In Brazil, telemedicine was allowed as an exception during the coronavirus disease (COVID-19) pandemic. Despite its recognized value and availability, telemedicine is not universally used, suggesting that some barriers prevent its adoption and acceptance within the community. This study aims to describe the implementation of a low-cost telemedicine service in a pediatric hospital in Brazil.
MethodRetrospective descriptive study reporting the first three months (April to June 2020) of the experience of implementing a low-cost telemedicine emergency care program in a public tertiary hospital. The service was available to patients up to 18 years of age enrolled in this hospital. A tool for assessing the severity of the patient was developed, the aim of standardizing the procedure, while maintaining quality and safety. Guardian's satisfaction was assessed with a questionnaire sent after teleconsultations.
Results255 teleconsultations were carried out with 140 different patients. Of the total consultations, 182 were from 99 patients that had performed the Real-Time Polymerase Chain Reaction (RT-PCR) test for the new coronavirus (SARS-Cov-2) or had direct contact with a person known to be positive for COVID-19. Only 26 (14%) were referred to an in-person consultation. No deaths, adverse events or delayed diagnosis were recorded. 86% of the patients who answered the satisfaction questionnaire were satisfied and 92% would use telemedicine again.
ConclusionThis study presents an innovative implementation of a telemedicine program in a public and exclusively pediatric tertiary service, serving as a reference for future implementation in other public services in Brazil and developing countries.
Telemedicine has advantages over telephone communication, such as interactions in real-time while seeing and hearing each other from the comfort of patient`s homes. It can result in a higher quality of clinical approach.1–3
Telemedicine has expanded considerably over the past two decades.1,2,4 Benefits include a possibility of remote diagnosis, the ability to monitor patients with chronic diseases [5] and provision of emergency care.1,3,4 Also contributes towards reducing the number of visits to the hospital, stress due to commuting to the hospital, and hospital-related stress.1,3,4 In addition, telemedicine reduces school and work absenteeism for patients and guardians. Telehealth can promote a cost reduction and allocate resources to improve the quality of patient care.1,3,4
Pediatric remote care offers the unique opportunity and additional benefit of seeing children where they live. Through the use of telemedicine, doctors can safely observe young individuals in a calm and comfortable environment while assessing their clinical condition without the influence of additional stressors.6
Studies have shown that around 80% of telemedicine consultations between doctors and patients are being conducted properly without the need for in-person visits to the emergency department. Further, they have reported good user satisfaction.2,5
Despite its recognized value and availability, telemedicine is not universally used, suggesting that some barriers prevent its adoption and acceptance within the community.7 Some barriers to the use of telemedicine include technological challenges, workflow integration, perceived usefulness, regulatory issues and costs for the hospital services with equipment, personal and dedicated connection, and for the users, which require a minimum internet band and a computer, tablet or smartphone to be able to use this service.7 So, the inclusion of this tool in public services involves even greater challenges.
The Brazilian government and Ministry of Health, motivated by the current COVID-19 pandemic, have recently allowed the use of telemedicine services.8 The Institute is a tertiary university center, a reference for the care of pediatric patients with chronic health conditions. Although COVID-19 is not associated with severe respiratory manifestations in children,9 most patients in The Institute have comorbidities, thus being considered a risk population for COVID-19.9,10 In the pandemic scenario, telemedicine could contribute to avoiding unnecessary visits to the emergency department and for the rational use of health services. In response to the pandemic, The Hospital Telemedicine Emergency Care Program (PATMHO- “Pronto Atendimento em Telemedicina Hospitalar”, in Portuguese) was developed in the pediatric emergency department of this tertiary pediatric public hospital.
Using a severity screening score for teleconsultation can be challenging. Some screening tools have been developed to assess the severity in pediatric telecare and have demonstrated satisfactory results, reinforcing that telemedicine can be used to safely assess patients remotely. However, the majority of studies have focused on the use of screening tools for doctor-to-doctor telecare in an intensive care environment.11–13 Due to the scarcity of specific scores for pediatric teleconsultation, the authors developed a severity score specifically for this study.
