To evaluate environmental obesogenic-related factors, such as physical activity in neighborhoods and schools, nutritional behavior, and intervention programs.
SourcesCritical analysis of literature with personal point of view from infant obesity experts and political advisors for public intervention.
Data synthesisAlthough obesity is a public health problem affecting several age groups, it is among children and adolescents that it plays a more important role, due to treatment complexity, high likelihood of persistence into adulthood, and association with other non-transmissible diseases while still in early age. Environment is a main component of the genesis and outcomes in the near future or long term. Modification of intake with high-density food, meal skipping, and high intake of saturated fat, sugar, and salt, associated to high levels of sedentarism are main causes of obesity.
ConclusionIntervention opportunities are related to modifications in political, environmental, and individual settings. School and physical activities in the educational environment are intertwined with nutrition intervention in continuous education. A critical review of some different scenarios in Latin American countries is presented.
Avaliar os fatores relacionados ao ambiente obesogênico, como atividade física nos bairros e nas escolas, comportamento nutricional e programas de intervenção.
FontesAnálise crítica da literatura com ponto de vista de especialistas em obesidade infantil e conselheiros políticos de intervenções públicas.
Resumo dos dadosEmbora a obesidade seja um problema de saúde pública que afeta diversas faixas etárias, é entre crianças e adolescentes que ela desempenha um papel mais importante devido à complexidade do tratamento, à alta probabilidade de persistência na vida adulta e à associação com outras doenças não transmissíveis com início precoce. O ambiente é um componente principal da gênese e dos resultados no futuro próximo ou em um prazo mais longo. A modificação do consumo de alimentos de alta densidade, pular refeições e o alto consumo de gordura saturada, açúcar e sal, associados aos altos níveis de sedentarismo, são as principais causas da obesidade.
ConclusãoAs oportunidades de intervenção estão relacionadas a modificações nos cenários político, ambiental e individual. Atividades escolares e físicas no ambiente educacional são intercaladas com intervenção alimentar em uma educação contínua. Uma análise crítica de alguns cenários diferentes é apresentada em países latino-americanos.
Obesity is defined as excessive body adiposity, above the ideal levels for good health. It develops from a chronic, positive energy balance, under the influence of multiple factors of social, behavioral, and environmental origin.1 Although obesity is a public health problem affecting several age groups, it is among children and adolescents that it plays a more important role, due to treatment complexity, high likelihood of persistence into adulthood, and association with other non-transmissible diseases starting at an early age.2,3 Between 1990 and 2010, childhood obesity in the world increased from 4.2% to 6.7%, being higher in developed countries (7.9–11.7%) as compared to developing ones (3.7–6.1%).4 It is estimated that in Latin America, 7.1% of children below the age of 5 years are obese. Obesity prevalence between the ages of 5 and 11 years ranges from 18.9% to 36.9%, whereas among adolescents (12–19 years of age) it varies from 16.6% to 35.8%.5
In Brazil, in the years encompassed between the National Study of Family Expense (Estudo Nacional de Despesa Familiar [ENDEF]) of 1974/75 and the Research of Family Budget (Pesquisa de Orçamentos Familiares [POF])6 of 1996/97, the obesity prevalence observed among children of the country increased from 4.9% to 17.4%.7 Nevertheless, an analysis by age bracket shows that obesity among children below the age of 2 years decreased 2.5%. Currently it affects 6.5% of this age group, having increased among children between the ages of 2 and 5 years from 3.0% to 7.7%.8 Obesity increased six-fold among school children between the ages of 5 and 9 years, affecting 16.8% and 11.8% of boys and girls, respectively. Among adolescents, this condition was estimated at 5.9% among boys and at 4.0% among girls.9
An obesogenic environment includes all aspects that have been shown to be related to possible cause-effects of genering obesity. Based on the concept that obesity is a genetic-metabolic disease modified by environmental factors, the present study focuses on physical and nutritional issues that could modify or be related to infant obesity resolution. A non-systematic review of intervention programs was performed, based on a critical approach and the experience of international organizations for the prevention of infant obesity.
