To describe and analyze the prognosis of children during the first year of life with a diagnosis of congenital diaphragmatic hernia admitted between the years 2005 and 2015 in the Neonatal Intensive Care Unit.
MethodIn a retrospective cohort, 129 children with a diagnosis of congenital diaphragmatic hernia were studied. The prognostic factors were analyzed, whereupon prenatal, delivery, and postnatal exposure variables were associated with death during the first year of life. The odds ratio and the confidence interval (95% CI) were calculated for all the studied variables, using the chi-squared test and Student's t-test.
ResultsThe study included 129 children hospitalized from January of 2005 to December of 2015. Seventy-nine (61%) patients died, 50 survived, and 33 had other associated malformations. Among the prognostic factors, the following were significant and increased the chance of death: polyhydramnios (p=0.001), gestational age of the earliest diagnosis (p=0.004), associated congenital abnormalities (OR: 3.013, p=0.022), pO2 of the first gasometry (p=0.000), pCO2 of the first gasometry (p=0.000), presence of pulmonary hypoplasia (OR: 3.074, p=0.000), use of preoperative vasoactive drugs (OR: 2.881, p=0.000), and use of nitric oxide (OR: 1.739, p=0.000). The presence of only intestines in the hernia content was a protective factor (OR: 0.615, p=0.001).
ConclusionThe mortality in the first year of life in patients with congenital diaphragmatic hernia in this study was 61% in the years 2005–2015. Among the prognostic factors that demonstrated a significant effect, pulmonary hypoplasia had the greatest impact.
Descrever e analisar o prognóstico de crianças ao longo do primeiro ano de vida com diagnóstico de hérnia diafragmática congênita admitidas entre 2005 e 2015 na Unidade de Terapia Intensiva Neonatal.
MétodoEm uma coorte retrospectiva estudamos 129 crianças com diagnóstico de hérnia diafragmática congênita. Foram analisados os fatores prognósticos onde as variáveis de exposição do pré-natal, parto e pós-natais foram associadas ao óbito no primeiro ano de vida. Calculamos a odds ratio (OR) e o intervalo de confiança (IC95%) para todas as variáveis estudadas, sendo utilizados os testes de qui-quadrado e o teste T Student.
ResultadosForam incluídos no estudo 129 crianças, internados de janeiro/2005 a dezembro/2015. Foram a óbito 79 (61%) pacientes, 50 sobreviveram e 33 tinham outras malformações associadas. Entre os fatores prognósticos foram significativos e aumentaram a chance de óbito a polidrâmnia (p=0,001), idade gestacional do diagnóstico mais precoce (p=0,004), anomalias congênitas associadas (OR: 3,013, p=0,022), pO2 da primeira gasometria (p=0,000), pCO2 da primeira gasometria (p=0,000), presença de hipoplasia pulmonar (OR: 3,074, p=0,000), uso de drogas vasoativas pré-operatórias (OR: 2,881, p=0,000) e o uso de oxido nítrico (OR:1,739, p=0,000). A presença de apenas intestinos no conteúdo da hérnia foi um fator protetor (OR: 0,615, p=0,001).
ConclusãoA mortalidade no primeiro ano de vida em portadores de hérnia diafragmática congênita, neste estudo, foi de 61% de 2005 a 2015. Entre os fatores prognósticos que demonstraram um efeito significativo, a hipoplasia pulmonar foi o de maior impacto.
Congenital diaphragmatic hernia (CDH) is associated with a failure in the fusion of the caudal pleuroperitoneal membranes that form the diaphragm, resulting in a defect of continuity, with potential thoracic migration of the abdominal structures under formation, resulting in compression of the lungs and, consequently, pulmonary underdevelopment, which can lead to the newborn's death.1–3 The incidence of CDH ranges from one in 2500 to one in 4000 live births, representing 8% of the major congenital anomalies. In Brazil, 1011 CDH cases were recorded in 2014, according to data from DATASUS4,5; however, the mortality rate due to this disease remains unknown.