In this article, the authors describe the challenges and process for implementing a telemedicine program for pediatric emergencies. The authors also present the severity score developed for the PATMHO implementation.
Additionally, preliminary results on care during the COVID-19 pandemic are discussed.
Materials and methodsStudy designThe retrospective descriptive study reporting on the first three months (April to June 2020) of the authors’ experience implementing a telemedicine emergency care program in a public tertiary hospital. The study shows preliminary data, mainly on user satisfaction.
The study was submitted and approved by the Ethics and Research Committee of the Hospital. The guardians of the patients provided oral consent before the start of the teleconsultation and were informed about the limitations associated with this form of care.
Platform and securityThe teleconsultations were carried out through Google Hangouts, a free software program with adequate safety certifications, in compliance with the Brazilian Health Insurance Portability and Responsibility Law (Lei de Portabilidade e Responsabilidade de Seguros de Saúde - HIPAA)14,15 and the Brazilian general data protection law.16
The authors use HIPAA-compliant Google Hangouts configuration. All video calls are encrypted in transit between the customer and Google and no images were recorded during the calls, ensuring privacy.14
The teleconsultation was documented in the patient's digital medical record, the same that is already used in the hospital for in-person consultations. It guarantees the safety of patient data due to the study's system has all certifications in compliance with Brazilian laws. All teleconsultations are digitally signed by the attending physician.
The teleconsultation room had a DELL ALL IN ONE Computer, Intel Core i5-8265 U Processor 8GB (1 × 8GB), DDR4, 2400 MHz HD 1 TB built-in webcam, and microphone, with Windows 10 Pro Single Language, 64 bits, associated to a 22-inch monitor, and an Epson Perfection V19 SCANNER. All of the infrastructures for the study was already available at the hospital and were relocated for use in telemedicine. Users could use any of the Google Hangouts-compatible devices (e.g., cell phone, tablet, or computer) with a camera, microphone and internet access.
The teleconsultationConsultations were carried out via video conference in real-time by a doctor from the pediatric emergency team, accompanied by a pediatric resident. The entire medical team in the emergency department, including residents, was trained and prepared for the teleconsultation.
The step-by-step instructions on how to access the telemedicine emergency care were advertised to the parents/guardians by email and through social networks.
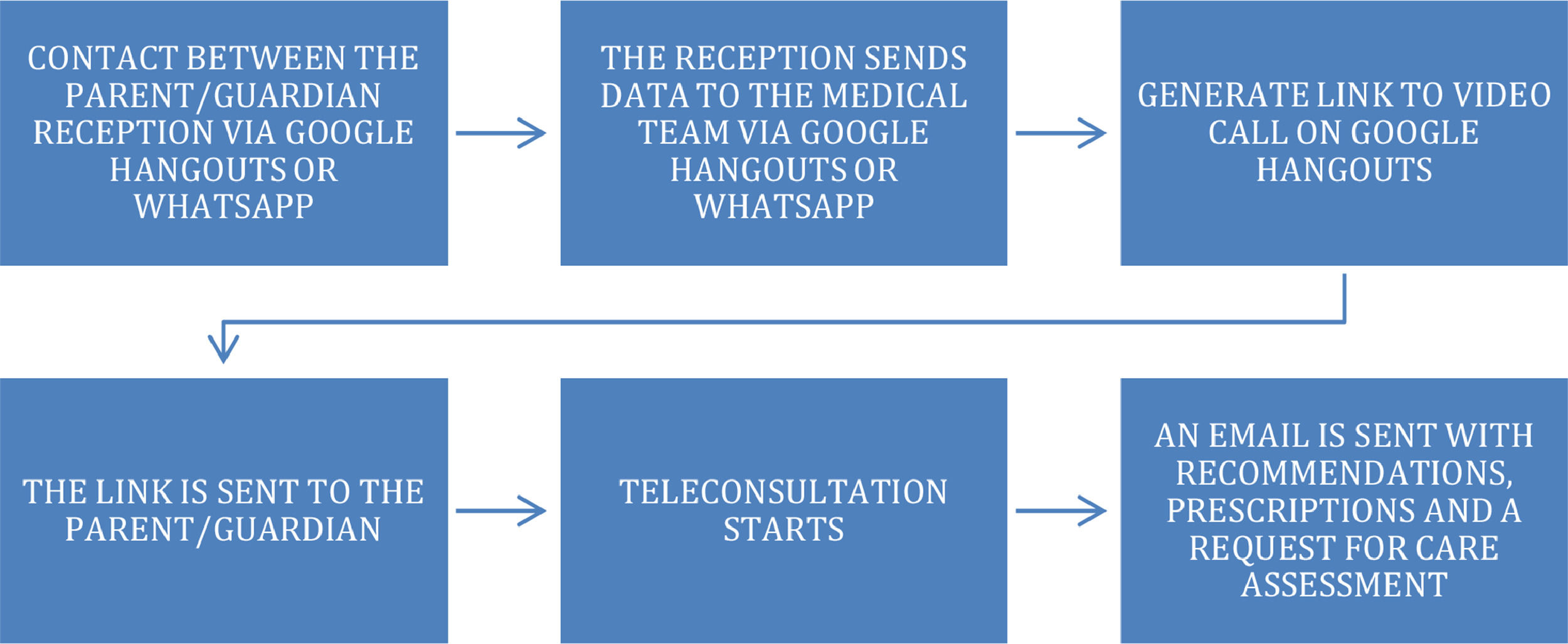
After the teleconsultation, an email was sent to the guardians, including general recommendations, medication prescriptions (if necessary), and the satisfaction questionnaire (Appendix 1). Teleconsultations were carried as indicated in Fig. 1.
