To analyse the mortality trends in children under five years old in Brazil from 2017 to 2020 and the influence of COVID-19 in 2020.
MethodsA retrospective study employing secondary data from the Brazilian Mortality Information System. Deaths according to cause were extracted and disaggregated into early, late, postneonatal, and 1 to 4-year-old periods. Corrected mortality rates per 1,000 live births and relative risk ratio for the cause of death were calculated.
ResultsThere were 34,070 deaths, being 417 (1.2%) from COVID-19 in 2020. COVID-19 mortality was 0.17 per 1000 live births, reaching 0.006 in the early neonatal period, 0.007 in the late neonatal, 0.09 in the postneonatal, and 0.06 in 1 to 4-year-old. Mortality decreased mostly for some diseases that originated in the perinatal period, congenital anomalies, diseases of the respiratory system and external causes, in this order. In 2020, the highest rate was in the early neonatal period, with a fall from 7.2 to 6.5, followed by the postneonatal (3.9 to 3.4) and late neonatal (2.3 to 2.1). Among children aged 1 to 4-year-old, external causes had the highest proportional rate, and diseases of the respiratory system showed the highest decline.
ConclusionThe mortality rate declined from 2017 to 2020, and this variation was higher in the early neonatal period. The risk of death from COVID-19 was 14 times higher in the postneonatal period and 10 times higher in children aged 1 to 4 year-old compared to the early neonatal period.
Historically, mortality in children has been used as one of the main indicators of health and socioeconomic development1,2 among countries. In Brazil, infant mortality has decreased since the end of the last millennium, thanks to the expansion of basic sanitation and maternal and child health care, although it still presents high values in the poorest regions and in certain pockets of poverty.2
The reduction in infant mortality rates (IMR) is also the result of decades of efforts and governmental initiatives focusing on child health, including the immunization program (1975), breastfeeding incentive program (1981), comprehensive health care program for women and children (1984), program for reducing infant mortality (1995).2 Also, as an integral part of the national primary care policy: the community health agents' program (1991), the family health program (1994), and the pact for the reduction of infant mortality in the legal Amazon and Northeast regions (2008).2 All these initiatives were focused on increasing health prevention and promotion actions and reducing intraregional differences. Data from the Brazilian Institute of Geography and Statistics3 showed a reduction from 29.0 deaths per 1,000 live births in 2000 to 22.2 in 2005, 17.2 in 2010, and 13.8 deaths in 2015.
Currently, with the overall reduction in child mortality rate (CMR), the United Nations4 adopts indicators resulting from preventable deaths. Thus, as part of the set of sustainable development goals to be achieved by the countries by 2030, the aims are to reduce neonatal mortality (0 to 27 days of age) and mortality in children under five years, to a minimum, respectively, of 12 and 25 per 1000 live births.
According to the United Nations Children's Fund,1 the number of deaths of children under five years of age worldwide decreased from more than 12 million in 1990 to approximately seven million in 2010 and 5.2 million in 2019, representing 58% reduction in deaths over the 29-year period. However, in 2019, more than half (53%) of these deaths were concentrated in sub-Saharan Africa and 28% in South Asia. In Brazil, 233,000 deaths of children up to 5 years old were recorded in 1990 and 40,000 in 2019, meaning a drop in CMR from 63 to 14 per 1000 live births, an average annual reduction of 5.2% in this age group.
Despite the advances in improving the living conditions of children aged under five years old in the decline of CMRs observed over the years in many countries, there is a risk of change in the pattern of mortality due to the COVID-19 pandemic. Therefore, it is necessary to monitor deaths by cause and age group and to evaluate the pandemic impact on mortality in general and, in particular, in children under five years old. Understanding this scenario is an important tool for management in pediatric clinics and hospitals. The present study aims to evaluate the annual evolution of mortality in children under five years old from 2017 to 2020 and to estimate the effect of COVID-19 in 2020 on this evolution.
MethodsA retrospective study was performed using public domain data from the Mortality Information System (MIS)5 of the Ministry of Health (MOH) for children under five years old in Brazil from 2017 to 2020.