InterventionOne measure alone is not enough to improve the nutritional profile of the population because of the epidemiologic complexity of child obesity. Interventions should encompass:
- -
Incentive measures: disseminate information and motivate individuals to adopt a healthy lifestyle;
- -
Support: facilitate healthy options among already motivated people;
- -
Health protection: prevent exposure of individuals to factors that stimulate non-healthy habits.10
In the political realm, Brazil is one of the signatories of the Plan of Action for Obesity Prevention and Control in Children and Adolescents. Among other actions, the plan requires the implementation of fiscal policies, such as taxes on sugary beverages and highly energetic value products, which are poor in nutrients; regulation of food commercialization and labeling; improvement in school feeding and in physical activity (PA) locations; and the promotion of breastfeeding and healthy eating.11
Before the signature of the Plan, policies aiming at making individuals aware of the importance of healthy life styles, including the adoption of healthy food habits and an active life style, had been already published in Brazil and had impacted child obesity. An example is the National Policy on Food and Nutrition (Política Nacional de Alimentação e Nutrição [PNAN]), the first national policy to propose actions that aim at respecting, protecting, promoting, and providing human rights related to health and food, as well as to emphasize the importance of overweight and obesity as a national public health problem.12
Recently, the Intersectorial Plan of Obesity Prevention and Control in Brazil (Plano Intersetorial de Prevenção e Controle da Obesidade do Brasil) was also published. The actions provided by this plan aim at improving the population's consumption standards, promoting the practice of PA, and organizing the treatment services for this condition.13
The objective of the National Policy of School Food (Política Nacional de Alimentação Escolar [PNAE]), implemented in 1955, is to cater to the nutritional needs of students while they are in the classroom. According to the policy, school food should offer three servings of fruits and vegetables each week, and a maximum of 10% of energy from simple sugar, 15–30% from total fats, 10% from saturated fat, and 1% from trans fat. Purchasing of low nutritional content drinks is forbidden and is restricted for semi-ready preparations, as well as for concentrated food with high levels of sodium or saturated fat. Moreover, in state school facilities the sale of snacks and drinks with products and/or preparations, whether industrialized or not, containing high content of calories, saturated fat, trans fat, free sugars, salt, alcohol content, and low nutritional content is forbidden.10 The Health Department published, for the private schools, a manual for healthy school cafeterias, with essential information regarding what represents a healthy snack and how to promote it.9
As to advertisement and marketing of food, the National Agency of Sanitary Surveillance (Agência Nacional de Vigilância Sanitária [ANVISA]) published RDC #24/2010, which regulates the supply, advertising, information, and other similar practices whose objective is to disseminate and commercially promote foods with high levels of sugar, saturated fat, trans fat, sodium, and low nutritional content beverages. This Resolution represented a major advance, but was suspended, by an injunction of the Federal Justice of Brasília, filed by the Brazilian Association of Food Industries (Associação Brasileira das Indústrias da Alimentação [ABIA]), which questioned ANVISA's competence to regulate the issue.14
Healthy eating initiativesIn the field of support and incentive for healthy eating, some studies were conducted in Brazil focusing on promoting breastfeeding and guidance related to the introduction of supplementary food. Interventions were focused on updating the training of professionals regarding feeding in the first year of life and educational activities with infants’ mothers and grandmothers. The most used theoretical reference in those actions was the “Ten steps for healthy feeding of children under 2 years of age.” By and large, results pointed to improvement in food consumption, such as longer duration of breastfeeding, less early food introduction, delay in introducing processed food to the child's diet, and higher frequency in meat consumption without altering the nutritional status.15–17 The authors praise the positive and protective results for child's health and suggest that other etiological factors should be considered in interventions aiming at obtaining favorable results regarding nutritional status.
