To estimate the prevalence of asthenopia in 0–18 year-old children through a systematic review and meta-analysis of prevalence studies.
SourcesInclusion criteria were population-based studies from 1960 to May of 2014 reporting the prevalence of asthenopia in children. The search was performed independently by two reviewers in the PubMed, EMBASE, and LILACS databases, with no language restriction. This systematic review was performed in accordance with the Cochrane Collaboration guidelines and the PRISMA Statement. Downs and Black score was used for quality assessment.
Summary of findingsOut of 1692 potentially relevant citations retrieved from electronic databases and searches of reference lists, 26 were identified as potentially eligible. Five of these studies met the inclusion criteria, comprising a total of 2465 subjects. Pooled prevalence of asthenopia was 19.7% (12.4–26.4%). The majority of children with asthenopia did not present visual acuity or refraction abnormalities. The largest study evaluated 1448 children aged 6 years and estimated a prevalence of 12.6%. Associated risk factors were not clearly established.
ConclusionAlthough asthenopia is a frequent and relevant clinical problem in childhood, with potential consequences for learning, the scarcity of studies about the prevalence and clinical impact of asthenopia hinders the effective planning of public health measures.
pretendemos estimar a prevalência de astenopia em crianças de 0 a 18 anos de idade por meio de uma análise sistemática e uma meta-análise dos estudos de prevalência.
Fontes dos dadosos critérios de inclusão foram estudos de base populacional de 1960 a maio de 2014 que relataram prevalência de astenopia em crianças. A busca foi realizada de maneira independente por dois analisadores nas bases de dados PubMed, EMBASE e LILACS, sem restrição de idioma. Essa análise sistemática foi realizada de acordo com as diretrizes da Colaboração Cochrane e com a Declaração dos Itens de Relatório Preferidos para Análises Sistemáticas e Meta-Análise (PRISMA). A escala Downs & Black foi usada para avaliação da qualidade.
Síntese dos achadosde um total de 1692 citações possivelmente relevantes recuperadas de bases de dados eletrônicas e buscas de listas de referência, 26 foram identificadas como possivelmente elegíveis. Cinco desses estudos atenderam aos critérios de inclusão, incluindo um total de 2465 indivíduos. A prevalência total de astenopia foi de 19,7% (12,4–26,4%). A maioria das crianças com astenopia não apresentavam anomalias de acuidade visual ou refração. O maior estudo avaliou 1448 crianças de 6 anos de idade, com prevalência estimada de 12,6%. Os fatores de risco associados não foram claramente estabelecidos.
Conclusãoembora a astenopia seja um problema clínico frequente e relevante na infância, com possíveis consequências para o aprendizado, a escassez de estudos sobre a prevalência e o impacto clínico da astenopia prejudica o planejamento efetivo das medidas de saúde pública.
Asthenopia, defined as a subjective sensation of visual fatigue, eye weakness, or eyestrain, is a common condition in adults1–4 and can result from a variety of causes, including uncorrected refractive errors, imbalance of extra ocular muscles, accommodative impairment, and improper lighting.5,6 It can manifest itself through different symptoms, such as watery eyes, itching, double vision, blurred vision, sore eyes, headache, dry eye sensation, and redness.6
Asthenopia is frequently associated with situations where the accommodative and vergence processes are more intense, such as in those who work long periods looking at video display units (VDU). Although children are using electronic devices, such as computers and videogames, with increasing frequency, the prevalence of asthenopia in this age group is unknown.1–5
This is an important gap in the literature, because when it affects children, visual fatigue may be related to problems involving reading, writing and learning disability, attention, and memory, as well as school performance.5 Visual fatigue may also indicate the existence of complex conditions such as dyslexia, which require special handling.5–8
Most studies of children have small samples and are highly heterogeneous regarding evaluation methods, with no standardized tools for diagnosis, population, and exposure conditions.
This study aimed to describe the prevalence of asthenopia and its related factors in childhood through a systematic review and meta-analysis of observational studies.
