To evaluate the functional status of individuals with Osteogenesis Imperfecta (OI) followed up at a reference center in the state of Bahia.
Materials and methodsThis is an observational, cross-sectional, descriptive study, which evaluated individuals with OI, based on a non-probabilistic sampling. To assess motor function, the Motor Function Measure (MFM) score was used, in addition to the measurement of muscle strength using the Medical Research Council (MRC) score. Functional performance was measured using the Pediatric Assessment of Disability Inventory, Computerized Adaptive Testing (PEDI-CAT).
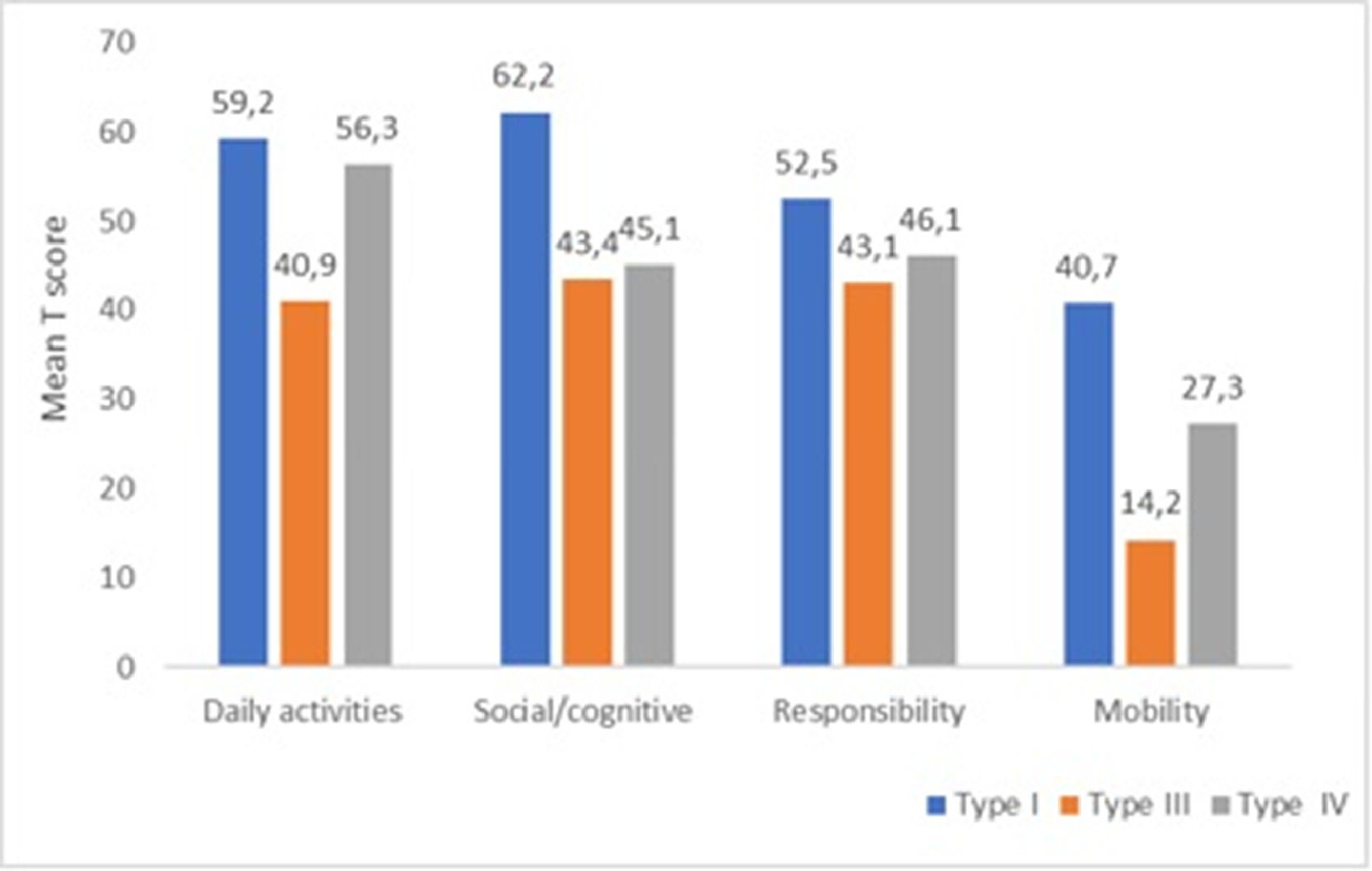
ResultsThirty-one individuals aged between two and 18 years old were evaluated. The overall score of MFM was 74.2%, and the lowest score was found in participants with type III OI (56.3%). The median of the MRC index was 80. The mobility domain was the most affected in the PEDI-CAT evaluation, with a mean T score of 23.9, (14.2 in type III OI).