Technological advances in the last 30 years have aided prenatal diagnosis, intrauterine surgery, and neonatal clinical and surgical management. Available technological advances such as high-frequency ventilation, mechanical ventilation, conventional and cycled CPAP (continuous positive airway pressure), and Oxyhood for the treatment of CDH infants have allowed newborns to maintain hemodynamic stability until it becomes possible to perform the surgical repair and increase survival; however, the mortality rate still remains significant when compared to other congenital anomalies. In addition to advances in the neonatal field, the development of fetoscopic surgery for tracheal occlusion has allowed the survival of many severe cases. There are still few studies in Brazil about the prognostic factors associated with the mortality of newborns with CDH in the first year of life, thus it being necessary to determine them, allowing for advanced support during the care of the newborns.6
Therefore, the aim of this study was to describe and estimate the mortality rate and associated prognostic factors in the first year of life of newborns with a diagnosis of congenital diaphragmatic hernia, in the years 2005–2015.
MethodsThis was a retrospective cohort study of children with CDH admitted to Instituto Fernandes Figueira (IFF/Fiocruz), located in the state of Rio de Janeiro, which is a referral center for high-risk pregnancies and fetal congenital anomalies.
The inclusion criteria included all infants born at Instituto Fernandes Figueira with a diagnosis of congenital diaphragmatic hernia during the years 2005–2015. The exclusion criteria comprised newborns transferred or hospitalized only to undergo the postnatal surgery, due to the absence of prenatal and delivery data.
Data collection was carried out based on the review of medical records from the beginning of the follow-up at the Fetal Medicine Outpatient Clinic to the discharge from the Neonatal Intensive Care Unit (NICU), and the analyzed prognostic factors were divided into two groups: antenatal and those from the period of hospitalization in the Neonatal Intensive Therapy Unit. The antenatal data consisted of gestational age at the time of diagnosis by ultrasonography, gestational age at birth according to Ballard, newborn's gender, birth weight, type of diaphragmatic hernia (left and right), congenital anomalies, early neonatal death, late neonatal death, mortality, postnatal death, amount of amniotic fluid (polyhydramnios, oligohydramnios, anhydramnios, and normohydramnios), delivery route (vaginal or caesarean section), (altered) karyotype result, intrauterine surgery, Apgar score, and arterial blood gas analysis (pO2 and pCO2).
The prognostic factors of the hospitalization period in the NICU included data regarding transient tachypnea of the newborn, hyaline membrane disease, pulmonary hypoplasia, suspected sepsis, confirmed sepsis, bronchopulmonary dysplasia, PDA (patent ductus arteriosus), vasoactive pre- and postoperative vasoactive drugs, preoperative transfusion, postoperative transfusion, use of nitric oxide, sildenafil, gastroesophageal reflux, GTT (gastrostomy) with or without Nissen fundoplication, arterial umbilical catheter, venous umbilical catheter, PICC (peripherally-inserted central catheter), surgical repair, mesh use, surgical complications, liver hernia, stomach hernia, intestine hernia, reoperation, and the use of mesh in the reoperation.
The data were stored in an Epi Info 7 database (Centers for Disease Control and Prevention, EPI-INFO, version 7, GA, USA) and data analysis was performed using SPSS software (SPSS for Windows, Version 16.0. Chicago, USA).
Considering death as the main outcome, the odds ratio and 95% confidence intervals (95% CI) were calculated for all variables studied. Pearson's chi-squared test was used to verify their association with dichotomous variables (potential predictors), and Student's t-test was used to compare the means of continuous variables.
The project was submitted to the Ethical Committee on Research Involving Human Beings of IFF/Fiocruz on February 6, 2015 and was approved under CAAE No. 45777215.5.0000.5269.
ResultsDuring the study period, 141 children with CDH were diagnosed, and after the inclusion and exclusion criteria were applied, a total of 129 medical records were considered for analysis, after 12 medical records related to newborns referred only for the surgical procedure were excluded. Of these, 121 were admitted at the NICU and eight died in the delivery room.
At the prenatal diagnosis, mean gestational age at diagnosis was 19 weeks. Forty (31%) preterm infants with a GA of less than 37 weeks and 89 full-term newborns (69%) were identified, with a GA of 37–41 weeks, were identified.7
Most newborns 77 (59.7%) were males, the mean birth weight of this population was 2622g (820–3940g), and the most prevalent type of hernia was on the left, with 106 cases, (82.2%), while 33 (25.6%) had other congenital anomalies; according to the intrauterine ultrasound investigation, the most frequent findings were cleft palate and lips, hydrocephalus, myelomeningocele, omphalocele, congenital clubfoot, Cantrell's pentalogy, amniotic band syndrome, esophageal atresia, renal malformations, and cardiac malformations.
