and promote positive development.
The COVID-19 pandemic has produced impacts on general health and child development through exposure to the virus and consequent infection, as well as through the social confinement recommended or mandated in an attempt to slow the progress of COVID-19, enable adequate medical care, and prevent the collapse of health care systems.
Consequently, the pandemic demands that millions of parents and caregivers demonstrate a high capacity for resilience to ensure protective health measures to prevent contagion. One of the pillars for overcoming adversity is interaction among people, which is compromised by isolation, leading to increased stress in both parents and children. In addition to general care and strategies to minimize stress, preserving children's well-being is an important focus, increasingly highlighted in medical literature. Children’s good health is one of the most important issues for the SDGs, and science demonstrates that genetic predispositions (biology) are modified by environmental influences (ecology) and affect learning capacities, adaptive behaviors, lifelong physical and mental health, and adult productivity.1
From this perspective, there are several factors that influence the physical and mental health of children and adolescents experiencing the stress inherent in a pandemic, such as isolation itself, school shutdown, reduced social life and physical activities, changes to routine, sleep difficulties, exposure to disharmony at home, excessive screen use, unhealthy diet, and others.2
Depending on levels and kinds of support, high and continuous stress may either be tolerable or become toxic to children and adolescents. ACEs are traumatic or stressful events that occur in childhood, such as abuse, neglect, domestic violence, and parents with substance dependence or mental illness. The pandemic can be understood as another source of ACE.3
This review of the scientific literature about the impacts of isolation, environmental restriction, social distancing, and the challenges of maintaining general child health and development within the context of previous epidemics and the COVID-19 pandemic was undertaken in light of the above.
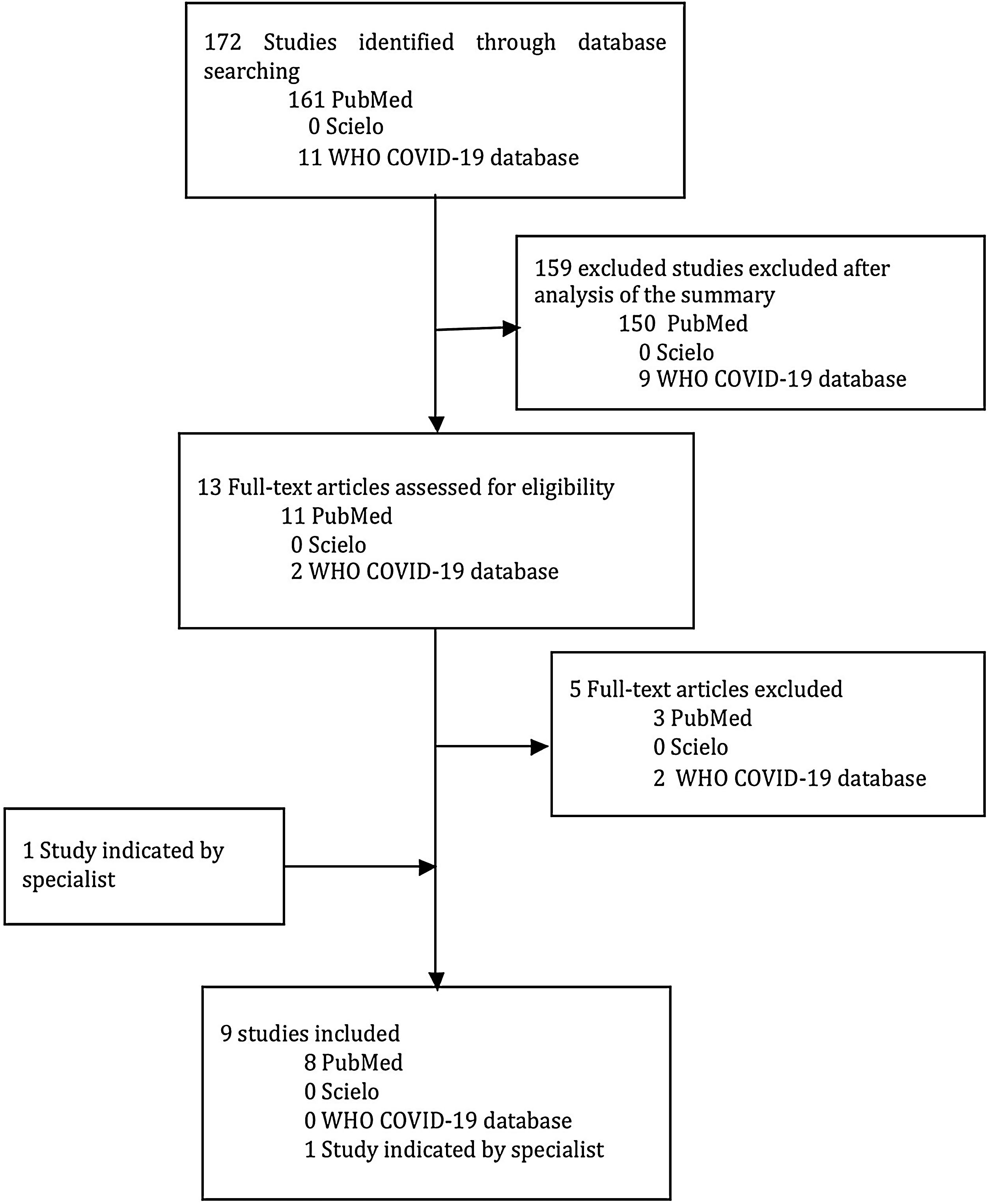
MethodsThe guidelines from the Preferred Reporting Items for Systematic Reviews4 were used to conduct this review of the scientific literature about the impacts on the general health, development, and mental health of children and adolescents as a result of previous epidemics and/or the COVID-19 pandemic.
Observational, cross-sectional, cohort, and ecological studies, case series, and systematic reviews, without language restrictions were included in the study. Studies of non-human subjects and experimental studies were excluded. The target population for this review was that aged 0–18 years, with no limitations related to gender, race or health condition.
