To detect RSV or other thirteen respiratory viruses as possible causer agent of bronchiolitis in infants.
MethodThis is an epidemiological analytical study, conducted using a nasopharyngeal aspirate of 173 hospitalized children younger than two years old with severe bronchiolitis in three hospitals in the Campinas Metropolitan Region (CMR) during 2013-14. The data was statically evaluated by Pearson's chi-squared test with statistical significance of 0.05 and 95% confidence level.
ResultsAs expected, the most prevalent viruses detected were RSV A and B in 47% and 16% of the samples, respectively. However, almost a third of severe bronchiolitis cases there were no detection of RSV, and the viruses more commonly detected were rhinoviruses, which were identified in almost a quarter of all positive samples for at least a viral agent.
ConclusionsAlthough nothing could be concluded from the disease severity and clinical-epidemiological data, the present study's results indicate that severe bronchiolitis is not always related to RSV infections in children younger than two years old, and the rhinoviruses were more prevalent in these cases. These findings reinforce the need to carry out a viral diagnosis in the hospital emergency would be very appropriate for all cases of respiratory infections in children, even for diseases in which the primary etiological agent seems to be well known.
Acute respiratory infections (ARI) are responsible for almost 20% of all deaths of children aged less than five years worldwide.1 Many pathogens can be found in these infections, but viruses seem to be the most common agents. Between them, only the human respiratory syncytial virus (RSV) can produce highly contagious infections in all children younger than two years old.2 The RSV is the primary cause of bronchiolitis, a significant complication of viral ARI in the lower respiratory tract,3 although other pathogens can be found as the cause of this disease without RSV infection.
In Brazil, even with the crescent number of data published in the last decade, much more should be known about the epidemiology of respiratory infections, which is also the leading cause of mortality in children younger than five years old.4 For this reason, the authors described the viral circulation pattern in hospitalized children cases in children younger than two years submitted to oxygen therapy due to severe bronchiolitis. The data factor three hospitals from Campinas Metropolitan Region (CRM) during 2013-14 and the clinical-epidemiological factors were evaluated to identify if there was any correlation between the epidemiological characteristic and the severity of the disease.
Material and methodsEthical statementThe research was approved by the National Research Ethics Commission (approval number CAAE: 00869612.7.0000.5404). According to supplementary material, the patients' legal representatives received all the explanations about the research and signed the "Informed Consent Form".
Study population and clinical-epidemiological dataChildren younger than two years old hospitalized with severe acute bronchiolitis requiring oxygen therapy in three hospitals located in the Campinas area, São Paulo State – UNICAMP Clinical, Vera Cruz, and Sumaré State Hospitals, during the years 2013 and 2014, were included in this study. Some epidemiological indices were recorded by the pediatric team from each hospital (gender, age, prematurity, history for atopy). Clinical conditions were followed using hospitalization time data, oxygen therapy time, time of Intensity Center Unity (ICU) admission if required, mechanical ventilation time if required, and evolution to death.
Samples processing and molecular testsNasopharyngeal aspirates were collected and immediately immersed in RNAprotect® Cell Reagent (Qiagen, CA, USA). The samples were stored at 4°C for up seven days in the hospital and then, when transferred to the lab, were stored at −80°C until their processing. The molecular assays were conducted at Laboratory of Animal Virology, Department of Genetics, Evolution, Microbiology and Immunology, Institute of Biology, University of Campinas (UNICAMP), Campinas-SP, Brazil. The samples were submitted to centrifugation before processing. The genetic material, DNA and RNA, were extracted using an Allprep DNA RNA kit (Qiagen, CA, USA) and the cDNA synthesis was conducted using a High-Capacity cDNA Reverse Transcription Kit (Applied Biosystems, CA, USA), both according to manufacturers’ instructions.