ConclusionsAmong the evaluated individuals, functional alterations were identified, reduced global gross motor functionality and muscle strength, impacting the mobility domain, with the most relevant findings in individuals with type III OI.
OI is a genetic disease that affects connective tissue. Its main characteristic is the susceptibility to bone fractures with consequent deformities and wide variability of clinical presentation. Other clinical findings include short stature, ligamentous laxity, blue sclera, dentinogenesis imperfecta, and hearing loss.1,2 Prevalence is estimated to be 1:20,000 live births.3
About 90% of OI cases are due to mutations in COL1A1 e COL1A2 and inherited in autosomal dominant pattern and cause defects in the biosynthesis of type I collagen, responsible for the related clinical presentation. Considering the advances in molecular genetic research, other genes and several variants involved in collagen processing or osteoblast function have been identified, with dominant, recessive, or X-linked inheritance, characterizing a disease with great genetic heterogeneity.2,4
According to Sillence's classification (1979), based on clinical and radiographic characteristics, OI is subdivided into 4 types (I, II, III, IV).5 The severity of OI can range from almost asymptomatic individuals with a mild predisposition to fractures, to individuals with severe skeletal deformities, mobility difficulties, and very short stature.4 Type I OI is non-deforming and is considered the mildest form. On the other hand, type II OI is the most severe and frequently lethal in the neonatal period. Type III comprises individuals with a higher degree of functional limitation due to severe bone fragility and marked bone deformity, in addition to extreme short stature. OI type IV is considered to have variable severity.2,4
Functionality is a broad term that encompasses the functions and structures of the body, as well as activity (execution of a task) and participation (involvement of an individual in a real-life situation, representing a social perspective of functionality). The capacity is realized by the participation that the individual presents for the execution of the activities and activities.6
The severity of the clinical manifestation of OI has a great influence on the development of motor skills and is associated with disorders of muscle strength, joint laxity, and functional capability.7,8 Depending on the severity of the metabolic disorder, there may be limitations not only to the structure and the function of the body but also to functional performance, there may be limitations in activities of daily living, sports, leisure, and social activities.9
Some studies have evaluated the functional characteristics of individuals with OI. However, few studies in the literature present the evaluation of body function linked to the impact on other domains such as activity and social participation, which will translate the impact of the clinical manifestations and complications of the disease on different areas of the life of individuals with OI.10 Thus, this study aimed to evaluate the functionality of individuals with OI followed up at a reference center.
Materials and methodsStudy setting and designThis is an observational, cross-sectional, descriptive study, evaluating individuals diagnosed with OI in clinical follow-up at the Professor Edgar Santos University Hospital, of the Universidade Federal da Bahia, which constitutes an OI Reference Center (OIRC).
ParticipantsThe sampling was non-probabilistic, including individuals with OI during their periodic hospital stay to receive parenteral bisphosphonates at the Pediatrics Unit. All participants undergo clinical follow-up in this OIRC. Were included individuals were aged between two and 21 years who agreed (patient and/or parent/guardian) to participate in the research. Those who did not understand the instructions of the evaluation instruments, making data collection unfeasible were excluded. Data were collected from October, 2019 through February 2021 by two examiners with experience in the area, duly trained in the use of evaluation instruments.