Deaths were disaggregated into four groups according to the child's age: 0 to 6 days (early neonatal - EA), 7 to 27 days (late neonatal -LN), and 28 to 364 days (postneonatal - PN), and one to four years (1-4y). Underlying causes of death were classified according to the International Statistical Classification of Diseases and Related Health.6
MR was calculated as deaths per 1,000 live births,7 for each group and corrected for underreporting.8 Relative risk (RR) was calculated for each cause and year of study for the LN, PN, and 1-4y, compared to the EN period. Data were analyzed using Excel® and the Statistical Package for the Social Science (SPSS-22)®.
This investigation does not require evaluation by the Ethics Committee in accordance with the resolution of the National Health Council number 5109 because it uses public domain information.
ResultThere were 34,070 deaths among children under five years old in Brazil in 2020, which means a reduction of 19% when compared to 2017 (42,141 deaths), being more marked among children aged 1-4y (-27%) and in the postneonatal period (-21%). On the other hand, the variation in the number of live births, in relation to 2017, was positive in 2018 (0.7%) and negative in 2019 and 2020 (-2.5% and -8.1%, respectively).
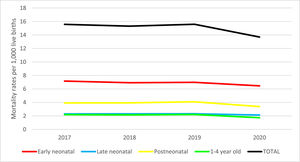
Regarding MRs, the values of the population evaluated maintained a similar trend in the EN periods and from 1-4y of age (Fig. 1). There was a slight decrease from 2017 to 2018, a slight increase from 2018 to 2019, and a sharper decrease in the last year. The LN and postneonatal periods also maintained a similar trend, that is, a slight increase in the first three years and a more marked decline in the last year. As a result, MR in children under five years of age fell from 15.6 to 15.3 per 1000 live births from 2017 to 2018, and there was an increase to 15.6 in 2019 and a significant decrease to 13.7 in 2020. In 2020, the MRs were 6.5, 2.1, 3.4, and 1.7 per 1000 live births, respectively, for the EN, LN, postneonatal, and 1-4y of age periods. In 2020, the EN period concentrated the majority of deaths (16,063, which means 47%), with the highest MR among the age groups (6.5 deaths per 1,000 live births) and showed the largest reduction in MR in relation to the beginning of the studied period (7.2 deaths per 1000 live births).
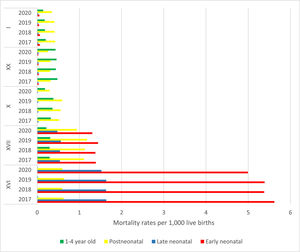
Figure 2 illustrates the five main chapters of causes of death in the period studied. The highest rates were observed in the EN period in all studied years, mainly due to causes related to certain conditions originating in the perinatal period and to congenital malformations, deformations and chromosomal abnormalities, with lower values in 2020. In the LN period, certain conditions originating in the perinatal period prevailed; then congenital malformations, deformities and chromosomal abnormalities; diseases of the respiratory system; certain infectious and parasitic diseases, and, finally, external causes of morbidity and mortality. In the postneonatal period, congenital malformations, deformities, and chromosomal anomalies appear first, followed by certain infectious and parasitic diseases and diseases of the respiratory system. As for children between one and four years of age, external causes of morbidity and mortality lead the death rates; respiratory diseases and congenital malformations, deformities, and chromosomal anomalies alternate according to the year, and certain infectious and parasitic diseases appear last.
Mortality rates of the five main causes of death, per 1000 births, according to chapters of the International Classification of Diseases (ICD-10), per year and period of occurrence, Brazil, 2017 to 2020. I = Certain infectious and parasitic diseases (except COVID-19), XX = External causes of morbidity and mortality, X = Diseases of the respiratory system, XVII = Congenital malformations, deformations and chromosomal abnormalities, and XVI = Certain conditions originating in the perinatal period.
Table 1 shows the RMs of the other causes of death recorded in children under five years old. There is little variation over the years investigated for most of the groups of death causes, with the exception of endocrine, nutritional and metabolic diseases, diseases of the nervous system and diseases of the circulatory system, which showed a decrease in the period. The appearance of COVID-19, highlighted in the group of certain infectious and parasitic diseases, which reached 417 (1.2%) of the 34,070 deaths observed in 2020, is remarkable. MR by COVID-19 was higher in the postneonatal period (0.09), reaching 0.17 per 1000 live births among children under five years old.