The PubMed, World Health Organization (WHO) COVID-19 and SciELO databases were searched on March 15, 2020, and again on April 25, 2020. All articles were double-screened by two authors according to title and summary in order to answer the following research question: "What are the consequences of previous epidemics and the COVID-19 pandemic on children’s quality of life, health, and development?" Health descriptors for research and related terms derived from DeCS and MeSH were: child, stress, pandemic, Ebola, influenza pandemic, and COVID-19. Combinations of descriptors were: (Child AND stress AND [pandemic OR Ebola OR flu pandemic OR COVID-19]), (child AND COVID-19), (pandemic AND COVID-19 AND child).
All of the studies were assessed in relation to their characteristics, quality, and congruence with the theme. Each study’s summary was initially analyzed and those that did not meet the inclusion criteria were excluded. Papers whose full-text was included were reviewed by author. A list of references for each article was analyzed in an attempt to select additional articles related to the topic. Experts in the field also suggested certain articles. Two tools were used to measure the quality of the articles included in this review: CASP and AMSTAR 2 (Fig. 1).
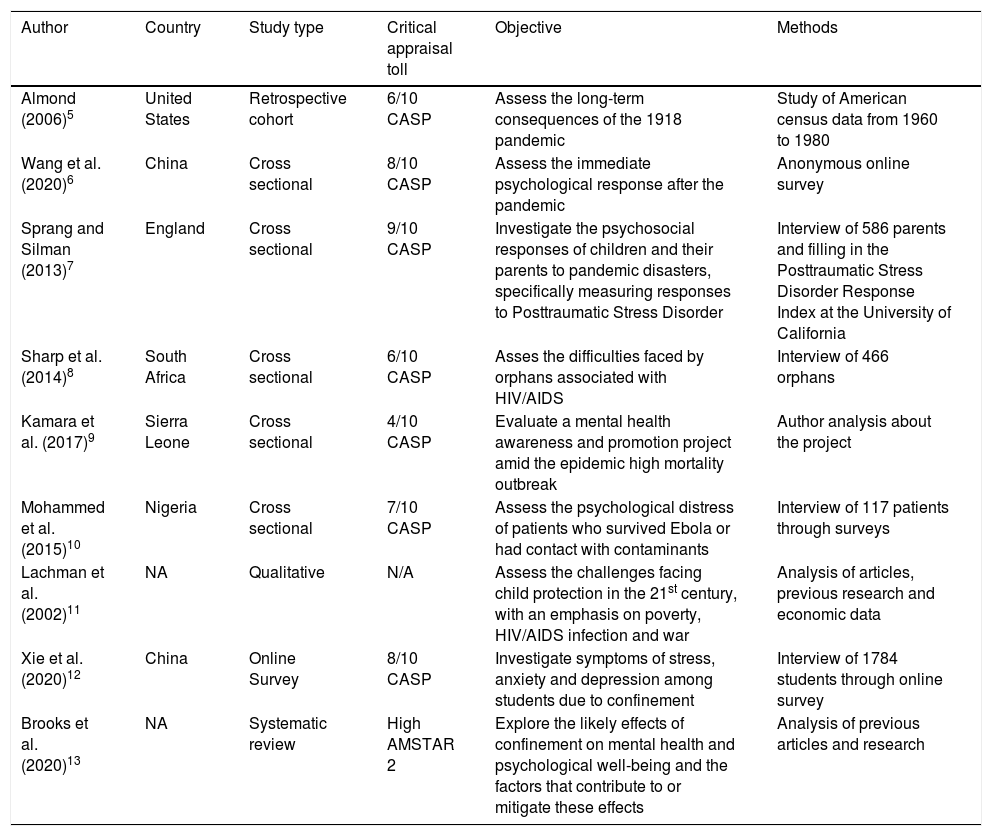
ResultsFrom the PubMed platform, 80 articles were selected, of which 14 were analyzed and eight were included in this review. A search for the descriptors resulted in only two studies from the WHO COVID-19 database, neither of which was selected, since they did not meet the criteria of the present review. No articles containing the descriptors were found on the Scielo platform. One further article was retrieved by manual search. In total, nine studies were included in this review. The CASP checklist resulted in scores greater than 5 in six studies and one less than 5. Using the ASTAR 2 criteria, the quality of the systematic reviews included was classified as high high (Table 1).
Summary of the studies included in this review.
| Author | Country | Study type | Critical appraisal toll | Objective | Methods |
|---|---|---|---|---|---|
| Almond (2006)5 | United States | Retrospective cohort | 6/10 CASP | Assess the long-term consequences of the 1918 pandemic | Study of American census data from 1960 to 1980 |
| Wang et al. (2020)6 | China | Cross sectional | 8/10 CASP | Assess the immediate psychological response after the pandemic | Anonymous online survey |
| Sprang and Silman (2013)7 | England | Cross sectional | 9/10 CASP | Investigate the psychosocial responses of children and their parents to pandemic disasters, specifically measuring responses to Posttraumatic Stress Disorder | Interview of 586 parents and filling in the Posttraumatic Stress Disorder Response Index at the University of California |
| Sharp et al. (2014)8 | South Africa | Cross sectional | 6/10 CASP | Asses the difficulties faced by orphans associated with HIV/AIDS | Interview of 466 orphans |
| Kamara et al. (2017)9 | Sierra Leone | Cross sectional | 4/10 CASP | Evaluate a mental health awareness and promotion project amid the epidemic high mortality outbreak | Author analysis about the project |