Considering the educational actions to incentive and support healthy foods in schools, a review study showed that most of the actions conducted in Brazil were implemented in the last five years, and an increment in knowledge on nutrition and changes in food habits in children were observed.18 However, regarding the nutritional status, and similarly to what was identified in actions geared to infants, the studies did not find any statistically significant changes. This may be explained by the acknowledgment that changes in body mass do not occur in a short period.19
School-based intervention programsIn a nine-month, controlled intervention study conducted among adolescents (10–11 years of age) of Duque de Caxias (RJ), monthly one-hour sessions on nutritional education promoted the consumption of fruit and homemade preparations instead of sugary beverages and other ultra-processed foods. The results showed a reduction in the consumption of industrialized cookies and soft drinks, together with an increase in fruit consumption, with no impact on body mass index (BMI) and on obesity prevalence.19
In Teresina (PI), a randomized, quasi-experimental study with adolescents of 10–14 years of age, from public schools, and with nine weekly meetings, showed a significant reduction in the consumption of soft drinks and processed juices, as well as a lower frequency of consumption of cold cuts and fried food.20
Thus, the success of intervention actions with the pediatric group is evident, related to changes in food consumption and the need for longer studies to evaluate the real effectiveness of the changes in nutritional status. Moreover, there is a need for studies to decrease the prevalence of childhood obesity that evaluate the impact of public policies.
Addressing the school environment is a very important aspect of “Health Promoting Schools” based on the Ottawa Charter for Health Promotion21 applied in many schools around the world, although its effectiveness has not been well established, either because it has seldom been evaluated or has not resulted in positive outcomes. One successful experience is the APPLES Schools project (“Alberta Project Promoting active Living and healthy Eating in Schools”), a three-year intervention in children from ten schools located in disadvantaged areas of Alberta, Canada. A full-time school heath facilitator in each school was responsible for engaging stakeholders, parents, staff, and students to implement different activities conducive to promoting healthy eating and activity. Apart from having a special person in charge of implementing this program, an important aspect is that the activities were tailored to the specific needs of each school. Evaluation including fifth grade students after two years of intervention revealed that children in APPLES schools consumed more fruits and vegetables, consumed less calories, and were less likely to be obese.22
A few examples of policy-based interventions to change the school food environment are briefly described here. “The Healthy Options for Nutrition Environments in Schools” (Healthy ONES)23 is based on a model which focuses on organizational change by using specific implementation cycles designed to build capacity within an organization. This approach was used in some low-income schools in the US. The intervention, which lasted two years, included eliminating the sale of unhealthy foods and the training of school staff in healthy eating. The nutrition environment was used to determine the amount of foods and beverages available at the schools. Observations were made monthly in each targeted school environment. Results were promising; the unhealthy food and beverage items per child per week decreased over time in intervention schools, while in control schools they increased.24,25
The Nutrition Policy Initiative (www.thefoodtrust.org) also was implemented in US schools, but only in those with more than 50% of children eligible for federally subsidized, free, or reduced-price meals. In 2008, Foster et al.26 included the following components: school self-assessment, nutrition education, nutrition policy, social marketing, and parent outreach. A recent evaluation examined the effects on obesity rates among fourth to sixth grade students. Over a two-year period, it showed a 50% reduction in the incidence of overweight, i.e., significantly fewer children in the intervention schools (7.5%) than in the control schools (14.9%) became overweight; however, no differences were observed in the incidence or prevalence of obesity after two years.
Nutrition detectives (www.nutritiondetectives.com),27 which is active in hundreds of schools in the United States and Canada, includes teaching children and their parents how to read food labels and detect deceptive marketing strategies, while learning to identify healthful foods. An initial evaluation of this program showed that third grade students and parents in intervention schools showed a significant increase in nutrition label literacy, while total calories, sodium, and sugar decreased non-significantly, and as found in most interventions, BMI did not change.
Constant28 reviewed the evidence on the effectiveness of school-based nutrition policy on the food environment, student's dietary intake, and BMI. The author found that although several policies have been implemented in both developed as in developing countries, very few have been evaluated. In some countries nutritional standards have already been established for competitive foods, while in other countries these will be implemented soon.