Intrauterine surgery started being available from the year 2012 in this study's Institute and is intended only for the most severe cases of diaphragmatic hernia. The fetal endoscopic tracheal occlusion is performed between the 24th and the 28th weeks of gestation, and the tracheal balloon is scheduled to be removed between the 32nd and 34th weeks of pregnancy; however, only four (3.1%) of the newborns were submitted to the endoscopic tracheal occlusion procedure so far, and of these three survived and one died, the latter having an associated genetic syndrome (Fryns syndrome), a condition that goes undiagnosed at the conventional karyotyping of the amniotic fluid.
Regarding the newborns aged 0–6 full days of life, there were 58 (73.4%) cases of early neonatal deaths in this sample, while among newborns aged 7–27 full days of life, there were 17 cases (21.5%) of late neonatal death; the newborns aged 28–364 days, which comprise post-neonatal death, represented four (5.1%) of the cases.8
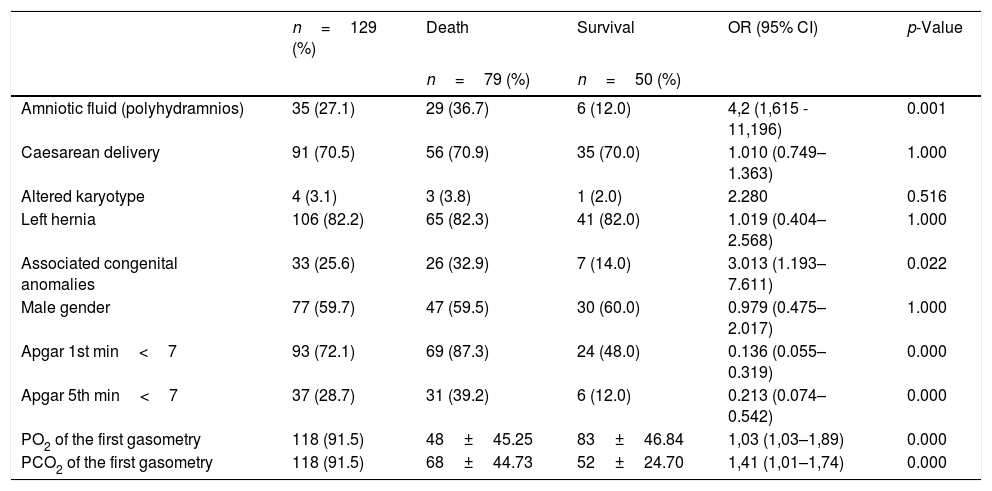
A total of 129 medical files of puerperal women were evaluated in the antenatal period and at the time of delivery (Table 1).
Antenatal and delivery information of the newborns according to the occurrence of death (n=129).
| n=129 (%) | Death | Survival | OR (95% CI) | p-Value | |
|---|---|---|---|---|---|
| n=79 (%) | n=50 (%) | ||||
| Amniotic fluid (polyhydramnios) | 35 (27.1) | 29 (36.7) | 6 (12.0) | 4,2 (1,615 - 11,196) | 0.001 |
| Caesarean delivery | 91 (70.5) | 56 (70.9) | 35 (70.0) | 1.010 (0.749–1.363) | 1.000 |
| Altered karyotype | 4 (3.1) | 3 (3.8) | 1 (2.0) | 2.280 | 0.516 |
| Left hernia | 106 (82.2) | 65 (82.3) | 41 (82.0) | 1.019 (0.404–2.568) | 1.000 |
| Associated congenital anomalies | 33 (25.6) | 26 (32.9) | 7 (14.0) | 3.013 (1.193–7.611) | 0.022 |
| Male gender | 77 (59.7) | 47 (59.5) | 30 (60.0) | 0.979 (0.475–2.017) | 1.000 |
| Apgar 1st min<7 | 93 (72.1) | 69 (87.3) | 24 (48.0) | 0.136 (0.055–0.319) | 0.000 |
| Apgar 5th min<7 | 37 (28.7) | 31 (39.2) | 6 (12.0) | 0.213 (0.074–0.542) | 0.000 |
| PO2 of the first gasometry | 118 (91.5) | 48±45.25 | 83±46.84 | 1,03 (1,03–1,89) | 0.000 |
| PCO2 of the first gasometry | 118 (91.5) | 68±44.73 | 52±24.70 | 1,41 (1,01–1,74) | 0.000 |
Chi-squared test; 95% CI, 95% confidence interval; OR, odds ratio.
