Malnutrition is characterized by situations of undernutrition and obesity resulting from the lack of micronutrients with the greatest impact on children. The objective of this review was to highlight inadequate food consumption, food security, and nutritional inadequacy leading to hidden hunger and the prevention and treatment of the main micronutrient deficiencies in Brazil.
Data sourceLiterature review carried out through a bibliographic survey in PubMed (National Library of Medicine, United States), Lilacs (Latin American and Caribbean Literature in Health Sciences), and SciELO (Scientific Electronic Library Online) databases. The search used the terms Occult hunger, (hidden hunger), and Child, in articles published between 2013 and 2023 in Portuguese, English and Spanish. The search was performed on 06/25/2023.
Data synthesisThe lack of micronutrients can occur insidiously and without clinical manifestations, being called hidden hunger. The prevention of nutritional deficiencies is part of the recommended actions in childcare, with healthy eating. Studies were cited related to macro and micronutrient intake deficiencies, both national and international, and strategies to improve micronutrient intake, including routine supplementation of iron, and vitamins D and A. The diagnosis, prevention, and treatment of the main deficiencies in Brazil (iron, vitamin A, vitamin D, zinc), currently adopted, concluded the topic.
ConclusionZero hunger and zero obesity must be part of the same policy, together with a nutritional education program.
Up-to-date knowledge about children's and adolescents' nutrition is essential for adequate guidance during consultations. Actions must begin with guidelines for maternal nutrition, before and during pregnancy, during the lactation phase, and throughout life, allowing normal growth and development, and optimizing the function of organs, systems and tracts. Great emphasis should be placed on disease prevention in the short and long term.1 Eating habits affect not only weight and height but also neurodevelopment.2,3
In Brazil, the epidemiological and nutritional transition was characterized by a marked decline in stunting in children. However, on the other hand, the epidemic emergence of obesity has been observed, which is often associated with the lack of micronutrients.4 The objective of this review was to highlight inadequate food consumption, food security, and nutritional inadequacy leading to hidden hunger and the prevention and treatment of the main micronutrient deficiencies in Brazil.
Data sourceThis was a literature review carried out with a bibliographic survey in the PubMed (National Library of Medicine, United States), Lilacs (Latin American and Caribbean Literature in Health Sciences), and SciELO (Scientific Electronic Library Online) databases. The search used the terms ‘hidden (occult) hunger’ and ‘child’, in articles published between 2013 and 2023 in Portuguese, English and Spanish. The search was carried out on 06/25/2023.
Data synthesisConceptFood, hunger, and poverty are closely related. In 2004 Josué de Castro defined as “total hunger, the true famishment that English-speaking people call starvation, a phenomenon, in general, limited to areas of extreme poverty and exceptional contingencies, as the much more frequent and more serious phenomenon; and the partial form, the so-called hidden hunger, in which, due to the permanent lack of certain nutritional elements, in a habitual diet, entire population groups allow themselves to slowly die of hunger, despite eating every day”.5
Both “total hunger” and “partial or hidden hunger” are associated with the concept of food security. This concept was widely discussed at the 1st National Conference on Food and Nutritional Security held in Brasília, between the 27th and 30th of July 1994, where the report was approved, which stated that the concept of Food Security should be constructed according to the national reality of each country.6,7