Establishing social healthy habitsBecause preferences and purchasing requests are influenced by cultural and social aspects as well as marketing strategies, which include advertisements on TV, the Internet, and advergames, schools should take advantage of these strategies to promote the appeal of healthier foods and beverages in various ways (Institute of Medicine, 2006-online http://iom.nationalacademies.org/Reports/2005/Food-Marketing-to-Children-and-Youth-Threat-or-Opportunity.aspx). Taste testing in imaginative forms provides students an opportunity to try healthy foods especially fruits and vegetables. Older children can be involved in making changes in order to improve food habits. In the United States, the Action for Healthy Kids, Students Taking Charge program (http://www.studentstakingcharge.org)29 and the Alliance for a Healthier Generation's empowerME@school toolkit (http://www.empowerme2b.org) are resources that provide examples in this area. Social marketing can be especially useful in targeting unhealthy behaviors.30 It is defined as the application of commercial marketing principles (i.e., the four “Ps” of place, price, product, and promotion) to benefit society and the intended audience rather than the marketer (Task Force on Community Preventive Services). Physical activity: increasing physical activity through information approaches, behavioral and social approaches, environmental and policy approaches.31 These “P” principles can change community norms by delivering health messages, as well as encouraging individual behavior change. For example, social marketing can encourage parents to adopt protective behaviors by demonstrating positive parental role models in order to create a healthy home environment, which also influences what children buy at school. Social marketing can be used to promote engagement and positive role modeling, and can also influence health policy by creating and promoting positive social images of healthy behaviors (i.e., show that a healthy option, such as eating fruits and vegetables, is superior to eating junk food).32
Hawkes C. et al.33 recently proposed a novel way of understanding food policy for obesity prevention, identifying four mechanisms, namely: providing an enabling environment for healthy preference, overcoming barriers, encouraging individuals to re-evaluate their unhealthy choices, and stimulating a food systems response. The evidence presented by the authors show that food policies can affect dietary intake from three areas: economic tools (taxes, subsidies), school settings, and nutrition labeling. With respect to schools, the implementation of a range of activities, mostly nutrition education and changes to the environment, have produced more significant and sustained changes. Regarding nutrition education, Kain J. et al.34 showed in a series of interventions in Chile that it had minimal effects, due to problems with adequate implementation, pre-existing unhealthy preferences among children, parents, and teachers, as well as lack of changes to the environment. Yet, other studies have shown that nutrition education-only interventions have been effective in changing intake of certain foods. Although policies that influence the school environment for obesity prevention are very important, the behavior of parents related to food, nutrition, and physical activity are probably more relevant. There is evidence that there are barriers for parents to adopting healthy lifestyles, as demonstrated by some studies based on focus groups. These barriers include the number of siblings, lack of time and money, neighborhood safety, and the child's preferences for sedentary activities.35–37
Sonneville et al.38 conducted a study in which parents of overweight children identified barriers from seven common recommendations for obesity prevention of sweetened drinks and snacks chips in schools was shown ineffective by Cullen et al.39 because in some schools students compensated by purchasing unhealthy “non-banned foods.” However, another study that assessed the impact of a district level nutrition policy in Los Angeles (US), which banned soft-drinks and snacks with limited nutritional value through vending machines and direct sales to all students during school days, showed that 55.5% of students reduced their soft drink consumption and 52.6% reduced snack intake in school.40
Programs targeting the environmentReduction in price of healthier foods, such as low-fat snacks and fruit and vegetables, might increase their sales, as was shown first by French S., in 2003.41 In addition, initiatives to promote fruit and vegetables consumption at schools have been proven successful42; however, it is not realistic to expect that students will continue to adopt healthy diet behavior at school if the school environment does not support these behaviors continually, which requires investigating whether students return to their former behavior when the intervention is no longer in place.
A study published in 2008 that determined the efficacy of behavioral interventions to prevent childhood obesity through a meta-analyses of randomized trials concluded that the effect on target behaviors was small, while that on BMI was non-significant. Longer interventions, greater than six months, yielded marginally better effects than shorter ones.43
Because in general, most childhood obesity prevention interventions have not proved to be sufficiently effective to be sustainable in the long run and obesity in most countries has either increased or remained stable, but has not declined, several highly respected researchers have recently proposed a “systems framework” to address this problem. The system approach focuses on the relationships between different aspects of the environment and interactions between individuals with the environment.44 It is important to distinguish it from a multicomponent model, the interactions among all sectors required to produce sustainable changes that can be scalable. This can be especially important to support modifications to the school environment that can make it easier to adopt healthy choices within the school premises. These issues, which are unique in each school, are critical when designing an intervention and determining its effectiveness.