Table 1 shows the antenatal and delivery factors of newborns with congenital diaphragmatic hernia according to the occurrence of death. There was a significant association of death with polyhydramnios in the amniotic fluid, associated congenital anomalies, gestational age at the diagnosis of CDH, birth weight, Apgar score at the 1st min<7, Apgar score at the 5th min<7, low PO2 in the first gasometry, and high pCO2 in the first gasometry.
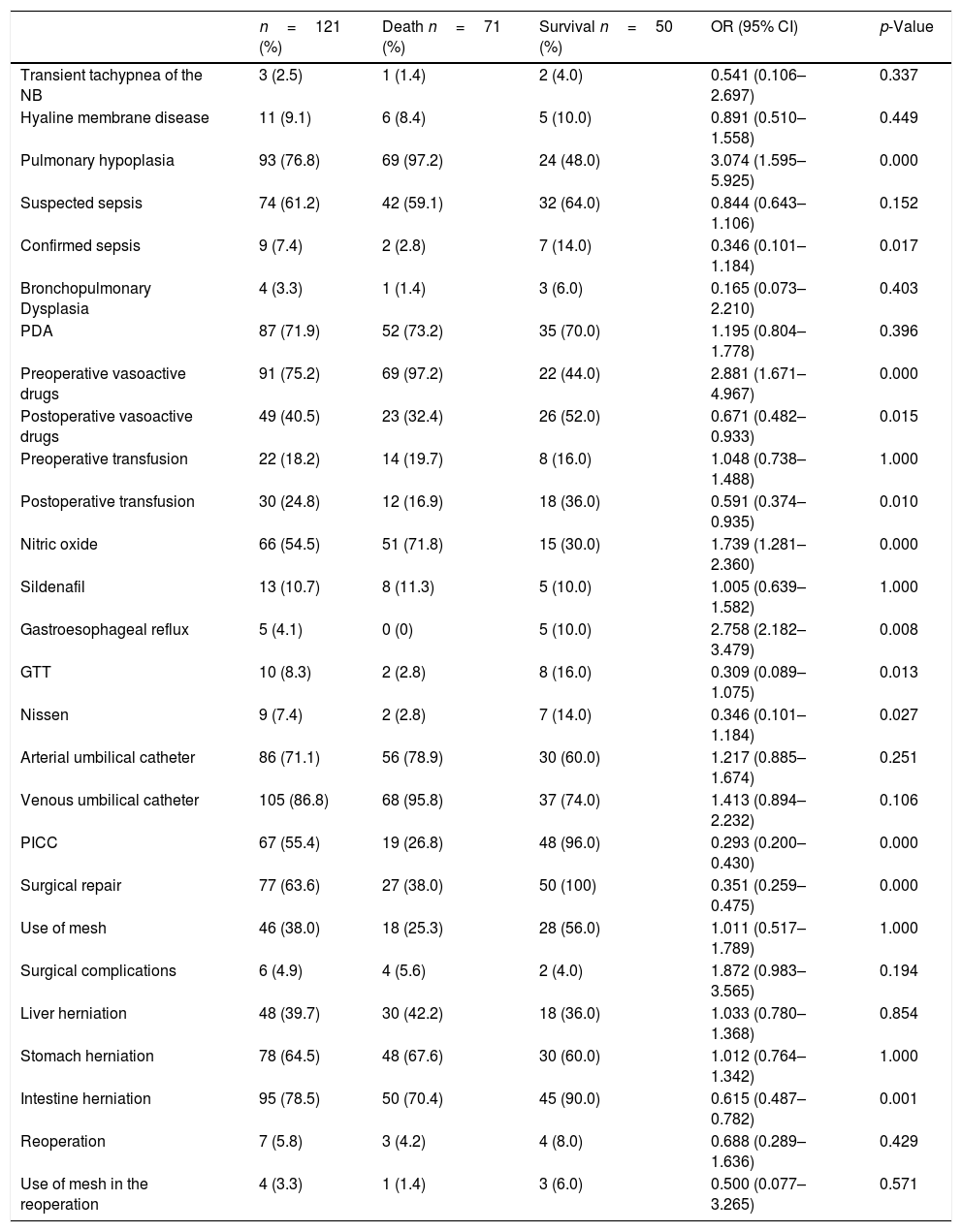
Table 2 shows the data regarding the hospitalization period in the NICU. Significant differences regarding death with pulmonary hypoplasia, preoperative vasoactive drugs, and herniation of the intestine were observed.