The concept of Food and Nutritional Security (FNS) is under permanent construction. It was used in World War I, reinforced in World War II, and consolidated with the creation of the United Nations (UN) in 1945. At that time, in the newly created international bodies, political tension was already observed between those who understood access to quality food as a human right (Food and Agriculture Organization of the United Nations – FAO) and those who understood that food security would be guaranteed by market mechanisms (Bretton Woods Institutions, such as the International Monetary Fund – IMF – and the World Bank, among others). FNS was defined in a 1986 document, as the “realization of everyone's right to regular and permanent access to quality food, in sufficient quantity, without compromising access to other essential needs, based on health-promoting food practices that respect cultural diversity and that are environmentally, economically and socially sustainable”.8
In 2006, the National Food and Nutritional Security System (SISVAN, Sistema Nacional de Segurança Alimentar e Nutricional) was created in Brazil9, highlighting that the guarantee of this right must consider the availability, access, and biological use of food, and the stability of food availability, access and use over time. It involves everything from the food production and distribution system to the socioeconomic conditions of a population.4 Food Insecurity (FI) consists of the violation of the human right to adequate food.10
Medical-Social importanceAccording to the World Health Organization (WHO), hidden hunger is defined as the non-explicit need for one or more of the 26 micronutrients that are essential for adequate body function.8,11 This condition affects the population in extreme poverty but may be present in obese people.12 Hidden hunger can affect all life cycles, but in children, nutritional deficiencies will have an impact on growth and development, as well as being a predictive variable for chronic non-communicable diseases in adulthood.13
In 2005, according to FAO data, 852 million people suffered from chronic hunger in developing countries. Between 2019 and 2021, hunger affected 7.9 % of the population in South America, 8.4 % in Mesoamerica and 16.4 % in the Caribbean.11 It should be noted that more than 2 billion people worldwide are at risk of developing micronutrient deficiencies. More than 1 billion have micronutrient deficiencies expressed as anemia, vitamin A deficiency or even learning impairment resulting from nutritional deficiencies early in life.14,15 In Brazil, the Family Budget Survey (POF, Pesquisa de Orçamentos Familiares) 2017–2018, through the application of the Brazilian Food Insecurity Scale (EBIA, Escala Brasileira de Insegurança Alimentar), showed that FI in Brazil increased by 62.4 % when compared to data from 2013. The study showed that 36.7 % of the households in Brazil had some degree of FI, whether mild (24.0 %, or 16.5 million), moderate (8.1 %, or 5.6 million), or severe (4 0.6 %, or 3.1 million). This setback places Brazil once again on the “Hunger Map”.16,17
The FI scenario became even more critical in 2020, due to the Covid-19 pandemic, especially for the pediatric population, as evidenced by data from the United Nations Children's Fund - UNICEF.18 The survey carried out in the second half of 2020 shows that 61 % of the families had a reduction in income, which was more evident in the poorest families (69 %). The increase in consumption of processed foods, soft drinks, and fast food during the pandemic was greater in families with children and adolescents and reported by 54 % of those interviewed.18 This scenario resulted in increased rates of obesity in childhood and adolescence and micronutrient deficiency.
Most prevalent nutritional deficienciesAccording to data from the WHO 202319, the most common micronutrient deficiencies globally are vitamin A, vitamin D, vitamin B12, iron, iodine, and zinc, with a higher incidence for iron, iodine, vitamin A, and zinc.14,20,21 The prevalence rates are: 30 % of the world population has insufficient iodine consumption; ⅓ of children under five years of age with vitamin A deficiency in low- and middle-income countries; 17 % of children do not consume the necessary amount of zinc; 18 % of children under five years of age have iron deficiency anemia.