MethodsThis systematic review was performed in accordance with the Cochrane Collaboration guidelines and the PRISMA Statement.9,10
Eligibility criteriaEligibility criteria were: studies describing asthenopia prevalence in children aged 0–18 years. Asthenopia was defined by the presence of visual fatigue or eye weakness during the performance of near visual tasks, writing, or reading as reported directly by children. Case reports, case series, and case-control studies in which no data on prevalence could be estimated were excluded. Studies of children referred to ophthalmic care due to eye symptoms were also excluded.
If a study contained multiple publications (or sub-studies), only the most recent publication was included, while the other publications were used for supplemental information.
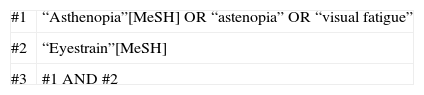
Information sourcesThe review protocol was registered with the institutional research committee. The search comprised online databases – MEDLINE (accessed via PubMed), Cochrane Library, LILACS, Google Scholar, SCIELO, and EMBASE, using MeSH terms for PubMed and Embase, and DeCS for LILACS and SCIELO. The search included references from 1960 to May of 2014 and comprised the following terms: “asthenopia”, “eyestrain”, and “visual fatigue” (Annex 1). Articles in languages other than English were included. To identify primary studies, the authors searched and checked for reference lists of previously published papers and abstracts. Full-text versions of all potentially relevant articles were obtained from electronic databases.
Study selection and data extractionTwo investigators (MAPV and LCP), independently evaluated titles and abstracts of all articles retrieved by the search strategy. All abstracts providing sufficient information regarding inclusion and exclusion criteria were selected for full-text evaluation. In the second phase, the same reviewers independently evaluated these full-text articles and made their selection in accordance with the eligibility criteria. Disagreements between reviewers were solved by consensus, and, if a disagreement persisted, by a third reviewer (VDC). Patient recruitment periods and areas were evaluated in order to avoid possible double counting of patients included in more than one report by the same authors/working groups.
The same two reviewers independently conducted data extraction, including methodological characteristics of the studies, prevalence of asthenopia and related factors using standardized forms. Disagreements were solved by consensus.
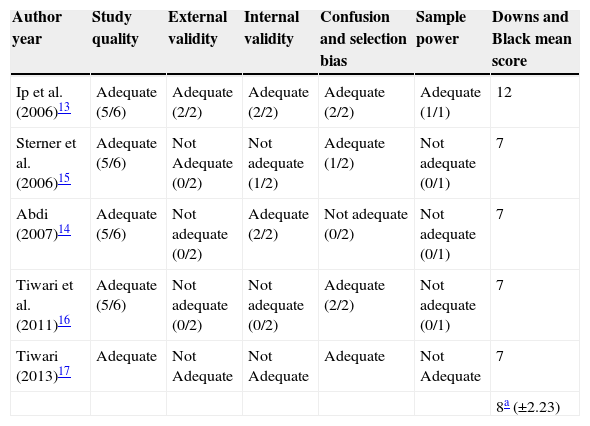
Assessment of risk of biasStudy quality was assessed using Downs and Black's quality score for non-randomized studies11 and comprised of five sections: (1) Study quality (ten items) – to assess the overall quality of the study; (2) external validity (three items) – to determine the ability to generalize the findings of the study; (3) study bias (seven items) – to assess bias in the intervention and outcome measure(s); (4) confounding and selection bias (six items) – to determine bias from sampling or group assignment; (5) power of the study (one item) – to determine whether findings are due to chance.
Two reviewers independently performed quality assessment and classified the studies as adequate, inadequate, or unclear/not reported according to each criterion.
As no intervention study was selected, the maximum score possible in the present review was 12 points. Any scores under 7 points were considered inadequate for inclusion in the meta-analysis.