| Mohammed et al. (2015)10 | Nigeria | Cross sectional | 7/10 CASP | Assess the psychological distress of patients who survived Ebola or had contact with contaminants | Interview of 117 patients through surveys |
| Lachman et al. (2002)11 | NA | Qualitative | N/A | Assess the challenges facing child protection in the 21st century, with an emphasis on poverty, HIV/AIDS infection and war | Analysis of articles, previous research and economic data |
| Xie et al. (2020)12 | China | Online Survey | 8/10 CASP | Investigate symptoms of stress, anxiety and depression among students due to confinement | Interview of 1784 students through online survey |
| Brooks et al. (2020)13 | NA | Systematic review | High AMSTAR 2 | Explore the likely effects of confinement on mental health and psychological well-being and the factors that contribute to or mitigate these effects | Analysis of previous articles and research |
The study by Almond describes poor educational and physical performance and lower income and socioeconomic status as adults in children whose mothers were infected by the Spanish flu during the 1918 pandemic.5
The study by Wang et al. on the psychological consequences of the COVID-19 pandemic, investigated 1210 individuals, the majority female (67.3%), from families of three to five people (80.7%), with children (67.4%), in 194 Chinese cities. In total, 53.8% of respondents rated the psychological impact of the outbreak as moderate or severe, 16.5% reported moderate to severe depressive symptoms, 28.8% reported moderate to severe anxiety symptoms, and 8.1% reported moderate to severe levels of stress. The majority of respondents spent 20 to 24 h a day at home (84.7%) and stated that they were concerned about family members contracting COVID-19. The “parents” group had higher levels of stress, anxiety, and depression when compared with the “no children” group, a statistically significant difference, and the majority of parents stated that they were “very” or “somewhat worried” about a child getting COVID-19.6
In another study, data were obtained from 586 parents interviewed in 2009 in the United States, Mexico, and Canada about the H1N1 pandemic.7 The respondents were predominantly female (78%), with an average age of 37 years. In the investigation of factors related to child stress, the most common diagnosis was acute stress disorder (16.7%), while 6.2% of children had post-traumatic stress disorder (PTSD). A total of 44.4% reported that their children did not receive professional mental health support, while 93.2% of the parents did not receive psychological assistance from professionals. Of the children who had access to mental health services during the pandemic, the most common diagnosis was anxiety disorder (20%), while only 1.4% had PTSD. Additionally, the criteria for diagnosing PTSD were found in 30% of the confined children and in 25% of the parents (based on reports from 398 parents), which indicates the high traumatic potential of social isolation and living in conditions of constant fear due to the advance of the pandemic.7
