To explore the clinical or sociodemographic predictors for both successful and failed extubation among Chinese extremely and very preterm infants
MethodsA retrospective cohort study was carried out among extremely and very preterm infants born at less than 32 weeks of gestational age (GA).
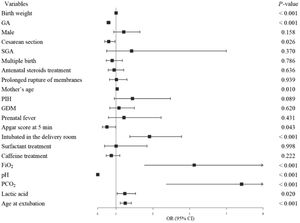
ResultsCompared with the infants who experienced extubation failure, the successful infants had higher birth weight (OR 0.997; CI 0.996–0.998), higher GA (OR 0.582; 95% CI 0.499–0.678), a caesarean section delivery (OR 0.598; 95% CI 0.380–0.939), a higher five-minute Apgar score (OR 0.501; 95% CI 0.257–0.977), and a higher pH prior to extubation (OR 0.008; 95% CI 0.001–0.058). Failed extubation was associated with older mothers (OR 1.055; 95% CI 1.013–1.099), infants intubated in the delivery room (OR 2.820; 95% CI 1.742–4.563), a higher fraction of inspired oxygen (FiO2) prior to extubation (OR 5.246; 95% CI 2.540–10.835), higher partial pressure of carbon dioxide (PCO2) prior to extubation (OR 7.820; 95% CI 3.725–16.420), and higher amounts of lactic acid (OR 1.478;95% CI 1.063–2.056).
ConclusionsHigher GA, higher pre-extubation pH, lower pre-extubation FiO2 and PCO, and lower age at extubation are significant predictors of successful extubation among extremely and very preterm infants.
Preterm birth rates are increasing, with more than one million preterm infants born annually in China.1 The greatest increase is in extremely and very preterm infants.1,2 A longer cumulative duration of mechanical ventilation among very preterm infants is associated with high rates of mortality and morbidities, including ventilator-associated pneumonia, diaphragmatic atrophy, pneumothorax, and bronchopulmonary dysplasia (BPD).3–7 Delayed weaning can also increase the risk of severe intracranial hemorrhage and delayed sepsis.6,8 Weaning from the ventilator as soon as possible and shortening the duration of invasive mechanical ventilation is the current consensus in clinical practice. This goal may be achieved using non-invasive respiratory support and, among intubated infants, by reducing the duration of mechanical ventilation by conducting successful extubation as early as possible. Weaning from a ventilator in preterm neonates is a variable and inconsistent process among centers and clinicians who have limited ability to predict extubation readiness.8
Extubation failure has been independently associated with increased mortality, longer hospitalization, and more days of receiving oxygen and ventilatory support.9–12 It is therefore critical to attempt extubation early and at a time when success is likely. Identifying factors associated with successful extubation may help reduce the duration of mechanical ventilation, improve outcomes, and help to design future research studies in ventilated preterm infants. However, extubation failure will occur in some preterm infants, often secondary to apnea, atelectasis, or intercurrent illness. Very preterm infants are at higher risk of extubation failure than mature infants.
Existing research reports the risk factors for extubation failure among extremely premature infants as: lower gestational age, a lower five-minute Apgar score, lower pH prior to extubation, a higher peak fraction of inspired oxygen, higher partial pressure of carbon dioxide (PCO2), a higher fraction of inspired oxygen prior to extubation, and small for gestational age status (SGA).8,13 However, previous studies have not proposed cut-off values of independent risk factors for extubation failure, and few studies have examined the impact of failed extubation on extremely and very preterm infants in China.
To address these research gaps this study aimed to explore the clinical or sociodemographic predictors for both successful and failed extubation among extremely and very preterm infants, and to identify the cut-off points of significant predictors. The hypotheses of this study are: (1) What are the predicting factors of successful extubation? (2) What are the predicting factors of failed extubation, and the cut-off values of predicting factors for failed extubation?
MethodsStudy designThis was a retrospective cohort study of extremely and very preterm infants intubated within 24 h of birth from 2016 to 2020 at Guangzhou Women and Children's Medical Centre, which has four Neonatal Intensive Care Units (NICUs). The human research ethics committee of Guangzhou Women and Children's Medical Centre approved this retrospective cohort study (SFRKLTZ2020D03300).