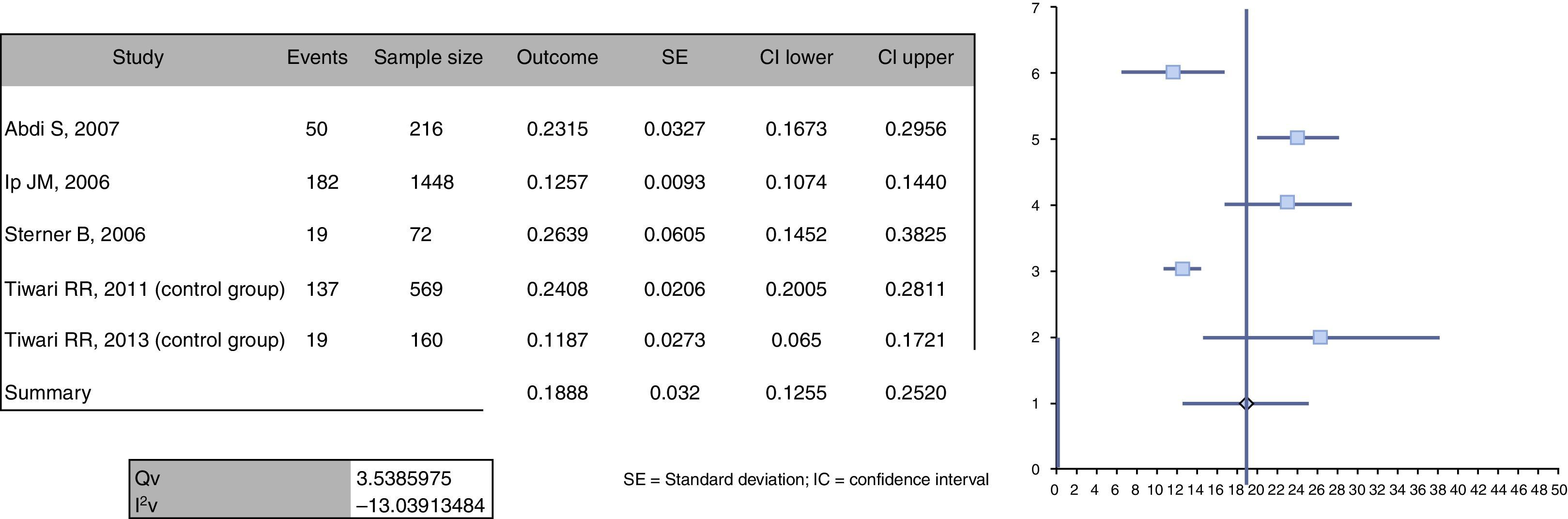
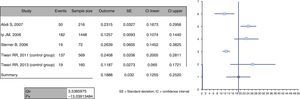
Data analysisThe outcome of meta-analysis is the summary effect or single groups summary. In this case, the outcome was combined prevalence. Prevalences were calculated using data extracted from the original studies, expressed as the number of cases divided by total number of participants evaluated. Standard errors, variance, and weighted effect size were calculated, and forest plots were produced using the method described by Neyeloff et al.12
Using this model, it is possible to obtain the result of the meta-analysis of descriptive data through both fixed and random effects. Furthermore, the model also calculates heterogeneity and inconsistency (Cochran's Q test and I2 inconsistency test) and enables the production of forest plots based on prevalence. Depending on the heterogeneity and inconsistency results, Neyeloff et al.12 propose the use of the random effects model when heterogeneity is high (above 50%) or when it is believed that there are significant differences between populations. Thus, random effects measures were adopted in the present study, considering the differences among the studied populations. Since variability was assumed to be not only due to sampling errors, but also to variability of effects in the population, in this model the weight of each study was adjusted with a constant (v) representing variability.11 When necessary, sensitivity analysis was performed, removing one study at a time and evaluating the possible changes that could lead to a significant difference.