Sharp et al. studied the level of child stress in 466 children between the ages of 7–11 years in South Africa orphaned due to HIV/AIDS, based on responses to a questionnaire survey. Of the respondents, 51.93% were female. Most respondents were in serious financial difficulties: 57% of the respondents did not have adequate clothes, and 60% did not have adequate school uniforms. Only 49.1% received three main meals a day. Just over half of the orphans' families had an income, 75% of which were based on subsidy. In addition, 31.7% of the surveyed children met the criteria for anxiety disorder, 26 (5.6%) met the criteria for affective disorder, and 40.6% of the sample met the criteria for ADHD.8
Kamara et al. described a mental health awareness and promotion project in the midst of a high fatality Ebola epidemic in Sierra Leone, in which a large number of people reported psychosocial problems. A total of 8700 people were infected and 3600 died, resulting in 3400 orphaned children. In the 143 interviews of patients attending the psychosocial and counseling clinic, 19% were aged 0–17 years, and half of the patients (71) experienced mild distress or depression, anxiety disorders, and grief or social problems, while 30 patients (21%) had psychosis and needed medication. Interventions took the form of individual care in hospitals aimed at improving the mental health of patients and professionals.9
A cross-sectional study assessed the psychological distress of 117 patients having an average age of 34 years who had survived or had contacts with the Ebola epidemic in Nigeria.10 Of the 117 respondents to a questionnaire, 78 (66.7%) were female of maternal age, 77 (65.8%) had a university education, and 45 (38.5%) were healthcare professionals. The death of a friend (OR = 6.0, 95% CI, 1.2–32.9) was significantly associated with feeling unhappy or depressed and with loss of ability to concentrate. Additionally, the most reported psychological suffering was “inability to focus on the task at hand” (38.5%) and “loss of sleep due to worry” (33.3%).
The systematic review by Lachman et al. focused on three important challenges for the protection of children's physical and mental integrity in the 21st century: poverty, HIV/AIDS, and wars, especially in less developed countries.11 The review specifically addressed problems associated with the economic situation in African countries (in Nigeria, for example, 58% of boys, 44% of girls, and 55% of children under 4 years of age were in a state of chronic malnutrition), and the challenges faced by those orphaned due to HIV/AIDS. The study suggests interventions and presents statistical data regarding weak economies and insufficient investments in countries such as Nigeria and Namibia, as well as citing data on the situation of refugees and on the psychological impact of wars (10–20% of children exposed to war are susceptible to psychiatric disorders).