Measuring instrumentsThis survey was developed specifically for this study. For the collection of clinical and sociodemographic variables, participants were interviewed using a semi-structured survey and medical records were analyzed. Medical chart data was available completely for all participants. The clinical and sociodemographic variables evaluated were: age, gender, residence, family income, education level of the participant, education level of the guardian, age of OI diagnosis, duration of clinical follow-up at OIRC, weight, height, body mass index, OI classification, need of walking gadgets, history of orthopedic surgeries, physiotherapeutic follow-up.
To evaluate weight, height, and body mass index, were used the curves child growth standards, of the World Health Organization, shown in the Z score.11 The types of OI were identified based on the clinical characteristics, having been diagnosed by a specialist physician, and this information was found in the medical record. Physiotherapeutic follow-up was reported by parents/guardians and was not performed at the OIRC.
For the assessment of gross motor function, Motor Function Measure (MFM) scale was used, which assesses the subject in three dimensions, standing and transfers, axial and proximal motor function, and distal motor function. This scale has been translated and validated for individuals with neuromuscular diseases, and its use may be extended to individuals with muscle weakness from other causes. In children between 2 and 6 years old, was used the reduced version with 20 items (MFM-20). For participants over 7 years old, the full version (MFM-32) was used. Each item evaluated is graded on a scale of 0 to 3 points. The score of each dimension corresponds to the sum of the points obtained by the subject in the items of that dimension, divided by the maximum score of this dimension, multiplied by 100.12,13
Muscle strength was assessed in the subgroup of participants over 6 years old who could cooperate. Medical Research Council (MRC) scales were used, ranging from zero (absence of contraction) to five (normal muscle strength). Three movements of upper limbs (shoulder abduction, elbow flexion, and wrist extension) and three of lower limbs (hip flexion, knee extension, and dorsiflexion) were evaluated bilaterally. After the evaluation, the MRC index was calculated, consisting of the sum of the test scales, divided by the number of muscles tested multiplied by 5. Then, this result was multiplied by 100.14
Functional performance was measured using the Pediatric Assessment of Disability Inventory, Computerized Adaptive Testing (PEDI-CAT), Version 1.3.6, which has already undergone translation into Portuguese and cultural adaptation to Brazil. The PEDI-CAT measures function in four domains: activities of daily living; mobility; social/cognitive and responsibility. The results are expressed in a T score, with the normality value up to two standard deviations from the mean.15
Data analysesData analysis was performed using the Statistical Package for Social Sciences (SPSS) software, version 25. To analyze the normality of the distribution of variables, the authors used the Kolmogorov-Smirnov test. Measures of central tendency and dispersion were presented as mean and standard deviation and/or median and interquartile range. Categorical variables were presented in absolute and relative frequency.
Ethical aspectsThe project was approved by Ethics Committee (protocol number 3.020.967). All participants and/or parent/guardian written consent and assent to participate in the study.
ResultsThirty-one individuals with OI, between two and 18 years old, were evaluated. The median age was 10 years, predominantly females (54.8%). Twenty-nine individuals lived in rural areas of the state, 87.1% of the sample lived on minimum wage or less. Table 1 shows the sociodemographic characterization of the studied sample.
Sociodemographic characteristics of 31 individuals with osteogenesis imperfecta, in a reference hospital in Bahia, Brazil, October/2019 to February/2021.
| Variables | Values |
|---|---|
| Age (years)a | 10 (3-12) |
| Gender n (%) | |
| Male | 14 (45.2) |
| Female | 17 (54.8) |
| Residency n (%) | |
| Rural areas | 29 (93.5) |
| Capital | 2 (6.5) |
| Family income n (%) | |
| Up to 1 minimum wage* | 27 (87.1) |
| 1 to 3 minimum wages* | 4 (12.9) |
| Education level of the participant n (%) | |
| Did not start school life | 6 (19.4) |
| Kindergarten/Preschool | 7 (22.6) |
| Incomplete elementary school | 17 (54.8) |
| Complete high school | 1 (3.2) |
| Education level of the guardian n (%) | |
| Illiterate | 1 (3.2) |
| Incomplete elementary school | 5 (16.1) |
| Complete elementary school | 3 (9.7) |
| Incomplete high school | 5 (16.1) |
| Complete high school | 17 (54.8) |
Clinical data: mean weight (Z score) was -2.9 and height (Z score) -4.1. Most of the evaluated individuals (48.4%) were classified as OI type IV, and twelve individuals had undergone some orthopedic surgical intervention. Only four of the individuals were in physical therapy. Table 2 shows the clinical characteristics.