Child mortality rates per 1000 live births, due to other underlying causes of death, according to chapters of the International Classification of Diseases (ICD-10), per year and period of occurrence, Brazil, 2017 to 2020.
Table 2 presents RR of deaths comparatively to EN period for each cause.
Relative risk and 95% confidence interval, compared to the early neonatal period (NP), according to chapters of the International Classification of Diseases (ICD-10), by year and period of occurrence, Brazil, 2017 to 2020.
In the postneonatal period, the RR was highest for the following ICD-10 chapters: certain infectious and parasitic diseases (except COVID-19); endocrine, nutritional and metabolic diseases; mental and behavioral disorders; diseases of the respiratory system; diseases of the digestive system; diseases of the skin and subcutaneous tissue; diseases of the genitourinary system; symptoms, signs and abnormal findings of clinical and laboratory findings, not elsewhere classified. This group also presents the highest RR for diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism (except in 2018) and COVID-19. The highest RR for diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism in 2018 occurred for children aged from 1-4y.
The authors highlight the high risk of neoplasms in children aged from 1-4y old, which decreased until 2019 and increased to a higher value in 2020, similar to the postneonatal period that presented the second highest values. For diseases of the respiratory system, the RR falls from 2017 to 2018. However, it increases in 2019, reaching the highest values in all periods of occurrence, falling drastically in 2020, and the ratio in the postneonatal period is almost 82 times higher than in the EN period and 51 times higher between one and four years of age.
With regard to diseases of the digestive system, the ratio is higher in the postneonatal period, with an increase over the years (2017 to 2019) and a decrease in 2020. The same is observed among children aged from 1-4y. As expected, certain conditions originating in the perinatal period and congenital malformations, deformities, and chromosomal abnormalities are lower in all periods compared to the EN period. In addition, according to expectations, the external causes of morbidity and mortality present the highest ratios between one and four years, with a decrease from 2017 to 2018 and increases in the following two years, being the ratio 18 times higher in 2020. The risk of death from COVID-19 was 14 times higher in the postneonatal period and 10 times higher in children aged one to four years compared to the EN period.
DiscussionIn the period studied, the MR in children under five years of age declined from 15.6 to 13.7 deaths per 1000 live births, and the most marked decrease was in the EN period. In addition, there was a reduction of -2.5% in live births in 2019 and -8% in 2020, when compared to 2017. These results reaffirm the trend of reducing infant mortality and other components of mortality in children under five years old, corroborating other national studies.2
Certain conditions originating in the perinatal period led to the causes of death in the neonatal period, situations that could be avoided by adequate attention to the health of women during pregnancy and delivery, as well as to the newborn in the first week of life.10 On the other hand, deaths from congenital malformations, deformities, and chromosomal abnormalities still do not have the avoidable potential.11
Moreover, the other three most frequent causes (certain infectious and parasitic diseases, including COVID-19, diseases of the respiratory system, and external causes of morbidity and mortality), in addition to certain conditions originating in the perinatal period, are potentially preventable by adequate child health care, including monitoring of growth and development, early diagnosis and treatment, adequate feeding, health education, and immunization. It is also important to point out that external causes of morbidity and mortality are observed more frequently among older children, whose exposure to risk factors is higher due to greater independence and physical mobility. Of the total number of deaths (41,115) in children under five years old recorded in 2019 in Brazil, 63.4% were considered fully preventable,12 and high values indicate care failures, which may contribute as inducers of public health policies.13
The contribution of COVID-19 mortality in 2020 was small, representing 1% (417) of deaths in children under five years old. MR in children under five years of age by COVID-19 covered all age groups, being higher in the postneonatal period. The low MR in children under five years old from COVID-19 may be the result of non-pharmacological measures14 implemented during the pandemic and the reduction of fecundity/birth.15 Among children under five years old, MR of some diseases originating in the perinatal period, in addition to COVID-19 was 0.7 deaths per thousand live births. This amount was similar to that in 2017 for the diseases in the perinatal period, showing that despite the slight reduction in 2018 and 2019, MR in this group (preventable causes) remained stable in the evaluated period.