Information on the hospitalization period in the neonatal intensive care unit – postnatal factors of newborns with congenital diaphragmatic hernia according to the occurrence of death.
| n=121 (%) | Death n=71 (%) | Survival n=50 (%) | OR (95% CI) | p-Value | |
|---|---|---|---|---|---|
| Transient tachypnea of the NB | 3 (2.5) | 1 (1.4) | 2 (4.0) | 0.541 (0.106–2.697) | 0.337 |
| Hyaline membrane disease | 11 (9.1) | 6 (8.4) | 5 (10.0) | 0.891 (0.510–1.558) | 0.449 |
| Pulmonary hypoplasia | 93 (76.8) | 69 (97.2) | 24 (48.0) | 3.074 (1.595–5.925) | 0.000 |
| Suspected sepsis | 74 (61.2) | 42 (59.1) | 32 (64.0) | 0.844 (0.643–1.106) | 0.152 |
| Confirmed sepsis | 9 (7.4) | 2 (2.8) | 7 (14.0) | 0.346 (0.101–1.184) | 0.017 |
| Bronchopulmonary Dysplasia | 4 (3.3) | 1 (1.4) | 3 (6.0) | 0.165 (0.073–2.210) | 0.403 |
| PDA | 87 (71.9) | 52 (73.2) | 35 (70.0) | 1.195 (0.804–1.778) | 0.396 |
| Preoperative vasoactive drugs | 91 (75.2) | 69 (97.2) | 22 (44.0) | 2.881 (1.671–4.967) | 0.000 |
| Postoperative vasoactive drugs | 49 (40.5) | 23 (32.4) | 26 (52.0) | 0.671 (0.482–0.933) | 0.015 |
| Preoperative transfusion | 22 (18.2) | 14 (19.7) | 8 (16.0) | 1.048 (0.738–1.488) | 1.000 |
| Postoperative transfusion | 30 (24.8) | 12 (16.9) | 18 (36.0) | 0.591 (0.374–0.935) | 0.010 |
| Nitric oxide | 66 (54.5) | 51 (71.8) | 15 (30.0) | 1.739 (1.281–2.360) | 0.000 |
| Sildenafil | 13 (10.7) | 8 (11.3) | 5 (10.0) | 1.005 (0.639–1.582) | 1.000 |
| Gastroesophageal reflux | 5 (4.1) | 0 (0) | 5 (10.0) | 2.758 (2.182–3.479) | 0.008 |
| GTT | 10 (8.3) | 2 (2.8) | 8 (16.0) | 0.309 (0.089–1.075) | 0.013 |
| Nissen | 9 (7.4) | 2 (2.8) | 7 (14.0) | 0.346 (0.101–1.184) | 0.027 |
| Arterial umbilical catheter | 86 (71.1) | 56 (78.9) | 30 (60.0) | 1.217 (0.885–1.674) | 0.251 |
| Venous umbilical catheter | 105 (86.8) | 68 (95.8) | 37 (74.0) | 1.413 (0.894–2.232) | 0.106 |
| PICC | 67 (55.4) | 19 (26.8) | 48 (96.0) | 0.293 (0.200–0.430) | 0.000 |
| Surgical repair | 77 (63.6) | 27 (38.0) | 50 (100) | 0.351 (0.259–0.475) | 0.000 |
| Use of mesh | 46 (38.0) | 18 (25.3) | 28 (56.0) | 1.011 (0.517–1.789) | 1.000 |
| Surgical complications | 6 (4.9) | 4 (5.6) | 2 (4.0) | 1.872 (0.983–3.565) | 0.194 |
| Liver herniation | 48 (39.7) | 30 (42.2) | 18 (36.0) | 1.033 (0.780–1.368) | 0.854 |
| Stomach herniation | 78 (64.5) | 48 (67.6) | 30 (60.0) | 1.012 (0.764–1.342) | 1.000 |
| Intestine herniation | 95 (78.5) | 50 (70.4) | 45 (90.0) | 0.615 (0.487–0.782) | 0.001 |
| Reoperation | 7 (5.8) | 3 (4.2) | 4 (8.0) | 0.688 (0.289–1.636) | 0.429 |
| Use of mesh in the reoperation | 4 (3.3) | 1 (1.4) | 3 (6.0) | 0.500 (0.077–3.265) | 0.571 |
n, number of patients; Student's t-test; 95% CI, 95% confidence interval; OR, odds ratio; NB, newborns; PDA, patent ductus arteriosus; GTT, gastrostomy; PICC, peripherally-inserted central venous catheter.