Although there is an overlap in such deficiencies at both the population and individual levels, and the full extent of multiple deficiencies remains poorly documented, hidden hunger remains a global challenge.20 Micronutrient deficiencies, often silent and others with classic manifestations, are identified as crucial in the pathophysiology of complications associated with chronic non-communicable diseases. The effects of the deficiencies, even mild and moderate ones, include poor physical growth and impaired cognitive and psychomotor development, anemia, night blindness, osteoporosis, cardiovascular diseases, increased morbidity from infectious diseases in children, and even cancer. They can also lead to far-reaching implications and affect the development potential of individuals through the reduction of educational gains and work productivity and, ultimately, prevent the development of societies and nations.21,22
Some national studies have shown the inadequacy of healthy food intake by children and adolescents. Bueno et al. (2013) analyzed 3058 children aged 2 to 6 years and observed that the prevalence of inadequate food intake was low for most nutrients. However, approximately 30 % of the sample consumed more saturated fat than the recommended amounts. The prevalence of inadequate vitamin E intake ranged from 15 % to 29 % and more than 90 % of the children had inadequate vitamin D intake. In children over four years of age, the prevalence of inadequate calcium intake was approximately 45 %. Sodium intake was greater than the upper intake level in 90 % of children under four years of age and 73 % of children over four years of age.23 Carvalho et al. (2015) observed, in a systematic review of food consumption in children up to ten years of age, that the prevalence of micronutrient inadequacy ranged from 0.4 % to 65 % for iron, 20 % to 59.5 % for vitamin A, 20 % to 99.4 % for zinc, 12.6 % to 48.9 % for calcium and 9.6 % to 96.6 % for vitamin C.24 Mello et al. (2016) showed that the diet of infants and preschoolers (six months to six years) was characterized by low consumption of meat, fruits, vegetables and green vegetables, high consumption of cow's milk and inadequate preparation of formula, in addition to early and high consumption of fried foods, sweets, soft drinks and salt.25 Data from SISVAN (2022), highlights that more than half of children aged five to nine years had the habit of eating meals while watching television (61.0 %), consumed sweetened drinks (67.0 %), and sandwich cookies, sweets or candy (60.0 %), which may contribute to the increase in the prevalence of hidden hunger.26
The deficiencies associated with the introduction of inadequate complementary foods are often multiple, mainly inadequate zinc, iron and vitamin B6, vitamin B12, riboflavin and niacin content. The National Study of Child Food and Nutrition (ENANI, Estudo nacional de alimentação e nutrição infantil) found a deficiency of vitamin A in 6 %, vitamin B12 in 14.2 %, vitamin D in 4.3 %, and zinc in 17.8 % of children aged 6 to 59 months.27
Iron deficiency, the main nutritional deficiency in the first years of life, was analyzed by the ENANI study (2019), which found a prevalence of anemia among children aged 6 to 59 months in Brazil at 10.1 %, with children aged 6 to 23 months showing a prevalence of 19.0 %.27 Ferreira, H et al. (2020), found a 40 % prevalence in children aged 6 to 60 months28 and Nogueira-de-Almeida et al. (2021) found a 33 % prevalence of anemia in healthy children under 7 years.29
The estimated global prevalence of deficiency in at least one of the three micronutrients (iron, zinc, vitamin A) was 56 % among preschool children.30 Oliveira et al. (2016), in a cross-sectional analysis carried out with 150 children aged 11 to 14 months treated in basic health units in Rio Branco, Acre, found anemia, iron deficiency, vitamin A and B12 deficiency in 23 %, 76 %, 18 %, and 20 % respectively.31 In adolescents, Veiga et al. found inadequacies for calcium (> 95 %), phosphorus (between 54 % and 69 %), and vitamins A (between 66 % and 85 %), E (100 %) and C (between 27 % and 49 %). More than 70 % of the adolescents had sodium intake higher than the maximum tolerable intake.32
Prevention and treatment of major nutritional deficienciesThe main prevention of hidden hunger is adequate nutrition, followed by universal prevention and efficient and timely treatment.
