Describe the results of the red reflex test in full-term newborns, as well as identify factors associated with red reflex test outcome and compare hospital length of stay between patients with inconclusive and normal red reflex test results.
MethodsDescriptive cross-sectional study of the results of the red reflex test performed in a tertiary hospital maternity unit between 2014 and 2018. A nested case-control study was also performed to search for anthropometric, gestational, and neonatal variables associated with the outcome of the red reflex test.
ResultsThere were121 identified cases of inconclusive red reflex test in 11,833 newborns. Sixteen alterations were confirmed, four considered severe: two cases of congenital glaucoma, one of cataract, and one of coloboma. Mean birth weight (p=0.04), length (p=0.03), and head circumference (p=0.02) were lower in patients with inconclusive red reflex test; however without a relevant effect size (d=−0.21, −0.22, and −0.25, respectively).The proportion of white, mixed-race, and black patients was significantly different between the groups (p<0.001), with a higher chance of inconclusive results in mixed-race (OR=2.22) and black (OR=3.37) patients when compared to whites. An inconclusive red reflex test led to an increase in hospital length of stay from 62 to 82hours (p<0.001).
ConclusionsThe red reflex test was able to identify four severe alterations in 11,833 newborns (0.03%). In the 121 newborns in which the red reflex test was classified as inconclusive, there was a 20-hour increase in the hospital length of stay, but a severe alteration was confirmed in only 3.3% of them. Differences in red reflex between white, mixed-race, and black patients should be considered.
Descrever os resultados do teste do reflexo vermelho em recém-nascidos a termo. Identificar fatores associados ao resultado do teste do reflexo vermelho e comparar o tempo de internação entre pacientes com teste do reflexo vermelho duvidoso e normal.
MétodosEstudo transversal descritivo dos resultados do teste do reflexo vermelho feito em maternidade de hospital terciário entre 2014 e 2018. Foi ainda feito estudo de caso-controle aninhado para pesquisa de variáveis antropométricas, gestacionais e neonatais associadas ao resultado do teste do reflexo vermelho.
ResultadosForam identificados 121 casos de teste do reflexo vermelho duvidoso em 11.833 recém-nascidos. Foram confirmadas 16 alterações, 4 consideradas graves: 2 casos de glaucoma congênito, um de catarata e um de coloboma. As médias de peso de nascimento (p=0,04), comprimento (p=0,03) e perímetro cefálico (p=0,02) foram menores nos pacientes com teste do reflexo vermelho duvidoso, entretanto sem um tamanho de efeito relevante (d = -0,21; -0,22 e -0,25; respectivamente). A proporção de pacientes brancos, pardos e negros foi estatisticamente diferente entre os grupos (p<0,001), com maior chance de resultado duvidoso para pardos (OR=2,22) e negros (OR=3,37) em comparação a brancos. O teste do reflexo vermelho duvidoso levou a um aumento no tempo de internação de 62 para 82 horas (p<0,001).
ConclusõesO teste do reflexo vermelho foi capaz de identificar 4 alterações graves em 11.833 recém-nascidos (0,03%). Nos 121 recém-nascidos em que o teste do reflexo vermelho foi classificado como duvidoso, houve aumento de 20 horas no tempo de internação hospitalar, porém se confirmou alteração grave em apenas 3,3% deles. Diferenças no reflexo vermelho entre brancos, pardos e negros devem ser consideradas.
Although childhood visual impairment (VI) accounts for only approximately 6% of VI cases worldwide,1 its importance should not be underestimated. The number of “years of blindness” in children with VI equals that of adults with cataracts.2 Vision is a crucial sense in childhood, so VI affects the patient's neuropsychomotor development and educational needs.3 The number and duration of hospitalizations are higher in children with VI.4 Mortality in children with VI is higher than in those with preserved visual function, and VI, even in the absence of other comorbidities, has been implicated as a predictor of death.3
Early diagnosis of childhood VI is of the utmost importance. Visual maturation occurs mostly up to 5 years of age, concomitantly with eye and brain development.5 Therefore, there is a critical period in which the visual system must be intact and during which interventions are more likely to result in visual improvement.6 Although there is evidence supporting the late treatment of amblyopia (unilateral or bilateral reduction of visual acuity secondary to insufficient or inadequate visual stimulation during the critical period),7 it is known that the visual system gradually becomes less responsive and the benefit of interventions is progressively reduced.6,8
The red reflex test (RRT), also known as the “red eye reflex test,” is recommended for the screening of childhood eye alterations by several societies, including the American Academy of Pediatricians and the Brazilian Society of Pediatrics.9,10 In Brazil, the RRT is mandatory while the newborn (NB) is still at maternity hospital in some states and there is pending legislation to require RRT in all NBs nationally.11
The RRT should be performed in a dark environment and the source of light should be projected simultaneously on both eyes of the patient. The reflexes of each eye should be compared and evaluated for brightness, size, and color. The RRT is classified as normal, inconclusive, or altered; the last two outcomes require subsequent evaluation. The absence of reflection, a white or yellow reflex, as well as the observation of substantial differences between the eyes, are indicative that there may be some eye alteration and constitute criteria for referral to an ophthalmologist.12
The RRT is described as a rapid and painless test. However, patients with suspected alterations should undergo a detailed, more invasive and pain-associated ophthalmologic assessment.13 Additionally, information from an apparently altered test in the NB and the waiting period for ophthalmologic assessment may lead to emotional stress and even increased length of hospital stay, which in turn leads to increased risk of nosocomial infections and costs.14 Therefore, the identification of factors that may be associated with an increase in the number of false positives from the RRT is pertinent.