PA opportunities at schoolThere is a common agreement that during the last decades, there has been a displacement of time from playing, engaging sports, and recreational games towards academic activities. Even some of the after-school programs must compete with technological options. Additionally, physical education (PE) classes do not always influence energy balance with moderate to vigorous physical activity (MVPA). The Center for Disease Control and Prevention of the United States recommends that MVPA should take at least 50% of lesson time. A global review, published by Hollis, including studies from nine countries and published between 2005 and 2014, analyzed the proportion of MVPA during PE lessons.45 The authors concluded that studies based on direct observations report that children spent 57.6% of the PE lesson performing MVPA, compared to studies based on accelerometers in which only 32.6% of the time was spent on MVPA. It is clear that although there are still limitations on PA evaluation methods in children, interventions aimed at increasing MVPA in PE lessons are needed.
School breaks are an excellent opportunity to develop motivational and recreational activities that improve the PA level and fair play. Compared to PE classes, breaks are usually full of non-competitive activities based on fun. A quasi-experimental intervention study conducted in three schools in California tested the time spent on MVFA after teachers’ social prompting of PA during recess. Findings from this study indicate that when a teacher prompted a child to engage in MVPA, it had a significant impact on the amount of MVPA while modeled by a competent adult.46
Unfortunately, when these types of interventions are analyzed regarding obesity prevention, the size effect on BMI is too small or null. Most of the current studies are focused on demonstrating results associated with chronic disease prevention; however, under a more qualitative standpoint of the intervention, it is possible that in the long run, there is impact from sustainable healthy behavior linked to PA.
“TAKE 10!” is another example of a program aimed at addressing the barriers against sedentary behavior at school. It takes advantage of the accumulation of ten minutes of PA during regular classes, integrating movement with academics in elementary schools. Up to August 2010, more than 40,000 schools in the United Sates had participated in TAKE 10! for the previous ten years. The analysis of the programs influence on energy balance suggests incremental expenditure attributed TAKE 10! activities, which range from 24 to 43kcal per 10-minute session. The longer-term studies reported by Kibbe et al. suggest that BMI maintenance is achieved in intervention students when exposure is sustained.47
PA levels naturally decrease with age. It is difficult to distinguish between the physiologic component of growth and the influence of the modern and obesogenic environment through the life course. Girls especially tend to be less active and less involved in PE. Many authors have focused on the role of gender in educational contexts and consider that educators have a critical role and can provide many positive experiences for all students, including girls in PE and sport in order to encourage them to adopt and maintain healthy active lifestyles. Especially for PA interventions, some authors emphasize the importance of age when considering preventive strategies. In preschool children, obesity prevention should focus on promotion of total PA and limitation of screen time rather than dietary behaviors, due to the lack of evidence based on dietary intake. Brown and Summerbell, after analyzing 38 school-based studies, reported that PA interventions may be more successful in younger children and in girls. For girls, dance appears to be an optimal opportunity both to encourage PA and also to maintain or decrease BMI.48
Effectiveness of PA in obesity prevention interventionsGenerally speaking, pediatric obesity prevention programs have been found to cause small changes in target behaviors and small or no significant effect on children's activity level and BMI.43,49 On the other hand, demonstrated by the same methodology (systematic review and meta-analysis) within similar periods of search, another study showed the importance of the PA component in school-based interventions to be effective in reducing BMI in children.50
The bias associated to these differences could be attributed to the measurement of variables of energy expenditure (accelerometer, observational, and/or questionnaires), and/or cut offs of anthropometric measurements, and also, the selection of the studies (randomized or non-randomized). All are probably causes of the differences in assessments and, consequently, in the conclusions.
Two Cochrane reviews on general interventions for preventing obesity in children and specifically on school-based PA programs have demonstrated more positive results.51,52 The first, which assessed educational, behavioral, and health promotion interventions, reported the success of interventions at preventing childhood obesity with no adverse outcomes, by improving both dietary and PA behavior.53,54
Specifically related to PA, in all age groups (0–5, 6–12, and 13–18 years), individual studies that met inclusion criteria demonstrate a significant intervention effect on PA-related factors (three, 21, and five studies, respectively), and some of them in terms of adiposity. The second review published by Dobbins was focused on programs promoting PA and fitness in children. After analyzing 26 studies from 302 eligible ones, there was evidence that school-based PA interventions had a positive impact on four of the nine outcome measures: duration of PA, television viewing, VO2 max, and blood cholesterol.