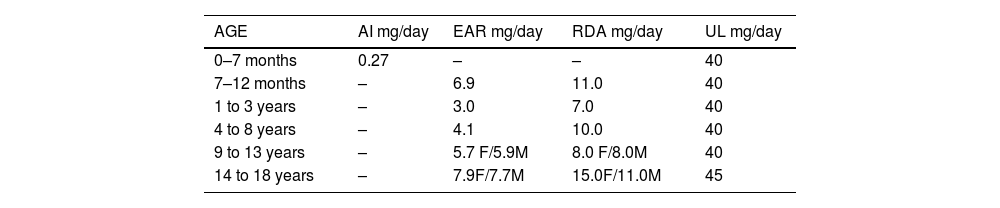
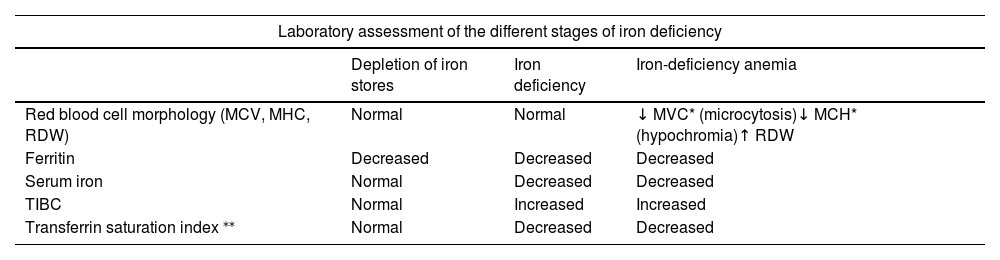
Iron is essential for the body in the formation of hemoglobin, in the transport of oxygen throughout the body, in cell oxidation, and participates in enzymatic reactions (production of new cells, amino acids, hormonal agents and neurotransmitters), for motor and cognitive development, as well as acting on the immune system.33 Children and pregnant women are especially vulnerable to the consequences of iron deficiency. The recommended requirement for iron by age is shown in Table 1.34 The diagnosis of deficiency must be attained early and the intervention must be immediate to avoid sequelae, as shown in Appendix 1. The WHO (2020) evaluates the iron status in populations with hemoglobin (Hb) and serum ferritin and/or transferrin receptors.35 The American Academy of Pediatrics (2011)36 and the Brazilian Society of Pediatrics (2021)37 recommend the laboratory investigation of iron deficiency, with or without anemia, at 12 months of age. However, in cases of suspicion based on the presence of risk factors, the investigation must be carried out promptly and performed early, especially in the absence of adequate iron prophylaxis. The recommended tests for diagnosis are: 1. Whole blood count: to evaluate (Hb), hematimetric indices (MCV, MCH, RDW), and the morphology of red blood cells; 2. Serum ferritin: as a marker of the store depletion phase; 3. C-reactive protein: to identify an infectious process. Treatment is carried out with oral iron. A dose of 3 to 6 mg of elemental iron/kg/day), divided or in a single dose, is recommended for six months or until replenishment of body stores is confirmed by the normalization of serum ferritin and Hb, MCV, and MCH.37
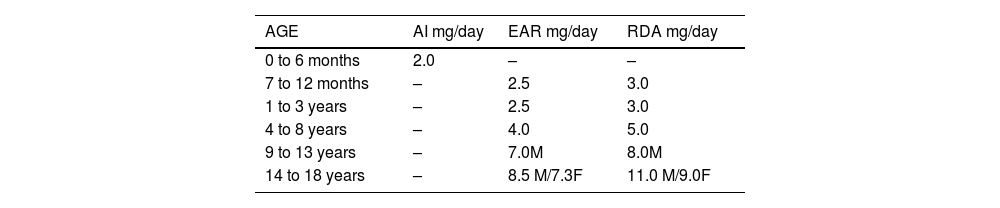
Reference values for daily iron requirements by age group.
EAR, Estimated Average Requirement; AI, Adequate Intake; RDA, Recommended Dietary Allowance; UL, Tolerable Upper Intake Level; M, male; F, female.