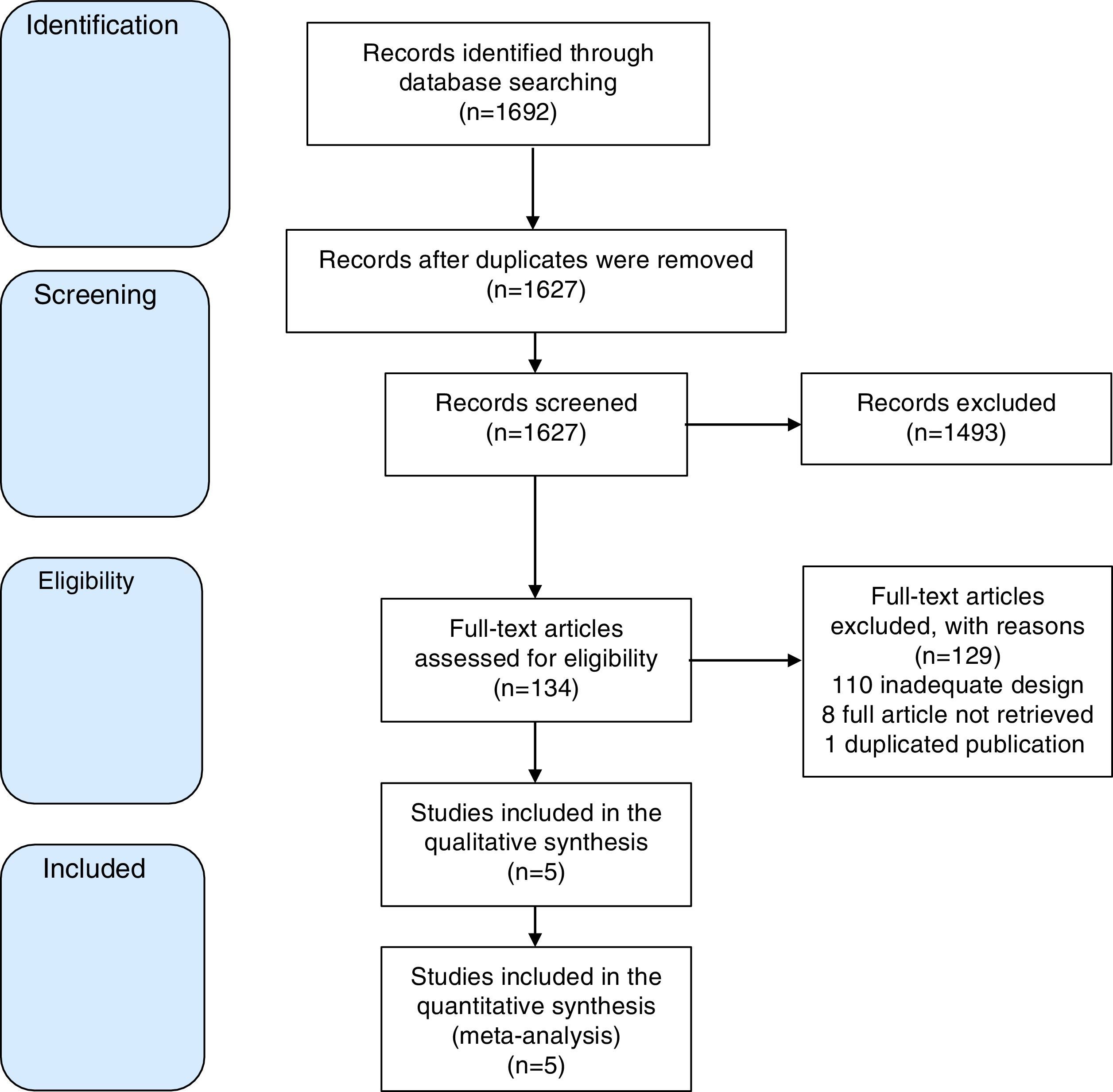
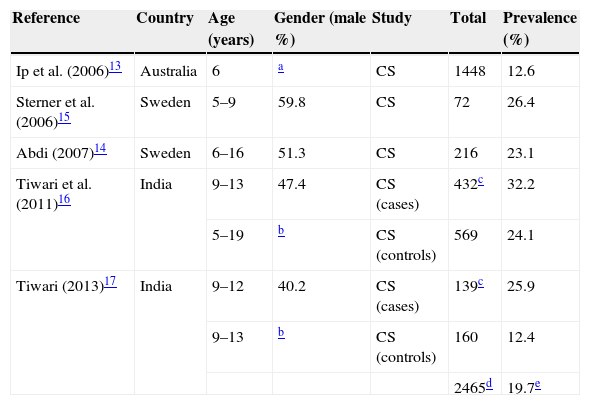
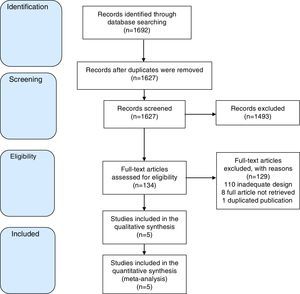
ResultsOut of 1692 potentially relevant citations retrieved from electronic databases and searches of reference lists, 26 were identified as potentially eligible. Five of these met the inclusion criteria, comprising a total of 2465 subjects. Fig. 1 shows the study flow diagram in this review. The maximum Downs and Black score was 12 points and the minimum was 7 points (mean=8.4). Tables 1 and 2 summarize the characteristics of these studies and methodological quality.