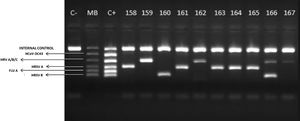
The Seeplex® RV15 ACE Detection Kit (Seegene, MD, USA) was used for viral detection, a qualitative test that detects fifteen different respiratory viruses in three sets, A, B, and C (set A: AdV A/B/C/D/E, CoV 229E/NL63, PIV1, 2 and 3; B: CoV OC43, RV A/B/C, RSV A and B, FLU A; C: BoV 1/2/3/4, FLU B, MPV, PIV 4, EV). All reactions were conducted according to manufacturers’ instructions. PCR products were visualized in 2% agarose gel containing GelRed (Biotium®) under ultraviolet transillumination. The expected size of the PCR bands was, in base pairs, according to Table S1.
Statistical analysisThe clinical-epidemiological factors were submitted to statistical analysis using Pearson's chi-squared test. The p-value lower than 0.05 were considered significant.
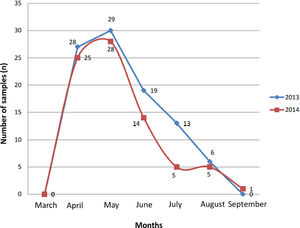
ResultsSamplesOne hundred seventy-three (173) hospitalized infants between March/2013 and September/2014 in three hospitals from Campinas Metropolitan Region (CRM) were included in the present study. According to Figure 1, the seasonality of hospitalizations was recorded in April and May in both years and remained high throughout late fall and until mid-winter, the dry season in the CRM.
Distribution of acute respiratory infections (ARI) (n) by months of 173 children younger than two years old with bronchiolitis hospitalized in three different hospitals (107, 43 and 23 from UNICAMP Clinical, Vera Cruz and Sumaré State Hospitals respectively) in 2013 and 2014 from Campinas Metropolitan Region, São Paulo State, Brazil.
The main clinical-epidemiological data related to the present study's population were summarized in Table 1. Risk factors such as premature birth (less than 37 weeks of gestation) and atopy family history were reported more frequently. Regarding the clinical progression of patients, the average time of hospitalization was 8.83 days, ranging from 1 to 64 days. The oxygen therapy time ranged from 1 to 63 days, with a mean of 7.23 days. 37 (21.3%) patients required mechanical ventilation, and 59 (34.11%) were admitted to the ICU. Of those in ICU, mechanical ventilation ranged from 2 to 37 days with an average of 8.9 days, and the time in ICU was on average 9.2 days, ranging from 2 to 37 days. Five children (2.89%) passed away due to complications related to severe bronchiolitis; in these patients, human rhinovirus (2), human respiratory syncytial virus type A (2), and meningitis (1) were identified. Even though the number of deceased patients is not representative (only 5), 40% of deaths were recorded in patients who had RV infections. The statistical analysis indicated that there was an association between the disease's severity and these related epidemiological factors.
Clinical-Epidemiological factors described of hospitalized children due to acute respiratory infections and bronchilitis in three hospital (UNICAMP Clinical, Vera Cruz and Sumaré State Hospitals) from Campinas Metropolitan Region, São Paulo State, Brazil.
Of 173 samples submitted to PCR reactions, more than 87% (151) samples were positive for one or more viruses, and only 8 in 2013 and 14 in 2014 were negative (22 in total). Figure 2 shows the electrophoresis gel of 10 samples (158 to 167) evaluated for set B, indicating the profile of bands and suggesting the high viral load even in cases in that co-detections (two or more bands in the same column) were recorded. Regarding positivity, the most prevalent virus was RSV A, detected in 91 of 151 positive samples, followed by 46 RV A/B/C and 41 RSV B. Other viruses also were identified in some samples and CoV-OC43, PIV 2, and FLU B was not identified in any sample. The viruses' distribution by year and their co-detection with others is available in Table 2. In 2013, RSV A was predominant, but the RV also presented a high number of detections. In 2014, RSV A continued to be the most prevalent but in a lower amount than 2013. Another relevant discovery was that in a quarter of the samples, two or three viruses were co-detected, most commonly the RV and RSV. The data related to co-detection was summarized in Table 2.