Clinical characteristics of 31 individuals with osteogenesis imperfecta, in a reference hospital in Bahia, Brazil, October/2019 to February/2021.
| Variables | Values |
|---|---|
| Age of OI diagnosis (years)* | 0.8 (0.08-4) |
| Duration of Treatment at OIRC (years) * | 3.5 (1.8-5.2) |
| Weight (Z score)a | -2.9 (3.0) |
| Height (Z score)a | -4.1 (3.5) |
| BMI (Z score)a | 0.5 (1.8) |
| OI classification n (%) | |
| I | 4 (12.9) |
| III | 12 (38.7) |
| IV | 15 (48.4) |
| Need of walking gadgets n (%) | |
| Totally dependent | 6 (19.4) |
| Wheelchair bound | 14 (45.2) |
| Need of Walker or crutches | 1 (3.2) |
| Walking independently | 10 (32.3) |
| History of orthopedic surgeries n (%) | |
| Yes | 12 (38.7) |
| No | 19 (61.3) |
| Perform physiotherapeutic follow-up n (%) | |
| Yes | 4 (12.9) |
| No | 27 (87.1) |
OI, osteogenesis imperfecta; OIRC, Osteogenesis Imperfecta Reference Center; BMI, body mass index.
Twenty-nine individuals were evaluated with MFM, 13 (44.8%) used MFM-20 and 16 (55.2%) used MFM-32. The mean total MFM score was 74.2%. The lowest scores were obtained in individuals with type III OI, a mean of 56.3%.
Fourteen individuals were evaluated using the MRC index and the median score was 80%, as shown in Table 3.
Measurement of gross motor function and muscle strength in individuals with osteogenesis imperfecta, in a reference hospital in Bahia, Brazil, October/2019 to February/2021.
| Variables | Total | Type I | Type III | Type IV |
|---|---|---|---|---|
| MFM total score (%)a | 74.2 (21.4) | 93.0 (14.0) | 56.3 (20.0) | 81.1 (15.2) |
| MFM by dimensions (%)* | ||||
| Standing and transfers | 30.8 (12.6-91.2) | 100 (48.1-100) | 12.6 (5.1-20.8) | 43.6 (25-94.9) |
| Axial and proximal motor function | 100 (98.6-100) | 100 (100-100) | 100 (48.6-100) | 100 (97,2-100) |
| Distal motor function | 100 (100-100) | 100 (100-100) | 100 (72.6-100) | 100 (100-100) |
| MRC Index (%) n=14* | 80 (71.2-92) | 80 (80-90) | 60 (40.0-86.6) | 81.6 (75-91.6) |
MFM, Motor Function Measure; MRC, Medical Research Council.
Twenty-nine participants were evaluated with PEDI-CAT inventory. The mobility domain was the most affected, mean T score of 23.9 (< -2SD). Mean T scores for responsibility, social/cognitive, and daily activities domains were 45.7, 46.7, and 50.5 respectively, and are considered in the normal range. Figure 1 shows the performances evaluated by the PEDI-CAT inventory, by subtype of OI.
DiscussionThis study aimed to evaluate the functionality of individuals with OI followed up at a referral center. The findings expressed low values for gross motor function and muscle strength, with an important reduction for individuals with OI type III. In addition, the functional performance assessed by PEDI-CAT was below normal in the mobility domain for OI types III and IV.