Compared to other countries, MR in children under five years old from COVID-19 estimated in this study (0.168 per 1000 live births) was almost five times higher than that of the United States (0.034),16 also presenting higher proportional mortality from COVID-19 (3.6%) versus 0.3% in the United States in the same age group. Among children under nine years old, the same study16 points out an MR smaller than that found in children under five years old in Brazil (1.68 per 100,000), namely: South Korea (zero), France, and the United Kingdom (0.09), Germany (0.12), Italy (0.16) and Spain (0.18). Despite the low impact of COVID-19 on the mortality of children up to five years old in Brazil, the national situation is more unfavorable than in other countries.
Among the populations affected by COVID-19, children are less affected when compared to adults and generally present milder clinical manifestations of the disease.17 However, this population may progress to death from COVID-19.18 In relation to newborns, there is still no scientific evidence of intrauterine COVID-19 infection, being the infection more probably acquired in a family environment after birth.19 In children affected by COVID-19, studies20,21 report that some develop severe inflammatory syndrome, which in rarer cases may progress to the multisystem inflammatory syndrome temporally associated with COVID-19 (MIS-C). Evidence on the frequency and mortality associated with MIS-C is sporadic, but official Brazilian data suggest an upward trend. In Brazil, the MOH retroactively implemented the MIS-C notification system in July 2020, having registered children under five years old, 269 cases and 21 deaths 2020.22 Although, the MOH has not recorded any cases of MIS-C, nor as an underlying or associated cause of death, it is known that it is a new disease, particularly growing in 2021 and little known in 2020. In 2021, 1,005 new confirmed cases and 59 deaths were reported until September 04,23 and 262 are still under investigation.
Although neonatal and under-five MRs have already reached the 2030 target, there is a certain stagnation from 2017 to 2019 and a decrease in 2020. The appearance of deaths from diseases of the nervous system and the increase in the RRR of deaths from diseases of the eye and adnexa in 2020 is evident in all age groups studied, being higher in all years for children between one and four years old. It is emphasized that, for infrequent diseases, the RRR may increase due to small changes, relatively camouflaging the final estimation. The risk ratios specifically show a reduction in deaths from infectious diarrhea in the chapter on certain infectious and parasitic diseases and malnutrition in the endocrine, nutritional and metabolic disease chapter. They also point to a reduction in pneumonia in the chapter of diseases of the respiratory system, which can be attributed to greater attention of the family (more present due to distance measurements) regarding respiratory symptoms and quick search for medical care, mainly due to fear of COVID-19.
One of the limitations of this study is the use of preliminary mortality data, which is estimated to cover 96% of deaths occurring in the national territory. The use of data from 2017 to 2019 served as a comparison and calibration for the inclusion of COVID-19 in 2020 as a differential cause. Moreover, this research did not focus on the possible underreporting of deaths due to COVID-19, which may have been recorded because of diseases whose symptoms may overlap, such as severe acute respiratory syndrome (SRAG), respiratory insufficiencies, and some septicemia.
In conclusion, in 2020, all-cause mortality in children under five years old decreased significantly, possibly due to lower exposure to health risks caused by non-pharmacological measures and a reduction in the number of live births. Mortality in children under five years old due to COVID-19 was low, but large-scale asymptomatic contamination may contribute to the transmission of the disease in other age groups because the social relationship in this age group is mainly restricted to family and school groups. The impact of COVID-19 on the scenario of social inequalities can be reflected in child and maternal health in the various Brazilian regional loco scenarios. It is recommended that actions aimed at reducing exposure to the virus, the probability of infection, and the severity of COVID-19 are associated with measures and actions of a predominantly economic, social, and health nature.24
Although the impact of COVID-19 on the under-five mortality rate in 2020 was low, the risk of dying from this cause was much higher than in other countries. These deaths suggest weaknesses in the provision of adequate and timely services for the population, especially in disease prevention and health promotion. There is also concern that post-pandemic effects may affect the health of Brazilian children and return to pre-pandemic or even higher levels.
The results of this study reinforce the importance of the pediatric clinic in the surveillance of possible alterations in the epidemiological picture of children due to coronavirus, especially in the specific symptoms of the disease, in addition to the development of other diseases resulting from COVID-19.
These are the challenges that must be predicable, serving as a stimulus for this pandemic situation not to occur again, aiming at improving children's health and achieving the sustainable development goals in 2030.
Public Call from MCTI/CNPq/CT-Saúde/MS/SCTIE/Decit No. 07/2020.