Source: IOM, 2001.34
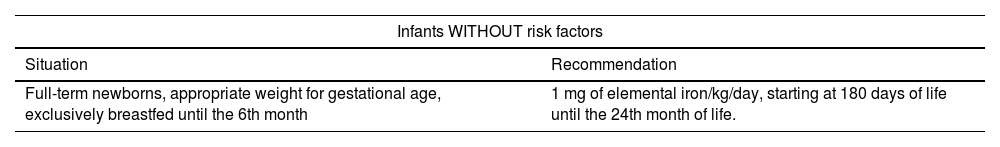
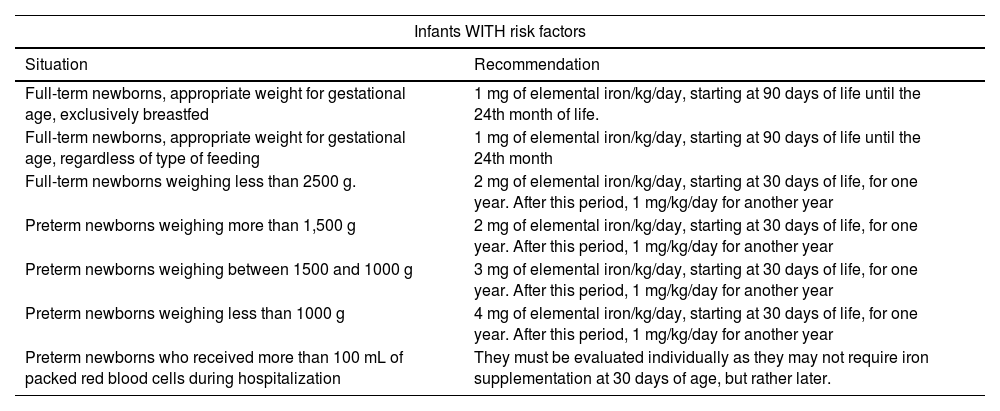
The SBP guideline for the prevention of iron deficiency anemia, according to the presence or absence of risk factors for anemia, is shown in Appendix 2 and Appendix 3.37
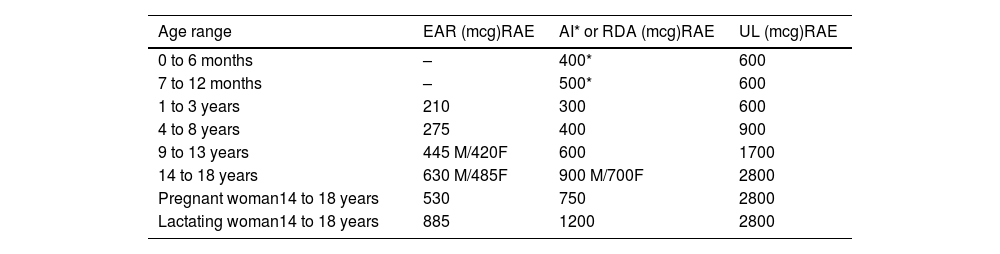
Vitamin A is important for normal vision, gene expression, reproduction, embryonic development, growth, and immune function. It is necessary for the integrity of epithelial cells throughout the body. Children with vitamin A deficiency are at greater risk of blindness and death from infections, especially respiratory infections and diarrhea. Vitamin A deficiency impairs iron mobilization from stores and, therefore, vitamin A supplementation improves hemoglobin concentrations. Zinc deficiency influences the mobilization of vitamin A from the liver and its transport to the circulation.38 The recommended daily average amounts of preformed vitamin A and provitamin A carotenoids are listed in Table 2 in micrograms (mcg) of retinol activity equivalents (RAE).
Reference values for daily vitamin A requirements by age group.
EAR, Estimated Average Requirement; AI, Adequate Intake; RDA, Recommended Dietary Allowance; UL, Tolerable Upper Intake Level; M, male; F, female.
Source: IOM,2001.34
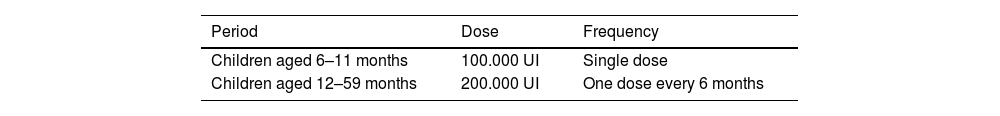
The prevention of vitamin A deficiency is shown in Table 3, according to a publication by the Ministry of Health (2013).38
Prevention of vitamin A deficiency.