Xie et al. investigated symptoms of depression and anxiety among students in Hubei province, China, during the COVID-19 school closures through an online crowdsourcing platform. Out of 2330 students, 1784 agreed to participate (1012 boys, 56.7%). A total of 22.6% of students reported depressive symptoms, while 18.9% reported anxiety symptoms. They concluded that serious infectious diseases, such as COVID-19, may cause mental health problems in children and that more studies are needed on this issue.12
Brooks et al. conducted a review of studies on the psychological impact of quarantine due to COVID-19. Most studies reported anxiety, stress, and depression.13 From the surveys included in the review, data revealed that more than 20% (230 out of 1057 individuals) reported fear, 18% reported nervousness and 186 reported sadness. Additionally, pre-quarantine predictors were shown to influence the level of psychological impact — for example, having a history of psychiatric illness was associated with feelings of anxiety and anger, while lower levels of formal education, lower age (16–24 years), female gender, and having one child as opposed to no children (although having three or more children appeared somewhat protective) were also associated with negative psychological impacts. The longer the quarantine, the greater the levels of post-traumatic stress. Fear of infection, a lack of basic supplies, and unclear information from officials were associated with frustration and anger. Among the post-quarantine stressors analyzed, financial loss was considered to be a risk factor for psychological disorders. Another study compared post-traumatic stress symptoms in quarantined parents and children with those who were not quarantined, revealing higher mean post-traumatic stress scores in children who had been quarantined than those who had not. Conversely, one study found that, although very few participants were extremely concerned about becoming infected or transmitting the virus to others, those who were concerned tended to be pregnant women and those with young children. Finally, the review proposed activities to mitigate the consequences of isolation, which included providing the population with as much clear information as possible, providing adequate supplies, seeking to reduce stress, and providing organizational support for health-care professionals.13
DiscussionThe COVID-19 pandemic has imposed a number of changes on daily routines needed to preserve individual health. Meanwhile, it is important to note that children around the world continue to grow and develop. In this scenario, one priority challenge is identifying and discussing pandemic-related factors that can negatively affect children’s growth and development and impair each child’s full potential, in order to develop prevention strategies that enable a healthier and more productive population over both the short and long term.
The scientific literature describes healthy pregnancy, balanced nutrition, immunity to diseases, restful sleep, a family environment rich in positive stimuli, and a high-quality educational system as the fundamentals for optimal child growth and development.14 All these fundamentals are relevant to the prevention of toxic stress and for the development of strong and lasting neural connections in the child's brain.15
The high level of stress that humanity is experiencing as a result of the COVID-19 pandemic may generate tolerable or toxic stress for children and adolescents, depending on if and how support is ensured. Under the appropriate care and support of adults who provide children with constant feelings of security and affection, the child’s body reorganizes itself biochemically and quickly returns to levels of physiological functioning without further damage.16 However, when this support is non-existent or inadequate, a failure of the body's functions to return to basal level primarily impacts the cardiovascular and neurological systems, with consequent irreversible loss of connections in the infant brain, due to toxic stress.17,18
Several factors related to the pandemic are recognized as ACEs and negatively interfere in the construction and structuring of the child's brain architecture.19,20 Restrictive social and economic reconfigurations, the fear of contagion, illness caused by COVID-19, isolated family life, school closures, the lack of support networks for other adults, the loss of loved ones, the difficulty of combining working from home with full-time childcare, financial challenges, increased exposure to pre-existing vulnerabilities (such as domestic violence, drug use, and mental illness in family members) can result in toxic stress, which will increase according to the sum of ACEs.21
The literature demonstrates that, for both parents and children, sleep routines and the balance of daily activities are usually altered during social isolation. In this context, the quality and duration of sleep may be irregular, the level of physical and outdoor activities substantially decreases, and the use of electronic devices such as TVs, cell phones and tablets (screen time) increases.2 These changes prevent child development from reaching its full potential.22
An increase in parental stress levels during a pandemic, a factor that directly interferes in children's quality of life, is therefore evident.6 Anxiety, excessive concern with cleanliness, excessive fear of falling ill or losing a loved one, concern for the elderly, increased domestic accidents, mood disorders, anxiety disorder, panic, or obsessive-compulsive disorder, and post-traumatic stress are consequences that children and adolescents may experience, according to research into pandemic situations similar to the current one.7,23
In addressing the challenges for pregnant women during pandemics, fetal losses caused by possible maternal infection have been investigated; however, losses due to secondary causes, such as mood changes during pregnancy and in the postpartum period are also relevant.24,25
The literature reveals that maternal anxiety and depression during pregnancy are related to impairments in children’s neurodevelopment and predispose increased behavioral disorders.5