The evaluation that includes all components of functionality is extremely important for the preparation of an adequate treatment plan since in OI, the impairment of muscle strength and gross motor function, which characterize the structure and function of the body, in justify changes in the execution of their activities and mobility, which can significantly restrict the social participation of these individuals.9
There was a predominance of participants from distant areas in the State and from low-income families treated at the present study's Reference Center. These factors can directly impact the access to complementary therapies aimed at improving the functionality of these individuals. It is important to emphasize that the center where the present study took place is the only one in the state to monitor individuals with OI in the public health system and it explains the concentration of patients from distant areas and mostly from less favored social classes.
It is noteworthy that only a small number of individuals in this sample were on physical therapy despite the fact most individuals were dependent on mobility or needed a wheelchair. In the sample evaluated by Coelho et al.,16 only 24% of the assessed children and adolescents reported performing some kind of physical activity.
Severe short stature was frequently found in the evaluated sample and composes a clinical characteristic of the disease that usually affects patients with OI type III or IV.17 Coelho et al.16, evaluated 50 Brazilian children and adolescents with OI, and found short stature in their sample, with a mean height (Z score) of -3.53 (± 2.59).
Assessment of gross motor function showed individuals with OI type III had worse results in the global score and the standing dimension and MFM transfers. The MRC scores were lower in the type III group when compared with individuals with type I and IV. Due to their greater skeletal involvement, individuals with OI type III experience recurrent fractures and periods of immobilization, with consequent muscle weakness and deconditioning, which leads to more expressive functional limitations.18
The findings here obtained to corroborate the results of a study by Brizola et al.19 When evaluating 62 children and adolescents with OI, they found that muscle strength assessed by manual muscle examination showed a difference when compared to type III to types I and IV for both upper and lower limb muscle strength. In a study by Coelho et al.,16 muscle strength was assessed using the handgrip and was found that the group with OI type III had significantly lower strength than OI types I and IV, and to the age-specific reference data.
Multidimensional assessment with PEDI-CAT showed the studied sample performed below expectations in the mobility domain, with the worst results in OI type III. These findings also corroborate those of Coelho et al.,16 who also assessed the mobility of individuals with OI, through the mobility domain of the PEDI inventory, where type III participants had the worst result with a significant difference when compared to types I and IV. The assessment of mobility is of particular interest to the population with OI, as it is associated with various aspects of participation and quality of life. Individuals with OI type III, for having great musculoskeletal limitation, demonstrate lower mobility scores, ambulation levels, and low levels of participation in sports and professional activities when they reach adulthood.20
In a longitudinal study, Montpetit et al., found that individuals with OI type IV who received a long-term multidisciplinary treatment approach evolved to excellent function in self-care and transfer skills, which is critical to living independently. In contrast, none of the individuals with OI type III achieved independent ambulation, and upper limb problems limited their readiness to live independently. These observations suggest that further improvements in the functional status of the most severely affected individuals with OI depend on advances in the clinical management of upper limb problems.21
This study has some limitations because the size of the studied sample is small. The number of cases followed up at the service at the beginning of data collection was 94 but the authors could only assess a lower number than expected, largely due to the difficulties in continuing the treatment that occurred during the SARS-CoV-2 pandemic.
In conclusion, individuals with OI evaluated presented important functional alterations, with a reduction in the global gross motor function and a reduction in muscle strength, affecting the mobility domain, especially individuals with OI type III. The results the authors presented here will contribute to the knowledge about the physical and functional characteristics of individuals affected by OI, favoring better planning of the therapeutic approach, and allowing the development of individualized care plans for rehabilitation and follow-up of children and adolescents with OI.
FundingThis study was carried out with the support of the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brazil (CAPES) – Finance Code 001.
The authors would like to thank the medical genetics service at Professor Edgard Santos University Hospital for encouraging and enabling research into rare diseases at the institution. To the rehabilitation unit of this hospital, for their cooperation in making data collection possible. Finally, the authors also thank the Post Graduate Program in Medicine and Health at the Universidade Federal da Bahia for its excellent academic support.