Operational definitionsThe criteria for intubation, extubation, and reintubation were as follows. Infants could be intubated if they met any of the following: fraction of inspired oxygen (FiO2) > 0.60 required to maintain oxygen saturation at or above 85% using pulse oximeter; PCO2 > 65 mm Hg, pH < 7.2; or hemodynamic instability.14 Intubation could also be performed at any time for repetitive apnea requiring positive pressure ventilation, clinical shock, sepsis, or the need for surgery. Extubation was to be attempted if the infant met all of the following criteria: PCO2 < 65 mm Hg, pH > 7.20; oxygen saturation ≥ 88% (extubation can be considered when oxygen saturation reaches 88% or higher); FiO2 ≤ 0.50; mean airway pressure < 10 cm H2O; a ventilator rate of ≤ 20 breaths per minute; an amplitude of less than twice the mean airway pressure if high-frequency oscillatory ventilation was being used; hemodynamic stability; and the absence of clinically significant patent ductus arteriosus.8,14 The infants were extubated in a model of non-invasive respiratory support by continuous positive airway pressure (CPAP), or non-invasive positive pressure ventilation (NIPPV). The criteria for reintubation were the same as those for initial intubation.
Sample size calculationAs this is a retrospective cohort study, the authors calculated the sample size post-hoc. The authors calculated the performance of each variable related to extubation failure based on the existing sample size and found that the statistical power was greater than 0.8, indicating the sample size of 385 to be sufficient. The authors used an event per variable (EPV) method to estimate the sample size required for the final multivariate logistic regression – with the EPV equal to 10, the final model was controlled to include eight variables at most. With a missing rate of 10%, the number of patients with extubation failure in the study was at least 88. In this study the extubation failure in the present study's sample was 110, indicating that the sample size of this study is sufficient.
Study participantsInfants were eligible if they had a gestational age (GA) of under 32 weeks, had been receiving mechanical ventilation through an endotracheal tube within 24 h of birth, and were scheduled to undergo extubation for the first time with “non-invasive” respiratory support in one of four NICUs of a regional children's medical centre in southern China. Infants were ineligible if they had a known major congenital anomaly that might affect breathing, or if they were intentionally stopped active treatment at NICU by parents. All subjects with pulmonary hypoplasia were excluded from this study.
Outcome measuresThe primary outcome was successful extubation for longer than three days. Secondary outcomes were BPD, death, BPD/death, retinopathy of prematurity (ROP), severe ROP (defined as needing surgery), necrotizing enterocolitis, severe necrotizing enterocolitis (defined as needing surgery), ligation of patent ductus arteriosus (PDA), intracranial hemorrhage (ICH), days on mechanical ventilation, and increased length of hospital stay among survivors. BPD was defined as the use of supplemental oxygen at 36 weeks postmenstrual age (PMA) or at discharge.15 Infants receiving high/low flow nasal cannula of 21% at 36 weeks were corrected by gestational age and labeled as BPD. Successful extubation was defined as survival without the need for respiratory support with an endotracheal tube for more than three days.16 Extubation failure was defined as the need for reintubation for any reason within 72 h following extubation.17 Hence, this study defined extubation success or failure as occurring up to three days following extubation.18,19 Increasingly, studies define reintubation within three days after extubation as extubation failure20,21 as this captures most clinical information regarding extubation failure and avoids the inclusion of new pathogenic factors in the reasons for extubation failure.
Data collectionDetailed data were collected on baseline characteristics: gestational age, birth weight, sex, mode of delivery, small for gestational age (SGA), Apgar score at five minutes after birth, prolonged premature rupture of membranes (> 18 h), multiple births, maternal age, hypertensive disorders in pregnancy, gestational diabetes mellitus, maternal fever at one week before delivery, antenatal steroids administration, and resuscitation in the delivery room. Peri-extubation characteristics were collected, including surfactant treatment, caffeine treatment, ventilator support (FiO2, pH, PCO2, lactic acid prior to extubation), and age at extubation.
Statistical analysesTo study the incidence and predictors of successful extubation, the authors grouped infants according to whether the first extubation was successful. The authors compared perinatal and peri-extubation characteristics of failed and successful infant extubation. Categorical characteristics were compared between the two groups using a chi-square test and continuous characteristics were analyzed using t-tests. For characteristics that did not follow the normal distribution, the authors used logarithmic transformation to adjust their distribution. Stepwise multivariate regression was used to determine factors associated with successful extubation. To avoid collinearity in the multivariate model, the authors screened the independent variables in advance (using stepwise regression) to determine the independent risk factors of extubation failure (p values of < 0.05 in bivariate tests).
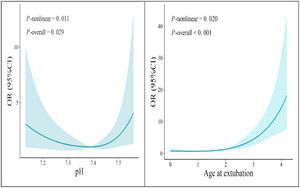
The authors also used the Restricted Cubic Spline regression to analyze the trend of independent risk factors and to explore whether there was a potential nonlinear correlation and critical point between extubation failure and the risk factors. Infants in the successful and failed extubation groups were compared for neonatal morbidities, as outlined above in the secondary outcomes.