This study evaluated the prognostic factors associated with death from the intrauterine period to the first year of life, establishing the significant factors associated with death, and allowing us to identify the profile of the most severe cases of congenital diaphragmatic hernia of this institution.
The identification of the worst prognostic factors remains a challenge to be overcome, aiming to provide adequate antenatal and postnatal care to this population, and to reduce mortality, minimize damage in adult life, and reduce hospitalization time, in an attempt to reduce the problems caused by complications and morbidities inherent to the most severe cases.
The mortality rate in this study comprised 79 cases (61.2%), which is similar to the mortality rate found in the national literature. A retrospective analysis of 27 medical files between April 1991 and January 2002 carried out with 27 newborns in Hospital das Clínicas of Faculdade de Medicina of Universidade de São Paulo (HCFMUSP) described a mortality rate of 67% of newborns with congenital diaphragmatic hernia.9
The exclusion criteria aimed to homogenize the sample, since the children referred only for the surgical procedure were excluded from this study due to different conditions in care and recording of the antenatal data, in the delivery room, and in the NICU, resulting in changes in prognostic factors, such as the occurrence of sepsis and bronchodysplasia.
In this sample, survival was similar between the two types of CDH, with the survival rate on the left side being 38.6% and on the right side, 39%. There is no consensus regarding the survival rate, as some authors report higher rates in newborns with right-sided diaphragmatic hernia, while others report that there is no difference in survival rates associated with the type of hernia, as observed in our population.10,11
The type of hernia was identified during the prenatal period through ultrasonographic assessment and was later confirmed by the description of the surgical report for cases in which the postnatal surgery was performed, or by the anatomopathological report in cases that died prior to the surgical procedure.
In the current sample, the mean gestational age at the diagnosis of prenatal CDH was 19 weeks; as in the present study, Colvin et al. also identified that the gestational age for the diagnosis of CDH was 19 weeks. Thus, these data corroborate those of most authors, who identified that the gestational age at the prenatal diagnosis was between 19 and 29 weeks.10,12–14
Recently published articles have described the incidence of diaphragmatic hernia with associated malformations as 35–50%; in the present study, 25.6% of the newborns had malformations, and 3.1% had an altered karyotype, which was the worst prognosis.13,15 Polyhydramnios was identified in 27.1% of the newborns who died, a higher rate than that observed in published articles, which identified a percentage between 14.8% and 20.2% of polyhydramnios cases. It is believed that this high rate is associated with the impossibility of performing an abortion for this type of congenital anomaly.10,12,14–16
In this study, the incidence of CDH was higher on the left side, representing 82% of cases, compared to only 18% of cases on the right side. The frequency found in this study corroborates several other authors, who reported a lower incidence of right-sided diaphragmatic hernia.10,14,17
The ideal moment for delivery remains uncertain, but a systematic review has shown that survival was higher when the gestational age of birth was between 37 and 38 weeks, and other authors have stated that delivery should occur at approximately 39–40 weeks. It is known that the inherent complications of preterm birth accentuate the hemodynamic instability of newborns, but in the present study the gestational age at birth was on average 37 weeks, consisting mostly of full-term newborns.18
The type of delivery did not affect newborn survival in this series, which is in agreement with other studies that also found no difference in survival of infants with diaphragmatic hernia after caesarean or normal delivery.10,12,14,17,19
The hemodynamic instability of the newborn in the delivery room was a determinant for more severe prognoses and evolution to death, evidenced by the Apgar scores in the 1st and 5th minutes<7, which in this study correlated to mortality rates of 87.3% and 39.2%, respectively, corroborating other studies in which the Apgar score was a predictor of mortality in cases of congenital diaphragmatic hernia.12,15,20
The most severe cases of the diaphragmatic defects, in which newborns showed greater pulmonary involvement, were identified by the arterial blood gas collected shortly after birth, with a lower pO2 in the first gasometry and a higher pCO2 in the first gasometry showing statistical significance with mortality.