Despite its importance and broad recommendation, the results of the RRT are scarce in the literature.15–17 The Hospital de Clínicas de Porto Alegre (HCPA) is a tertiary university hospital that performs the RRT in all NBs before hospital discharge. The present study was carried out with the objective of analyzing the results of the hospital screening program, as well as identifying non-ocular factors that may be related to an inconclusive RRT.
Patients and methodsPopulationA retrospective evaluation of patients born in the hospital between January 1, 2014 and January 31, 2018 was performed. All NBs undergo RRT before hospital discharge and inconclusive or altered cases are evaluated by an ophthalmologist during the hospital stay.
All neonates born during the study period who were under rooming-in care were included. The patients were divided into two groups:
Inconclusive RRT group: all patients with RRT classified by the pediatrician as inconclusive or altered.
Control group: consisted of a sample of NBs with normal RRT.
There was no matching and the medical records of all NBs were randomly organized in an Excel (Microsoft Corporation®, Excel, WA, USA) spreadsheet using the “RANDOM ()” command; then the first 450 were selected. Of these, two were part of the “inconclusive RRT” group and another five were excluded due to admission at the semi-intensive therapy unit before discharge.
Patients requiring intensive or semi-intensive care unit admission, as well as those with incomplete medical records, were excluded.
Sample sizeThe period to be studied was defined by the availability of information regarding ophthalmologic consultations in computerized medical records at the HCPA. The inclusion of four controls for each case was established for the case-control study.
A total of 564 NBs were included (121 patients with inconclusive RRT and a sample of 443 individuals with normal RRT), which provided the study with a statistical power of 83% to detect a difference of 0.3 standard deviations between the means of epidemiological and anthropometric variables analyzed between the groups. The level of significance was set at 0.05.
Study designThis is a descriptive cross-sectional study of RRT results and subsequent ophthalmologic evaluation. A nested case-control study was also performed. The result of the RRT was considered an outcome and the anthropometric, neonatal, and gestational variables were considered as predictors.
RRT and ophthalmologic evaluationThe RRT was performed by resident physicians in pediatrics under the supervision of professors. The protocol recommends that it be performed in a dark environment with the ophthalmoscope lens diopter set at “0″ and that the light be projected simultaneously on both eyes of the subject, at a distance of approximately 45cm. The absence of reflex in one or both eyes, the observation of a white or yellowish reflex, dark spots in the reflex, as well as the existence of asymmetry between the eyes constitute criteria for referral to the ophthalmologist.
The ophthalmologic examination was performed after pharmacological mydriasis with 0.5% tropicamide. Patients were submitted to indirect binocular ophthalmoscope evaluation for ocular media opacities (cornea, aqueous humor, crystalline, and vitreous humor), as well as the assessment of fundus structures.
Ophthalmological alterations were considered severe when they required surgical intervention or outpatient follow-up.
Ethical considerationsThis study was approved by the Research Ethics Committee of the institution. This research did not receive any specific grants from public, commercial, or nonprofit funding agencies.
Statistical analysisThe normality of the samples was evaluated using the Shapiro-Wilk test. Continuous variables are expressed as means and standard deviations, and categorical variables as counts and percentages. The percentages—with their respective 95% confidence intervals—were presented for the descriptive results. Student's t-test was used to compare the means of continuous variables between the groups and the chi-squared test or Fisher's exact test to compare categorical variables. Association measures between variables and groups were calculated, expressed as odds ratios (OR) with 95% confidence intervals (95% CI) for categorical variables and Cohen's d statistics for continuous variables. A significance level of 5% was adopted in all analyses. Data were analyzed using SPSS (SPSS Statistics for Windows, version 22.0. Armonk, NY, USA).