These results indicate that despite BMI not being an effective primary outcome measure, some other positive health outcomes could be considered as part of the variables that determine prevention of chronic diseases.
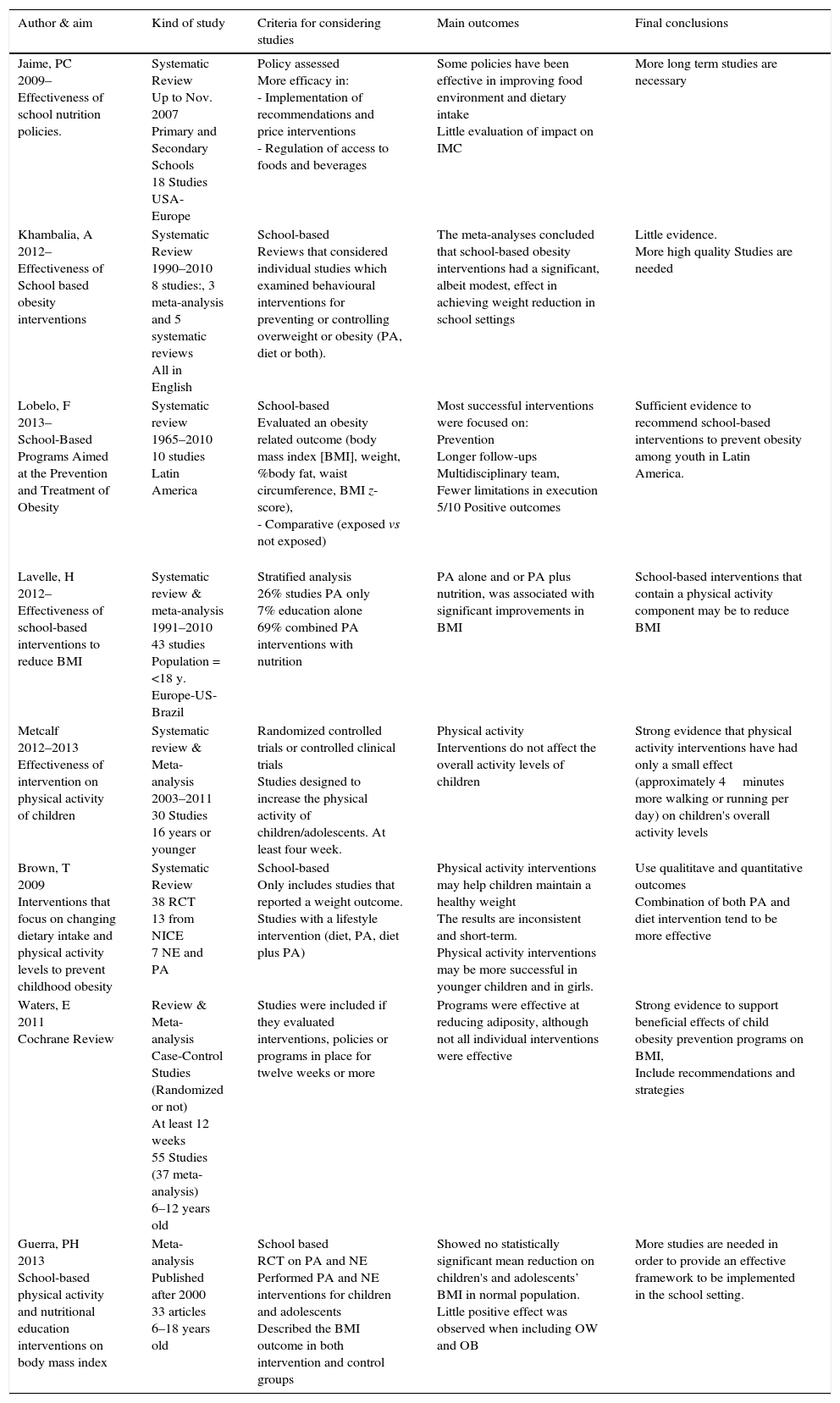
Opportunities for PA in schools, interventions to increase duration and recreational PA, and capacity building for teachers appear to be critical to determine and sustain healthy habits. Since these behaviors are often promoted by environmental cues, current findings suggest value of this type of intervention, especially in proposing change strategies that favor PA (Table 1).