Descriptive results of the selected studies of asthenopia in children.
| Reference | Country | Age (years) | Gender (male %) | Study | Total | Prevalence (%) |
|---|---|---|---|---|---|---|
| Ip et al. (2006)13 | Australia | 6 | a | CS | 1448 | 12.6 |
| Sterner et al. (2006)15 | Sweden | 5–9 | 59.8 | CS | 72 | 26.4 |
| Abdi (2007)14 | Sweden | 6–16 | 51.3 | CS | 216 | 23.1 |
| Tiwari et al. (2011)16 | India | 9–13 | 47.4 | CS (cases) | 432c | 32.2 |
| 5–19 | b | CS (controls) | 569 | 24.1 | ||
| Tiwari (2013)17 | India | 9–12 | 40.2 | CS (cases) | 139c | 25.9 |
| 9–13 | b | CS (controls) | 160 | 12.4 | ||
| 2465d | 19.7e |
Methodological evaluation of included studies.
| Author year | Study quality | External validity | Internal validity | Confusion and selection bias | Sample power | Downs and Black mean score |
|---|---|---|---|---|---|---|
| Ip et al. (2006)13 | Adequate (5/6) | Adequate (2/2) | Adequate (2/2) | Adequate (2/2) | Adequate (1/1) | 12 |
| Sterner et al. (2006)15 | Adequate (5/6) | Not Adequate (0/2) | Not adequate (1/2) | Adequate (1/2) | Not adequate (0/1) | 7 |
| Abdi (2007)14 | Adequate (5/6) | Not adequate (0/2) | Adequate (2/2) | Not adequate (0/2) | Not adequate (0/1) | 7 |
| Tiwari et al. (2011)16 | Adequate (5/6) | Not adequate (0/2) | Not adequate (0/2) | Adequate (2/2) | Not adequate (0/1) | 7 |
| Tiwari (2013)17 | Adequate | Not Adequate | Not Adequate | Adequate | Not Adequate | 7 |
| 8a (±2.23) |
Combined asthenopia frequency of was 19.7% (SD 6.7; 12.4–26.4%). Fig. 2 shows the prevalence forest plot. Heterogeneity measured by random effects was very low (I2=−13.03).
The authors used different questionnaires to detect cases, and only Tiwary et al. adopted control groups. The only population-based sample was that described by Ip et al. The other authors used convenience samples.
The largest study, conducted by Ip et al.13 evaluated 1448 children aged 6 years and estimated a prevalence of 12.6%. 82% of children with eye fatigue symptoms had normal ocular examination. Adbi14 evaluated 216 children aged 6 to 16 and detected 23.1% asthenopia prevalence. The symptoms were related to refractive errors (myopia and astigmatism), low visual acuity, and accommodative insufficiency. Sterner et al.15 evaluated 72 children, aged 5–9 years, and estimated an asthenopia prevalence of 26.4%, with relevant influence of accommodative insufficiency.