ResultsA total of 385 extremely and very preterm infants were intubated in the first 24 h after birth. Among these, 26 infants were excluded (six infants had major congenital malformations, and 20 infants were not given active treatment at NICU by their parents). Thus, 359 infants were included in the retrospective study. Of these 359 infants, there were 249 (69.4%) successful extubation cases and 110 (30.6%) failed cases.
As shown in Table 1, infants in the failed extubation group had lower birth weight, with a mean of 1075.90 g (SD = 283.58); lower gestational age, with a mean of 27.98 weeks (SD = 1.71); and higher pre-extubation FiO2 rates of 40%. Infants in the failed extubation group were more likely to have been intubated in the delivery room; had lower pre-extubation pH, with a mean of 7.32 (SD = 0.18); had higher pre-extubation PCO2 (with 6.30 kPa) and higher amounts of pre-extubation lactic acid (equalling 2.4) (Table 1).
Characteristics of infants in successful and failed extubation groups.
FiO2, fraction of inspired oxygen; GA, gestational age; GDM, gestational diabetes mellitus; IQR, interquartile range; PCO2, partial pressure of carbon dioxide; PIH, pregnancy-induced hypertension; SGA, small for gestational age.
Note: Chi-squared test for categorical variables and student's t-test for continuous variables.
Generalized linear regression analysis in Table 2 shows the following were associated with successful extubation: higher birth weight, higher gestational age (GA), a cesarean section delivery, a higher five-minute Apgar score, and higher pH prior to extubation. Higher FiO2 and higher PCO2 prior to extubation were associated with failed extubation after the stepwise multivariate regression was conducted (Table 2).
The association of multiple risk factors with failed extubation.
| Variables | OR (95% CI) | p value |
|---|---|---|
| GA | 0.555 (0.435-0.709) | < 0.001 |
| pH | 0.016 (0.00-0.296) | 0.005 |
| PCO2 | 13.195 (4.125-42.209) | < 0.001 |
| FiO2 | 4.052 (1.457-11.263) | 0.007 |
| Age at extubation | 1.466 (1.028-2.091) | 0.035 |
FiO2, fraction of inspired oxygen; GA, gestational age; PCO2, partial pressure of carbon dioxide.
Note: PCO2, FiO2 were in-transformed; P value was calculated by stepwise multivariate regression model.
Failed extubation was associated with older mothers, infants intubated in the delivery room, higher FiO2 prior to extubation, higher PCO2 prior to extubation, higher amounts of lactic acid, and greater age at extubation (Figure 1). The cut-off values of the independent risk factors were pH = 7.38, and age at extubation = two days, respectively. If the pH was lower than 7.38, or the age at extubation was greater than two days, the extubation failure rate was higher (Figure 2).
Predictors of successful extubation (OR<1) and failed extubation (OR>1). FiO2, fraction of inspired oxygen; GA, gestational age; GDM, gestational diabetes mellitus; PCO2, partial pressure of carbon dioxide; PIH, pregnancy-induced hypertension; SGA, small for gestational age Note: PCO2, FiO2 were in-transformed; P value was calculated by generalized linear model.
As shown in Appendix (Supplementary Material), the risk of BPD in the failed extubation group was 2.753 times higher than that of the successful extubation group. The risk of death before discharge in the failed extubation group was 14.058 times higher than that of the successful extubation group. The risk of BPD/death in the failed extubation group was 12.304 times higher than that of the successful extubation group. The risk of ROP in the failed extubation group was 1.774 times higher than that of the successful extubation group. The risk of severe ROP in the failed extubation group was 4.037 times higher than that of the successful extubation group. The risk of PDA ligation in the failed extubation group was 4.349 times higher than that of the successful extubation group. The adjustment factors were gestational age, pre-extubation pH, pre-extubation PCO2, pre-extubation FiO2, and age at extubation. Of the survivors, infants in the failed extubation group had longer hospital stays and spent more days on mechanical ventilation compared with those in the successful extubation group (Appendix).
DiscussionIn this retrospective cohort study of extremely and very preterm infants intubated within 24 h after birth, extubation success was predicted by higher gestational age, higher pre-extubation pH, lower FiO2 prior to extubation, and lower pre-extubation PCO2, and lower age at extubation. Infants in the present cohort study who experienced extubation failure were more likely to experience BPD and die before discharge from the hospital, as well as needing prolonged mechanical ventilation and hospitalization.