Summary of reviews and/or meta-analysis for physical activity intervention.
| Author & aim | Kind of study | Criteria for considering studies | Main outcomes | Final conclusions |
|---|---|---|---|---|
| Jaime, PC 2009– Effectiveness of school nutrition policies. | Systematic Review Up to Nov. 2007 Primary and Secondary Schools 18 Studies USA-Europe | Policy assessed More efficacy in: - Implementation of recommendations and price interventions - Regulation of access to foods and beverages | Some policies have been effective in improving food environment and dietary intake Little evaluation of impact on IMC | More long term studies are necessary |
| Khambalia, A 2012– Effectiveness of School based obesity interventions | Systematic Review 1990–2010 8 studies:, 3 meta-analysis and 5 systematic reviews All in English | School-based Reviews that considered individual studies which examined behavioural interventions for preventing or controlling overweight or obesity (PA, diet or both). | The meta-analyses concluded that school-based obesity interventions had a significant, albeit modest, effect in achieving weight reduction in school settings | Little evidence. More high quality Studies are needed |
| Lobelo, F 2013– School-Based Programs Aimed at the Prevention and Treatment of Obesity | Systematic review 1965–2010 10 studies Latin America | School-based Evaluated an obesity related outcome (body mass index [BMI], weight, %body fat, waist circumference, BMI z-score), - Comparative (exposed vs not exposed) | Most successful interventions were focused on: Prevention Longer follow-ups Multidisciplinary team, Fewer limitations in execution 5/10 Positive outcomes | Sufficient evidence to recommend school-based interventions to prevent obesity among youth in Latin America. |
| Lavelle, H 2012– Effectiveness of school-based interventions to reduce BMI | Systematic review & meta-analysis 1991–2010 43 studies Population =<18 y. Europe-US-Brazil | Stratified analysis 26% studies PA only 7% education alone 69% combined PA interventions with nutrition | PA alone and or PA plus nutrition, was associated with significant improvements in BMI | School-based interventions that contain a physical activity component may be to reduce BMI |
| Metcalf 2012–2013 Effectiveness of intervention on physical activity of children | Systematic review & Meta-analysis 2003–2011 30 Studies 16 years or younger | Randomized controlled trials or controlled clinical trials Studies designed to increase the physical activity of children/adolescents. At least four week. | Physical activity Interventions do not affect the overall activity levels of children | Strong evidence that physical activity interventions have had only a small effect (approximately 4minutes more walking or running per day) on children's overall activity levels |
| Brown, T 2009 Interventions that focus on changing dietary intake and physical activity levels to prevent childhood obesity | Systematic Review 38 RCT 13 from NICE 7 NE and PA | School-based Only includes studies that reported a weight outcome. Studies with a lifestyle intervention (diet, PA, diet plus PA) | Physical activity interventions may help children maintain a healthy weight The results are inconsistent and short-term. Physical activity interventions may be more successful in younger children and in girls. | Use qualititave and quantitative outcomes Combination of both PA and diet intervention tend to be more effective |
| Waters, E 2011 Cochrane Review | Review & Meta-analysis Case-Control Studies (Randomized or not) At least 12 weeks 55 Studies (37 meta-analysis) 6–12 years old | Studies were included if they evaluated interventions, policies or programs in place for twelve weeks or more | Programs were effective at reducing adiposity, although not all individual interventions were effective | Strong evidence to support beneficial effects of child obesity prevention programs on BMI, Include recommendations and strategies |
| Guerra, PH 2013 School-based physical activity and nutritional education interventions on body mass index | Meta-analysis Published after 2000 33 articles 6–18 years old | School based RCT on PA and NE Performed PA and NE interventions for children and adolescents Described the BMI outcome in both intervention and control groups | Showed no statistically significant mean reduction on children's and adolescents’ BMI in normal population. Little positive effect was observed when including OW and OB | More studies are needed in order to provide an effective framework to be implemented in the school setting. |
RCT, randomized controlled trial; PA, physical activity; BMI, body mass index; OW, overweight; OB, obese; NE, nutritional education.