Agarose gel image (2%) highlighting the viewing standard of the results. Molecular Weight Marker (MB) corresponds to the pattern used in set B to identify 5 different species of viruses. In this case, 4 positive samples for RV A/B/C (159, 162, 166 and 167), 5 positive samples for RSV A (158, 161, 163, 164 and 165) and 2 positive samples for RSV B (160 and 166). Note: the sample 166 presented co-detection with RV A/B/C and RSV B.
Positivity of viral species detected in nasopharyngeal aspirates from 151 children hospitalized by acute respiratory infections and bronchiolitis in three hospitals (UNICAMP Clinical, Vera Cruz and Sumaré State Hospitals) from Campinas Metropolitan Region, São Paulo State, Brazil. The positive samples were stratified by viral specie (12 viral species detected), a number of viral species by sample (single, double or triple detection in each sample), and year of collection (2013 and 2014).
Severe bronchiolitis is characterized by intense inflammation, edema, and necrosis of epithelial cells of the airway. In general, it has been associated with RSV infections, single or joined to other viral pathogens, in special RV.5,6 There is a significant impact on public health because, in many cases, the children affected by this disease can develop respiratory insufficiencies throughout their whole life.
The respiratory viruses’ assessment using molecular tests has allowed the best understanding of bronchiolitis.7 The present study was conducted in three hospitals in the 10th largest metropolitan region from Brazil during the summer end of 2013 and the beginning of spring 2014 (two consecutive falls and winters). This area is crucial epidemiologically because it is almost 100 kilometers from Brazil's most extensive metropolitan region – São Paulo – and in these places, two main Brazilian international airports are located. This study registered, by PCR, the viral epidemiological profile of 173 ARI cases in infants. For the laboratory assays, the present study's samples were stored at 4°C for up seven days until being processed. Despite the RNA preservative addition, the storage time was considered extensive, suggesting that RNA degradation might have happened, especially in samples with low viral load, and it could have influenced the authors’ limit of detection. However, in RSV infections, the high viral load seems to be more associated with severe disease,3 and then this procedure could not strongly affect the results since the present study's population was composite just by severe cases of bronchiolitis.
The present study's data indicated that the hospitalization rate occurred due to viral infections since that 87% of the samples presented one or more viruses detected. In addition, the circulation of these viruses was recorded mainly in the months of April and May, which correspond at the beginning of the cold and dry season, a critical period for respiratory infections in many regions of Brazil,8 including the CMR. There were fewer cases in 2014 (78 compared to 95 in 2013) when higher temperatures were recorded throughout the year compared to 2013. Gardinassi et al.9 also identified meteorological factors such as temperature and relative air humidity directly influencing the viruses' circulation pattern. They described an epidemiological profile of eight respiratory viruses' species, including RSV and RV, in hospitalized children at São Jose do Rio Preto, a city with similar weather to the CRM area, and concluded that the dry seasons provided a predisposition to the transmission and viral infections effectiveness. These findings also were observed in the present work. This drier and colder period causes the airways to dry out; this dryness associated with the behavioral habit of staying in closed and poorly ventilated environments in a low-temperature shelter favors viral spread, especially in people with a developing immune system, such as children, or weakened, such as elderly or immunocompromised patients.
The RV has been frequently associated with respiratory infections10 and is phylogenetically classified as A, B, and C,11,12 presenting an extensive genetic diversity (more than 150 strains according to Chen et al.13 Previously, the subtype C was described as more pathogenic between them; however, other studies have indicated that this characteristic is controversial.11,14 According to data presented by Watanabe et al.,15 these viruses were detected in 28.6 % of evaluated samples; furthermore, the high frequency of this species of pathogen has been associated with the high demand by the healthcare system, mainly in the ARI season in Brazil. In the South Brazilian region, the RV was detected in 17% of samples from infants younger than six months old hospitalized due to acute bronchiolitis.16
Other developing countries such as South Africa17 also have reported RV in a quarter of hospitalized patients with severe ARI; Simusika et al.18 found this virus in 22.1% co-detection in Zambia. Van der Zalm et al.19 discussed a relevant point in their longitudinal study that the RV is predominantly prevalent in young children, which can be associated with the substantial diversity of subtypes. They found RV in 37% of the evaluated samples, and between them, they identified an impressive amount of 27 different subtypes. Additionally, an average of three subtypes was identified in samples from each patient. This average suggests that the abundant diversity of subtypes may not induce cross-immunity. During the development and maturation of the immune system in the early stages of childhood, recurrent infections by different subtypes appear to cause more severe clinical conditions.