Preterm infants may fail extubation due to the increased work of breathing, significant apnea and bradycardia, low oxygen saturation, respiratory acidosis, and upper airway narrowing.12 The predictive value for extubation success among infants with higher GAs was expected. Clinicians caring for extremely preterm infants are aware of the increased risk of extubation failure in immature infants compared with more mature infants. In the original randomized trial16 the rate of re-intubation was 32% in extremely preterm infants, compared with 7% for very preterm infants. Most clinicians also consider blood gas measurements, including PCO2, before extubation9 in the knowledge that mechanically ventilated infants with severe hypercapnia are unlikely to be able to generate adequate spontaneous tidal volumes to be successfully extubated.
Higher pre-extubation pH, lower pre-extubation FiO2, and age at extubation independently predicted extubation success in the present study. Consistent with previous research, a higher pre-extubation pH, higher five-minute Apgar scores, and higher GA were associated with extubation success.4,12,17 Further consistent with previous research, age at extubation was a significant predictor of successful extubation.22 This study also found that if the age at extubation was greater than two days, the extubation failure rate increased accordingly.
The authors found in the univariate analysis that cesarean section deliveries, older mothers, and lower lactate pre-extubation were associated with extubation failure, but no association was found in the multivariate analysis. These results might be caused by collinearity; they were not independent risk factors. Additionally, the authors found there was a nonlinear relationship between extubation failure, age at extubation, and carbon dioxide partial pressure. The present data showed that when the pre-extubation pH was lower than 7.38 and the age at extubation was greater than two days, the risk of extubation failure would increase significantly.
At present, research evidence provides limited guidance on extubation indicators. Previous studies evaluating whether newborns should be extubated have focused on clinical symptoms and pulmonary function indicators.23,24 The present study indicates that pH and age at extubation may be used as significant predictors of failed extubation and suggests cut-off values to judge extubation failure.
Extubation failure has an adverse effect on the prognosis of newborns. The authors found those very preterm infants who failed extubation had higher rates of neonatal morbidities, including BPD, death, combined outcomes of BPD/death, ROP/severe ROP, and ligation of PDA. Among survivors, those in the failed extubation group spent longer on mechanical ventilation and had longer hospital stays compared with those in the successful extubation group. The present study's results are consistent with studies by Manley et al.13 and Chawla et al.8 Both these studies were conducted among extremely preterm infants born at less than 28 weeks gestational age and found that failed extubation was associated with BPD, death, longer hospital stays, and ventilation courses. Manley et al.13 also noted that extremely preterm infants who failed extubation were more likely to experience severe retinopathy of prematurity and PDA ligation. Chawla et al.8 noted that extremely preterm infants who failed extubation were more likely to experience severe intracranial hemorrhages (grade III/IV) and late-onset sepsis.
Endotracheal reintubation is not an easy process. Recent studies reported successful intubation rates of between 60% and 73% in preterm neonates, as well as long periods of time (51 ± 28 s) needed for intubation.25,26 Endotracheal intubation is associated with discomfort for the infant and may result in malposition of the tube, trauma to the airway, and hemodynamic instability.25,27 Endotracheal intubations have also been associated with alterations in brain function, as monitored by electroencephalography.28 Reintubation is associated with an increase in nosocomial pneumonia and high mortality, and it is critical to identify effective intervention strategies for avoiding reintubation.29
There are several limitations to this study. It involved a retrospective cohort study of data with selection bias, as the infants included in the analysis, were cared for in one center. Even though the authors adjusted for important and significant clinical variables, there could have been unknown differences in the failed and successful extubation groups that may be associated with both failed extubation and neonatal morbidity. The authors did not analyze the impact of different ventilator modes on extubation failure as the study focused only on initial extubation failure. In clinical practice, infants could have repeated intubation and extubation episodes. A recent systematic review noted that prophylactic methylxanthines reduce the rate of extubation failure in premature infants.30 In the present study's analysis, there was no statistical difference in the use of caffeine before extubation in either the successful or failed extubation groups. Whether or not the association between extubation failure and morbidities such as BPD or death were related to the extubation procedure itself could not be determined from these data. The cut-off values for predicting the failure of extubation obtained in this study are for reference only and need to be further confirmed by a large sample and multi-center study. The failure extubation rate of 30% was higher than in other studies, and this may reflect the treatment status in the present study's center. Finally, as this is a retrospective cohort study, the authors did not collect specific modality parameters for post-extubation respiratory support, and therefore this study could not examine the effect of different modalities on extubation.
ConclusionsThis study found that higher GA, higher pre-extubation pH, lower pre-extubation FiO2 and PCO2, and lower age at extubation are significant predictors of successful extubation among extremely and very preterm infants.
This study is funded by Guangzhou Municipal Health Commission (grant #: 20221A011028).