ResultsA total of 13,296 records of patients born in the HCPA were identified during the study period who were under rooming-in care. Of these, 1301 were excluded for admission at the semi-intensive care or the intensive care unit, and 162 due to missing or discrepant information in the medical records. The study flowchart is shown in Fig. 1.The authors identified 121 cases of inconclusive RRT among 11,833 NBs during the study period, which corresponds to 1.0% (95%CI: 0.8–1.2). After the ophthalmologic evaluation, 16 cases of alterations were confirmed (13.2% [95% CI: 7.7–20.6] among the suspected cases and 0.14% [95% CI: 0.09–0.23] of the total number of patients). Retinal hemorrhage was the most frequently observed alteration, being identified in 12 of the patients; it did not require follow-up in any of them. Four cases of severe eye alterations were identified (3.3% [95% CI: 0.9–8.2] of suspected cases and 0.03% [95% CI: 0.01–0.09] of the total number of patients). The two patients with congenital glaucoma were submitted to surgical procedure before hospital discharge, and the patient with congenital cataract was discharged and submitted to surgical procedure in the 4th week of life. The case of iris coloboma and choroid was referred for outpatient follow-up.
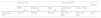
Anthropometric, gestational, and neonatal variables of the inconclusive RRT and control groups are shown in Table 1. Patients in the two groups did not differ significantly regarding gender (p=0.53), weight adequacy (p=0.32), type of delivery (p=0.38), gestational age (p=0.31), and Apgar score at the 1st (p=0.11) and 5th (p=0.45) minutes.
Characteristics of individuals from inconclusive RRT and control groups.a
| Characteristic | Inconclusive RRT n=121 | Control n=443 | pb |
|---|---|---|---|
| Male gender, n (%) | 64 (52.9) | 218 (49.2) | 0.53 |
| Birth weight, g | 3,190±450 | 3,290±480 | 0.04 |
| Weight adequacy, n (%) | 0.32 | ||
| SGA | 18 (14.9) | 47 (10.7) | |
| AGA | 97 (80.1) | 360 (81.8) | |
| LGA | 6 (5.0) | 33 (7.5) | |
| Length, cm | 48.2±2.1 | 48.7±2.3 | 0.03 |
| Head circumference, cm | 33.6±1.5 | 34.0±1.6 | 0.02 |
| Ethnicity, n (%) | < 0.001 | ||
| White | 55 (45.4) | 305 (68.8) | |
| Mixed-race | 33 (27.3) | 83 (18.7) | |
| Black | 33 (27.3) | 55 (12.4) | |
| Vaginal delivery, n (%) | 78 (64.5) | 305 (68.2) | 0.38 |
| Gestational age, wks. | 39.4±1.6 | 39.2±1.5 | 0.31 |
| Apgar 1min, n (%) | 0.11 | ||
| <4 | 1 (0.8) | 4 (0.9) | |
| 4–6 | 9 (7.4) | 14 (3.2) | |
| ≥7 | 111 (91.7) | 425 (95.9) | |
| Apgar 5 min, n (%) | 0.45 | ||
| <4 | 0 (0.0) | 0 (0.0) | |
| 4–6 | 0 (0.0) | 2 (0.5) | |
| ≥7 | 121 (100.0) | 441 (99.5) | |
| Length of stay, h | 81.8±37.4 | 61.7±29.1 | < 0.001 |
RRT, red reflex test; SGA, small for gestational age; AGA, adequate for gestational age; LGA, large for gestational ag.
The mean birth weight (p=0.04), length (p=0.03), and head circumference (p=0.02) were lower in the inconclusive RRT group compared to controls, but without a relevant effect size (d=−0.21; −0.22, and −0.25; respectively). Mixed-race and black patients had their RRT results classified as inconclusive more often than whites (Table 2), with an OR=2.22 (95% CI: 1.35–3.65) for mixed-race vs. white and 3.35 (95% CI: 1.99–5.64) for black vs. white patients (p<0.001).Although non-whites had proportionally more inconclusive RRTs, all severe alterations were identified in white patients, and there was a statistically significant difference between them (0/66 vs. 4/55, p=0.03).
An inconclusive RRT led to a 20h increase in average hospital length of stay (61h vs. 81h, p<0.001).
DiscussionVinekar et al.18 examined 1021 full-term NBs using a RetCam (Massie Research Laboratories, Inc –Dublin, California, USA), a digital camera capable of documenting eye structures, and found severe alterations (requiring medical care or surgical intervention) in 0.9% of cases, including one patient with retinoblastoma. Li et al.19 performed RetCam evaluation on 14,786 individuals and identified eye alterations in 2% (excluding cases of retinal hemorrhage), including treatable retinal diseases, 11 cases of congenital cataract, three cases of retinoblastoma, in addition to eye abnormalities that may be associated with systemic diseases such as microphthalmia and congenital optic nerve anomalies. Wasilewski et al.,20 in a prospective study in which ophthalmologists evaluated 667 NBs in the maternity ward, identified ocular alterations in 25 (3.75%). It is noteworthy that in 56% of patients with altered ophthalmologic examination, the pediatrician did not identify any abnormality on the routine examination. It should be noted that although some of these alterations were not of major relevance for neonatal screening, there was one case of iris coloboma and choroid, and two cases of congenital cataract, severe conditions that could lead to blindness.