Although there are no consolidated studies on the possible impacts of COVID-19 on the health of pregnant women and their children, especially over the long term, the maternal stress caused during this period is a problem that needs to be more widely addressed.26
Genetic developmental programming is strongly influenced by the environment. In an environment with social restrictions — where play and leisure activities are only possible within the home environment; where people wear masks and the learning of facial expressions, communication, and language is restricted; and where demonstrating affection is discouraged by many — there is a tendency towards limitations in the formation of certain areas of the brain, including the social brain, with consequent impairment in the acquisition of cognitive, behavioral, social, and communication skills.27
Social isolation taken as a prophylactic measure during pandemics is important, but may have several negative impacts — such as anxiety and stress in adults and also in children — since free socialization and relationships are important for well-being, increasing social behaviors and stimulating synaptic connections, favoring the construction of the social brain. Physical activities relevant to adequate physical conditioning, emotional well-being, and growth and development in childhood are also restricted.28,29
Studies comparing the symptoms of post-traumatic stress in parents and children confined in pandemic situations with those of families in normal routines indicate that stress levels are four times higher for children who have been in quarantine.7
During pandemics such as the current one, one common measure is suspending in-person school activities to aid in controlling the spread of the virus. The possible ways and times to carry out such activities are heavily discussed in the scientific context and their impacts affect families in different ways.
The effectiveness of school shutdown as a measure to combat the spread of epidemics such as COVID-19 has been discussed.30 Viner et al. examined 16 studies (ten studies of the SARS outbreak in 2003, one of other coronavirus epidemics, and five addressing COVID-19) and found scarce data relating to the effectiveness of closing schools to control COVID-19. Although some studies point to the effectiveness of school closure as part of a general package of social isolation measures, some studies using models indicate divergent results, while an isolated analysis of school shutdown was not found. In addition, school closure in cases of virus pandemic appeared to have better results when transmission was greater in children than adults, unlike with COVID-19.
A modeling study by Bayham et al. included information from 3.1-million American individuals and estimated the impact of school shutdown on healthcare professionals involved in the care of children between the ages of 3–13 years.31 They concluded that, although there may be a decrease in COVID-19 mortality due to a reduction in cases as a result of school closures, loss of children’s access to school healthcare workers may result in an increase in mortality, i.e., the net benefit of closures may be lower. A definitive conclusion could not be reached because the real damage to the health-related workforce and of possible social interactions to address this problem (local care networks and family for example) was not definitively known.
Kim et al., in a 2020 study based on a mathematical model that evaluated populations in two groups, one aged 19 years or below and another aged over 19, using a susceptibility-exposure-infection-recovery model to analyze school closure in Korea, concluded that this approach was essential in mitigating the COVID-19 epidemic.32 They added that maintaining the suspension of classes would save 255 children in the Korean population, factoring a 30-fold increase in infection rate among students returning to school.
In families with more favorable socioeconomic conditions, children and caregivers need to adapt to a distance-learning model. This can generate increased demands for parents to provide guidance to their children about the excessive use of electronic devices (screen time). It is also important to note that, in many cases, closing schools in less developed countries causes a total shutdown of learning activities, since the socioeconomic reality of a large portion of the population prevents access to distance education projects using the internet.2
In these countries, children have access to a range of playful, evaluative, extracurricular and socialization activities at school, and school closure therefore involves a substantial loss in the teaching/learning and socialization processes. In addition, a number of public policies take place in schools — mainly in public institutions — such as balanced and free food programs, guidance about personal hygiene, sports projects, citizenship incentives, and others.
In a context in which children spend the whole day at home,33 there are increased lonely periods and moments for child self-care. Situations such as these are fragile, particularly for children under 13 years of age who care for younger siblings without assistance from adults, which can cause an increased risk of domestic accidents, serious behavioral impacts and developmental disorders, such as selective mutism, speech delay, social interaction deficits, and others. Other possible consequences of school closures are the possibility that child abuse may remain unreported and that the longer the period of school closures the higher the possibility that the child will never return to school.
There are also nutritional risks and other impacts on children’s growth and development. The literature demonstrates that a lack of basic supplies such as food, water, and clothing causes frustration and has been consistently associated with anxiety, months after quarantine in previous epidemics.13
The causal factors of social contexts already related to dietary errors, child malnutrition, or obesity worsens due to decreased public support for the vulnerable (closures or limited functioning of schools that provide food, NGOs, and popular restaurants) with consequent difficulties with healthy nutrition.