It seems to be increasingly clear that rhinoviruses have been critical etiologic agents of severe bronchiolitis in Brazil. However, other viruses were already related in patients with bronchiolitis, including MPV, CoV, BoV, FLU, AdV, and PIV.3 The present study's results showed that one-third of bronchiolitis cases were associated with other respiratory viruses (RV, EV, BoV, PIV 1, 3 and 4, FLU A and coronaviruses CoV 229E / NL63). As shown in the present study's results, despite other viruses having been identified in minor proportions, their importance should be highlighted, whether in cases of single infection or co-infection. For the control and prevention of this significant pathology, the focus must be maintained on the various viruses involved, and not only on RSV, as it has been discussed before. Previously, most of the research was mainly focused on identifying RSV, so other viruses have often not been considered. Nevertheless, with the evolution of the diagnosis tools, like a commercial panel of PCR including several viral species, it became possible to identify the presence and emphasize the importance of the others in the epidemiology of infectious diseases like ARI.
Further than all these RNA viruses as the causer of severe ARI in children, although in a small percentage, the DNA virus BoV has been detected in severe cases as bronchitis, bronchiolitis, and pneumonia20 in the CMR. Their infections presented similar symptomatology as other viral respiratory infections, including fever, cough, and wheezing.21 Del Rosal and coworkers22 reported that the BoV could represent a critical epidemiological respiratory pathogen, especially for infants younger than six months old. In Brazil, BoV has been identified in up to 13.2%23 of the samples, and most of the cases seem to be associated with co-detection (in 83% of the cases, according to data published by Del Rosal et al.).22
Co-detections can be important as and additional data for clinical evolution. The most common co-detection was between RV and RSV A or B in patients with associated risk factors, but none with a tendency towards greater or lesser severity, according to other studies.6,24 However, greater severity in cases of multiple infections has been previously shown.25,26 The present study's results indicated that 37 of 151 positive samples presented co-detection between two or three viruses, at a significant proportion between RV and RSV. According to other reports, these patients presented many associated risk factors that should be associated with greater severity.25-27 However, this fact did not occur in the present study's population, and similar data has been reported by other researchers.6,24 Nothing could be concluded from the disease severity and clinical-epidemiological data. For example, one patient who had no associated risk factor presented severe disease, and in his samples was identified a co-detection of two viruses. These findings indicated that severe bronchiolitis seems to present multifactorial causes, at least according to the data obtained by the present study.
The present study's samples were collected primarily on the HC-UNICAMP (107/173) from patients users of the Brazilian Unified Health System (SUS), a free access health system maintained by the federal government. Furthermore, this is a school hospital where research and attention to the population have been a common practice. That said, in the Brazilian hospital routine, the molecular diagnosis was not a standard tool before the COVID-19 pandemic, mainly due to scarce financial resources and the necessity of high investment in equipment and people trained to carry tests out. However, it has become even more apparent that molecular diagnosis is an essential diagnostic tool for epidemiological surveillance, mainly to detect the actual causal agent of respiratory infections diseases.
The present study's results indicate that one-third of bronchiolitis was not related to RSV infections. Another important virus detected in severe cases of bronchiolitis was the RV or its co-detection with RSV. These findings reinforce the need to carry out a viral diagnosis in the hospital emergency would be very appropriate for all hospitalized children, even for diseases in which the primary etiological agent seems to be known.
FundingThis work was supported by the FUNCAMP (Unicamp Development Foundation), FAPESP (São Paulo Research Foundation), and CNPq (National Council for Scientific and Technological Development).
The authors are very grateful to the pediatrics team from the three hospitals included in the present study to support the samples’ collection and access to patient records and to the biologist Eduardo Luis Costa Lobo Benfatti, for critical reading and English revision of this manuscript.