| Period | Dose | Frequency |
|---|---|---|
| Children aged 6–11 months | 100.000 UI | Single dose |
| Children aged 12–59 months | 200.000 UI | One dose every 6 months |
Source: Brazil. Ministry of Health (MH), 2013.38
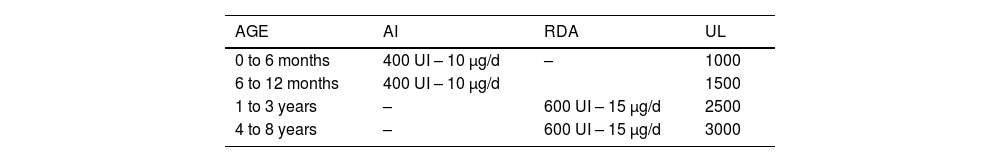
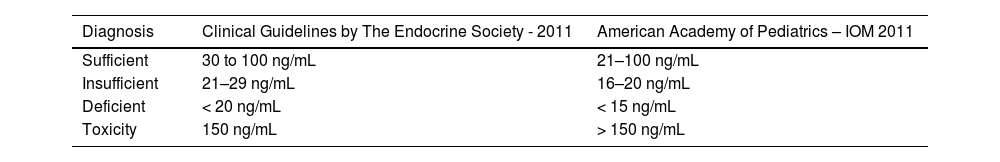
Vitamin D deficiency is one of the most common nutritional disorders worldwide. In Brazil, although the majority of the population lives in regions with adequate sun exposure, hypovitaminosis D is a common problem in children and adolescents.39 Although defined as a vitamin, this substance is conceptually a prohormone (secosteroid) that plays a fundamental role in calcium homeostasis and bone metabolism. It is involved in the regulation of more than 1000 genes, with a role in physiological and immunological processes and endothelial membrane stability.40 Its deficiency may be associated with type 1 diabetes mellitus, asthma, atopic dermatitis, food allergies, inflammatory bowel disease, rheumatoid arthritis, cardiovascular disease, schizophrenia, depression, and several neoplasms.39,40 For the groups at risk for deficiency, prevention is recommended with 400 IU/day (< 1 year), from the first week of life and 600 IU/day (> 1 year) until two years of age, which should be maintained if the individual belongs to a risk group, according to Table 4. Appendix 4 depicts the levels for diagnosis.39
Vitamin D deficiency decreases the intestinal absorption of calcium and phosphorus, leading to an increase in parathyroid hormone (PTH; secondary hyperparathyroidism) that mobilizes calcium from the bone to restore normal serum calcium, causing a reduction in bone mineralization. Therefore, it is important that calcium is also at the recommended levels for the age.39 Dietary reference values are established to meet the needs for growth, development, health function and maintenance, with the daily calcium recommendation for 0 to 6 months is 200 mg/day; 6 to 12 months, 250 mg/day; 1 to 3 years, 700 mg/day; 4 to 8 years, 1000 mg/day and 9 to 18 years, 1300 mg/day.41
Zinc works as a component of several enzymes in maintaining the structural integrity of proteins and regulating gene expression. Daily iron intake at levels like those found in some supplements can decrease zinc absorption. The primary effect seems to be a decreased absorption of zinc at an iron: zinc ratio of 3:1 when iron was administered in water. However, when iron was administered during a meal, this effect was not observed. Reduced copper status was associated with increased zinc intake.34 The recommended zinc intake by age is shown in Table 5
Reference values for daily zinc requirements by age group.
| AGE | AI mg/day | EAR mg/day | RDA mg/day |
|---|---|---|---|
| 0 to 6 months | 2.0 | – | – |
| 7 to 12 months | – | 2.5 | 3.0 |
| 1 to 3 years | – | 2.5 | 3.0 |
| 4 to 8 years | – | 4.0 | 5.0 |
| 9 to 13 years | – | 7.0M | 8.0M |
| 14 to 18 years | – | 8.5 M/7.3F | 11.0 M/9.0F |
EAR, Estimated Average Requirement; AI, Adequate Intake; RDA, Recommended Dietary Allowance; M, male; F, female.