Among 7641 NBs in whom ophthalmic alterations identified with RRT or RetCam were compared, the sensitivity of RRT for anterior and posterior segment alterations was 99.6% and 4.1%, respectively.21
It should be recalled that, although more than 80% of the abnormalities undetected by the RRT in the posterior segment were retinal hemorrhages, most of which have an excellent prognosis,22 some alterations with treatment indication were not identified, including one case of retinoblastoma, which can be fatal.
Regarding specifically the retinoblastoma detection with RRT, the test was unable to detect abnormalities in all 13 eyes with lesions in the study by Khan and Al-Mesfer23 and, without pharmacological mydriasis, it identified leukocoria in only three of ten eyes with tumors in the evaluation by Canzano and Handa.24
Of 11,500 patients submitted to RRT in the maternity unit of an Israeli university hospital over a period of two years,16 12 (0.1%) suspected cases were identified. They underwent ophthalmologic evaluation, which diagnosed congenital cataract in five of them. Another evaluation,15 carried out in Italy, applied RRT to 22,272 NBs and found 461 (2.1%) suspected or altered cases. Of these, three had confirmation of severe eye alterations, which comprised two cases of cataract and one retinoblastoma.
The present study, carried out in the maternity unit of a tertiary university hospital, identified 121 (1.0%) cases of suspected RRT in 11,833 NBs. Of these, severe alterations were confirmed in four (3.33% of suspected cases and 0.03% of total NBs), a result close to that found in the Italian study,15 but with the identification of considerably fewer severe cases when compared to reports of global ophthalmologic evaluation, most of them performed with a RetCam.18–20
Despite the small number of identified severe alterations, the importance of making an early diagnosis should be stressed. Three of the four patients underwent surgery in the neonatal period, which is crucial for the prevention of blindness, and which would hardly have been possible without the identification of alterations by the RRT. In this sense, an evaluation performed in Sweden showed that performing the RRT at the maternity hospital increased by more than three-fold the number of patients with a diagnosis of cataract.25
Patients submitted to ophthalmologic evaluation due to inconclusive RRT had a 30% increase in hospital length of stay. Considering that 97% of them did not have any severe alterations, measures to reduce the number of false positive results should be evaluated.
The mean birth weight, length, and head circumference were statistically lower in the inconclusive RRT group when compared to controls, but without showing good discriminatory power between the groups. However, there was a statistically and clinically significant difference in the distribution of ethnic groups, with a higher proportion of mixed-race and black patients among NBs with inconclusive RRT. These patients corresponded to 55% of the suspected cases and there were no confirmations of severe ocular alteration.
Attention should be paid to differences in red reflex between white individuals and those with darker skin pigmentation, which is also associated with increased intraocular structure pigmentation and, consequently, darkening or attenuation of the red reflex. One possibility to be considered in inconclusive cases is the repetition of RRT after pharmacological mydriasis, which may facilitate the observation of the red reflex.
This study has some limitations. No routine refraction was performed in NBs assessed by ophthalmologists, which could have justified some cases of inconclusive RRT, as high refractive errors may cause red reflex alterations. Moreover, the fact that only NBs with inconclusive RRTs were evaluated by ophthalmologists makes it impossible to adequately estimate their accuracy.
Considering the implications of an early diagnosis of eye alterations, including the possibility of visual rehabilitation and the identification of both systemic comorbidities and potentially fatal diseases such as retinoblastoma, neonatal ophthalmologic screening is relevant. Ophthalmologic screening strategies with RetCam, performed experimentally,18,19 have diagnosed eye diseases in a considerably larger number of NBs compared to RRT, but their use is limited by practical (mainly due to the need for pupillary dilation and contact with ocular surface) and financial reasons.
Thus, the RRT is a practical, fast, and inexpensive test, which allows its performance in a large number of patients. Results of the use of the RRT in maternity hospitals are still, however, scarce. The comparison of a neonatal examination performed by an ophthalmologist (which although difficult to accomplish in terms of public health, is more accessible than using the RetCam) with the pediatric RRT should be considered. It is suggested that further research be directed towards the definition of the accuracy and cost-effectiveness of the test, with particular concern for its sensitivity.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Baldino VM, Eckert GU, Rossatto J, Wagner MB. Red reflex test at the maternity hospital: results from a tertiary hospital and variables associated with inconclusive test results. J Pediatr (Rio J). 2020;96:748–54.
This study was carried out as a requirement to obtain a Master's Degree from the Programa de Pós-Graduação em Saúde da Criança e do Adolescente, Faculdade de Medicina, Universidade Federal do Rio Grande do Sul (UFRGS), Porto Alegre, RS, Brazil.