Tiwari et al.16,17 evaluated children in very unusual conditions who worked as stone polishers or in the shoe-making industry. The control groups used in both studies did not comprise working children and were therefore included in this analysis. Prevalences of 24.1%16 and 12.4%17 were found, respectively.
DiscussionThe combined frequency of asthenopia was 19.7% in this systematic review and meta-analysis of population-based prevalence studies. Gender was not associated with differences in prevalence, but children aged over 7 years showed presented symptoms in all studies.
The relation between asthenopia and visual acuity, binocular dysfunctions or refraction abnormalities was controversial. Ip et al.13 demonstrated that 82% of children aged 6 years have normal ocular examination. In the study conducted by Abdi, a strong association was observed in children aged between 6 and 15 years between symptoms and refractive problems (specially in myopic or astigmatic children), low visual acuity, and accommodative insufficiency.14
Reverse causality could explain why asthenopia was more prevalent in those who wore optical correction. The lower prevalence among children under the age of 7 years may be underestimated due to the difficulties in understanding the questions used for diagnosis by said children. In the study conducted by Sterner et al.15 the sample was selected by invitation. This is a relevant limitation and probably led to selection bias.
In symptomatic children or in children referred to ophthalmic care, some associated causes were described, such as heterophoria (1.4–8.8%), convergence insufficiency (6–11%), accommodative insufficiency (11.1%), amblyopia (3.6%), and strabismus (7.3%). Simple measures could treat most of these causes, which highlights the importance of early detection.7,8,13,15,18 Notwithstanding, these factors occur at the same frequency in children with normal ophthalmic examination.13
It would also be interesting to study children with learning disabilities to evaluate the proportion of these problems that could be attributed to asthenopia. Since most studies showed no important relationship between asthenopia and visual acuity, screening only children with visual impairment would not detect a significant proportion of children with asthenopia.7,8,18 The true frequency of other symptoms of asthenopia and their consequences need to be studied in greater detail.
A limitation of this systematic review is the small number of studies included, even though the searches were conducted using a sensitive strategy and with no language restrictions. The quality of the individual studies was quite heterogeneous regarding sample size, patient selection, methods of assessing asthenopia symptoms, and reporting bias. Nevertheless, the prevalences reported were similar, except for those exposed to unusual laboral conditions. Lower prevalence among children under the age of 7 years may represent an underestimation, possibly because of the difficulties in understanding the questions used for diagnosis in children under this age. Funnel plots are appropriate and should be interpreted as representative for this observational (non-interventional) analysis. They do not reflect the causal effect, but rather different prevalence values. Even though the squares that represent the studies have the same size, the study weight can be estimated by the confidence interval width.
The most important finding of this review is the scarcity of studies enabling the evaluation of asthenopia prevalence in different pediatric populations, as well as the lack of a standardized instrument that is quick to apply and easy to understand.7,8,19–21 It is surprising that most studies are restricted to adults, since asthenopia in children may have important clinical consequences, such as learning disabilities, with potential impact in their future.5,7,8 The absence of detailed knowledge about the true prevalence of asthenopia hinders an effective planning of public health measures for prevention and treatment.
There are lessons to be learned from studies in adults. Asthenopia symptoms in adults increase with time of VDU use.1–6 Children worldwide are heavy users of computers and videogames, sometimes with very long periods of use and at increasingly earlier ages, which makes them especially susceptible. Thus, it is possible that asthenopia prevalence in children will increase in the near future, with additional consequences for learning and school performance. As prevalence is expected to rise with increasing VDU use, more population-based studies are necessary to estimate asthenopia prevalence and related factors in this context, as well as its consequences for learning and development. Nonetheless, until such studies have been conducted, this systematic review may serve as a reference for public and school policies.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Vilela MA, Pellanda LC, Fassa AG, Castagno VD. Prevalence of asthenopia in children: a systematic review with meta-analysis. J Pediatr (Rio J). 2015;91:320–5.