Source: IOM,2001.34
Diagnosis of iron deficiency and iron-deficiency anemia.
| Laboratory assessment of the different stages of iron deficiency | |||
|---|---|---|---|
| Depletion of iron stores | Iron deficiency | Iron-deficiency anemia | |
| Red blood cell morphology (MCV, MHC, RDW) | Normal | Normal | ↓ MVC* (microcytosis)↓ MCH* (hypochromia)↑ RDW |
| Ferritin | Decreased | Decreased | Decreased |
| Serum iron | Normal | Decreased | Decreased |
| TIBC | Normal | Increased | Increased |
| Transferrin saturation index ⁎⁎ | Normal | Decreased | Decreased |
MCH, mean corpuscular hemoglobin; RDW, red cell distribution width (measurement of anisocytosis); TIBC, total iron binding capacity; MCV, mean corpuscular volume.
Recommendation for prophylactic iron supplementation in infants WITHOUT risk factors for iron deficiency.
Fonte: SBP, 2021.37
Recommendation for prophylactic iron supplementation in infants WITH risk factors for iron deficiency.
Source: SBP, 2021.36
Serum levels of 250H-vitamin D for diagnosis.
Health policies must guarantee the right of all children to a healthy start in life, beginning with preconception and pregnancy, guiding maternal lifestyle (nutrition, physical activity, stress, smoking, alcohol consumption, etc.). The first 1000 days of life, from conception to the second year, are crucial for the future health and the formation of human capital42, with immediate initiation of breastfeeding after birth, exclusive breastfeeding for six months of life, and supplemented breastfeeding up to 2 years or more. Extending care to 2200 days, up to 5 years of life, with adequate nutritional guidelines, determines short and long-term health.43,44
The importance of micronutrient deficiencies or "hidden hunger" was clearly emphasized by the inclusion of specific targets on iron, vitamin A, and iodine deficiencies at the 1990 World Summit for Children and other major international nutrition conferences. Since then, significant progress has been made in eliminating vitamin A and iodine deficiencies, with a lower impact on iron deficiency anemia, so far. The role of international agencies such as the WHO, UNICEF, FAO, and the World Bank in helping countries progress towards the goals of the World Summit for Children has been very important.44
According to UNICEF (2019), one in three children under the age of five does not receive the nutrition they need to grow well, as shown in the 2019 edition of The State of the World's Children study. The communities increasingly face a triple burden of malnutrition: despite the decline in undernutrition, 149 million children under the age of 5 still suffer from stunting and almost 50 million are underweight; 340 million children suffer from hidden hunger – vitamin and mineral deficiencies – one in two children has hidden hunger, and rates of overweight and obesity are rising rapidly.44 Deficiencies of several micronutrients generally share a common etiology, such as low consumption of foods of animal origin, fruits, and vegetables, or losses due to frequent infections.22,45
Strategies to resolve hidden hunger include a high-quality diet with a variety of fruits and vegetables, lean meats, low-fat dairy products, whole grains, and an adequate proportion of fatty acids (omega 6 and 3 fatty acids). Consider minimizing the consumption of foods rich in added sugars, saturated fat, alcohol, and sodium, while providing supplementation and/or commercial fortification.46 Biofortification increases the concentration of target nutrients in staple food crops, mainly through genetic manipulation, to attenuate prevalent nutritional deficiencies (iron, zinc, vitamin A).47 For prevention, appropriate maternal and infant feeding strategies need to be practiced. Iron, vitamin A, vitamin D, and zinc supplementation programs need to be expanded. Vitamin B12 deficiency screening and supplementation should only be carried out in high-risk groups.47
Final considerationsIn Brazil, the two extremes of malnutrition – undernutrition due to the lack and obesity due to the excess – share the same scenario. Fighting hunger requires action. On the other hand, families tend to include high-calorie foods in their diet, which are generally less expensive. The issue could be seen from the angle of lack of nutritional information, which requires a focus on promoting education and not on food distribution. Zero hunger and zero obesity must be part of the same policy that includes a nutritional education program so that families can have better knowledge and more access to nutritional quality foods.48 Gabriel Mistral (Nobel Prize winner, 1945): “Many things we need can wait. The child cannot wait. Now is the time when their bones are being formed, their blood is being made, and their mind is being developed. To them, we cannot say tomorrow, their name is today”.48