Despite differences in size effect of positive outcomes from PA interventions, there is no doubt about the general beneficial effect of PA during growth and development. From psychological to biological issues, there are a wide range of health outcomes that have proved to be beneficial for a healthy life. Recommendation of PA during childhood is thus a consensus among scientists and researchers.55
One of the key points includes starting as early as possible to favor a link between early-life experiences and later health outcomes, creating a pattern of PA behaviors through life. Another aspect is that current levels of PA are very poor, and both developed and developing countries do not meet PA recommendations, despite the existent guidelines. As a general rule, recommendations include, type, and duration of PA, and level of intensity.
The environment plays a critical role in infancy, favoring or discouraging engagement in recreational movement activities, PA, and sports. The role of education through messages, or academic contents within the curricula, controversially does not influence behaviors if they are not supported by an increase in opportunities and more access to facilities and activities. Education alone is less effective for prevention than treatment programs, in contrast to encouraging teachers and the entire school staff to become drivers of physical and health literacy and behavior change, and also for being themselves more physically active.56
Summary of recommendations- •
Time: Elementary schools 150/minutes/week. Secondary schools 225–300minutes/week.
- •
Intensity in PE classes: Students are physically active (MVPA) for at least 50% of the PE lesson time.
- •
Quality: Enjoyable classes while teaching and children develop appropriate skills for age and gender.
- •
During school time: Increase opportunities to be active during recess and lunch time. Consider integrating PA into classroom activities.
- •
Schools should provide adequate environments, including equipment and playgrounds, and also organize activities during breaks.
- •
Encourage and offer after school activities, both competitive and non-competitive, in order to include as many students as possible.
- •
Engage teachers and family through events, education, messages, and marketing favoring PA, working positively to create an active school community.
One of the main barriers to achieving the goals of the PA component in preventive programs is the high prevalence of overweight and obesity, which in developing countries is approximately 50% of the elementary school population when considering the sum of both conditions. The challenge for upcoming programs is to consider additional capacity building for PE educators in the field, to teach them how to integrate different “body sizes” within the PE lessons, how to encourage children to be physically active and enjoy it, and how to integrate all children, independent of the physical condition, during the PE class and breaks. The most commonly cited barriers are the limitations in school facilities. In developing countries, financial support for PE classes, breaks, and playgrounds is usually not the priority, and the critical conditions of facilities limit the frequency of PE classes when the weather is inclement. Despite the critical conditions of the schools, sometimes the value is the clue to move forward in some countries, and not the budget. “Salten!” – an Argentinean intervention – was an obesity prevention program developed to increase energy expenditure at schools. Many activities during breaks, including a facilitator, were proposed: a minimum number of materials were donated, playgrounds were painted to encourage playing on the painted ground, and the teacher's training was adequate to increase moderate and vigorous physical activity during school hours.57
Considering that global environmental conditions are leading to energy imbalance, many intervention opportunities appear to be at least part of the solution. It seems very difficult to arbitrary separate the components of energy balance, but in children, the energy expenditure through PA is a crucial component in preventive strategies.
Some authors suggest that school-based interventions are more effective compared to home-based interventions to prevent obesity in children and adolescents. De Bourdeaudhuih et al.58 reviewed 11 European studies and concluded that combining educational and environmental components that focus on both sides of the energy balance create better and more relevant effects, suggesting that environmental interventions might include PA interventions like organized PA during breaks, or before and after school; improved availability of PA opportunities in and around the school environment; and increased PE lesson time; without failing to consider the interventions on healthy food options.
FundingILSI, Coca-Cola, CPW, Danone Institute International and Danone Research, CNPq.
Conflicts of interestMauro Fisberg is an invited speaker for Abbott, Danone, Coca-Cola, Nestle, Unilever, EMS. The other authors declare to have no conflicts of interest.
Please cite this article as: Fisberg M, Maximino P, Kain J, Kovalskys I. Obesogenic environment – intervention opportunities. J Pediatr (Rio J). 2016;92(3 Suppl 1):S30–9.