There is a lot of discussion about the ideal time to perform the postnatal surgery, but most international studies propose that the surgical repair of the diaphragmatic defect be performed after clinical stabilization. The newborns who underwent postoperative surgical repair at the earliest moment, i.e., at less than 10 days of life, showed the best prognosis in this study, also showing a lower rate of surgical complications when compared to those described by Colvin et al.12
The use of mesh to occlude the diaphragmatic orifice was necessary in 38% of newborns with extensive diaphragmatic defect, and although these represent the most severe cases of diaphragmatic hernia, the newborns in whom it was used showed a higher survival rate.
Patent ductus arteriosus (PDA) was confirmed by echocardiography performed before surgery or as early as possible and was identified as a risk factor. The use of vasoactive drugs in the preoperative period and the use of nitric oxide were also identified as risk factors for death this study, determining the cases of diaphragmatic hernia with worse prognosis.18
Despite the prolonged hospital length of stay, there were few cases of sepsis in this study, confirmed through the result of positive blood cultures collected during hospitalization at the intensive care unit.
In international studies on mortality associated with diaphragmatic hernia, approximately 87% of survivors have an associated morbidity, such as pulmonary, gastrointestinal, and neurological diseases, and these complications were also responsible for the longer hospital length of stay.15
In the present study, only 3.9% of the patients had gastroesophageal reflux, when compared with another study of which percentage was 11%.21 Those with gastroesophageal reflux returned to the institution due to repeated hospitalizations from pneumonia, requiring gastrostomy with fundoplication; despite the small number of cases, repeated admissions constituted a risk for the infants.
The consequence of mechanical ventilation use for a long period on the newborn's immature lung results in the onset of a typical pulmonary disease of prematurity, bronchopulmonary dysplasia; however, in this study, children were followed up to 1 year of age and only 3.1% had bronchopulmonary dysplasia, a small number compared to another follow-up study of up to 2 years of infants with diaphragmatic hernia, where the incidence of chronic pulmonary disease was 50%.22
The organs herniated by the diaphragmatic defect were identified by the description of the operative report, the description of the ultrasound, and pathological reports, with hernia of the intestine being the most frequent and representing a protective factor against death in this population.
Liver herniation was identified in 42.2% of cases of diaphragmatic hernia that resulted in death in this study, corroborating other authors that described the presence of intrathoracic liver hernia as a more reliable ultrasound prognostic factor for the occurrence of neonatal death.13,15,22,23
The strong association of pulmonary hypoplasia with mortality was also identified by other authors, who stated that diaphragmatic hernias with minor defects were associated with a lower degree of pulmonary hypoplasia and had a higher survival rate.13,24
Among the limitations of this study, a selection bias may have occurred, since the patients referred only for the surgical procedure in this institution were excluded, who would probably be less severe cases and, consequently, with lower mortality.
The definition of reliable prognostic factors is a constant concern of the centers treating patients with diaphragmatic hernia and no single factor was shown to be ideal for predicting survival. However, it was identified that the presence of only intestines in the hernia content was a protective factor against mortality in our sample.
To conclude, among the prognostic factors associated with the mortality of newborns with congenital diaphragmatic hernia, the ones that represented a worse prognosis, resulting in a higher chance of death were the use of preoperative amines due to the extreme hemodynamic instability of these newborns, and the presence of pulmonary hypoplasia, which represented the most severe cases and the greatest extent of the diaphragmatic hernia.
Conflicts of interestThe authors declare no conflicts of interest.
The authors would like to thank the postgraduate course teachers for sharing their knowledge and teachings that provided reflection and learning, and the employees of the Archives Section of Instituto Fernandes Figueira, for their numerous trips to the archives to verify the database and the medical records, preparing them for later analysis.
Please cite this article as: Carmo RI, Peixoto-Filho FM, Bueno A, Fonseca M, Junior SC. Prognostic factors of death in children during the first year of life due to congenital diaphragmatic hernia: analysis of a hospital cohort from 2005 to 2015. J Pediatr (Rio J). 2020;96:569–75.
Study conducted at Fundação Oswaldo Cruz (FIOCRUZ), Instituto Nacional de Saúde da Mulher, da Criança e do Adolescente Fernandes Figueira (IFF), Rio de Janeiro, RJ, Brazil.