The pandemic, by restricting the maintenance of outside activities and weight loss programs, encourages a sedentary lifestyle due to social distancing and a ban on attending gyms, parks, and leisure areas, alongside an increase in the consumption of canned food (high in sodium) and industrialized foods (with a longer shelf life) containing less essential nutrients for the developing brain, resulting in a negative impact on the growth of children and adolescents.
It is therefore important to anticipate malnutrition and childhood obesity classically associated with a higher incidence of respiratory infections and precarious immune response. In addition, there is a clear tendency for such patients to get worse due to these factors, and this may continue for many months after the pandemic has ended, due to a growing economic crisis and accentuated social vulnerabilities.
In turn, a cross-section of 1319 American adults — including 284 fathers — suggested that 68% of fathers feel closer or much closer to their children since the pandemic.34
This increased involvement with their fathers can have many benefits for kids, including strengthening cognitive and emotional development and increasing the chances of academic and career success and life satisfaction.35
Child toxic stress in previously unstructured homesThe pandemic experience of COVID-19 aggravates the rates of substance abuse, domestic violence, and untreated and pre-existing mental health problems.2 Many caregivers have experienced symptoms of post-traumatic stress, confusion, anxiety, and anger. This leads to caregivers having a greater predisposition to mental health problems, compounded by the reduced availability of elective care, while users of illicit substances face increased levels of stress, and families with a history of domestic violence do not benefit from the supervision of guardianship services.13,36
Issues such as these become even more relevant when analyzing children previously exposed to vulnerable domestic environments and who, through social isolation, are confined full time.37,38 Added to this is the child's inability to access external support networks, such as school, tutoring services, friendly environments, and play activities.
It is thus evident that social isolation should be evaluated as a contributing factor for environments inappropriate to children's mental health. It is also necessary to understand that, in many homes, social isolation amplifies the harmful experiences that the child has faced for a long time, without the possibility of minimizing psychological aggression and resulting in toxic stress. There is therefore an urgent need for psychosocial support, especially for families that had already displayed risk factors for healthy child development prior to the pandemic.
Strategies for preventing health problems and promoting child growth and development
Around the world, millions of children live with ACEs and many adults live with their legacy. Scientific findings suggest that a 10% reduction in ACE prevalence could equate to annual savings of three million disability-adjusted life years (DALYs) or $105 billion. Programs to prevent ACEs and moderate their effects are hugely important, in line with SDG priorities. Rebalancing expenditures towards ensuring safe and nurturing childhoods is economically beneficial and would relieve pressures on healthcare systems.3
Initiatives that have a great impact on the general and mental health of children and adolescents include: public health education and family support strategies; parental training in organizing play, physical activities, a balanced diet, appropriate screen time and content, mindfulness techniques, moments to share anguish, listening time for children, the transmission of a sense of security and resilience, affection, and reciprocity in relationships between parents and children; satisfactory school learning; and specialized treatment for children who suffer toxic stress and its consequences.21,27,29
This systematic review has several limitations. Firstly, due to the immediacy imposed by the COVID-19 pandemic, this study was conducted in mere months. Secondly, the review revealed a scarcity of publications that address the topic of child development and health in epidemic contexts, which reflects the continued inadequate focus on child development and its determinants.
ConclusionsThe COVID-19 pandemic has produced high morbidity and mortality rates within the global population,39 as well as risk factors for healthy growth and development among children. The increase in parental stress, the suspension of classroom activities, social isolation measures, nutritional risks, children’s exposure to toxic stress, especially in previously unstructured homes, and a lack of physical activities are some of the factors found in the literature.
In the face of this pandemic, the creation of activities to promote health and healthy development and prevent toxic stress becomes a priority in order to improve the individual health of children and adolescents and their families, the health of the community, and the intellectual and working capacity of these individuals over the long term, with positive economic and social results for each nation, in order to ensure that the SDGs are fulfilled.
Conflicts of interestThe authors declare no conflicts of interest.
To librarian Marilene da Conceição Felix da Silva, who organized the reference list, and and to Warren Ediger, for grammar and spelling review.