Patients who were referred for reassessment through telemedicine (after being discharged from the in-person consultation) received a folder with step-by-step instructions for participating in PATMHO (Appendix 2). The parent/guardian`s mobile number was recorded, and the teleconsultation was scheduled. On the day of the consultation, the guardian contacted the hospital using Google Hangouts or the pediatric resident contacted them directly by phone or WhatsApp to remind them and helping with any access difficulties.
A follow-up could be carried out through a new teleconsultation, depending on the physician's medical judgment.
Population of studyAll patients were between the ages of 0 and 18 years of age, currently treated at inpatient or outpatient services of the study's hospital, were eligible to use PATMHO.
The patients who participated were divided into two groups: those that spontaneously sought the PATMHO services, and patients that sought in-person care and were then referred for re-evaluation through telemedicine within 48 h. They were also divided into suspected or confirmed cases of COVID-19 or other pathologies.
Evaluation of satisfactionThe email that was sent at the end of the teleconsultation included a satisfaction survey to be answered anonymously by the guardians (Appendix 1). The Telemedicine Satisfaction Questionnaire (TSQ) was adapted for the use of this study. The TSQ was developed in 2003 and has demonstrated a high level of reliability, validity, and consistency.17,18 Questions regarding the guardians, such as degree of relationship with the patient, age, and education level were included.
Development of a severity score for teleconsultationThe study's PATMHO screening score (Appendix 3) was developed based on early warning scores and the recognition of physiological changes such as the Pediatric Observation Priority Score,19 the Pediatric Assessment Triangle,20,21 the Pediatric Early Warning Score,19,20,22 and the screening score used in the Institute Emergency Department.23 This score was developed in the context of the COVID-19 pandemic, requiring future modifications.
In the study's score, the authors included comorbidities considered as a risk factor for developing severe forms of COVID-19,9 exposure to COVID-19, assessment of the level of consciousness, circulatory and respiratory assessment, and the last assessment item called potential risk of urgency.
Only considering a patient's vital signs does not seem to be the most appropriate way to identify critically ill patients in emergency departments.19–22 Assessing vital signs, such as heart rate, through teleconsultation is very difficult. Interestingly, some screening systems include the overall impression of the doctor in their classification despite the clinical diagnosis. For this last assessment item, a physician's knowledge and experience are necessary, but not sufficient. An important factor in this context is the doctor's gut instinct or sixth sense.19–22
The severity score varies from 0 to 35 points. A value greater than or equal to 5 is considered a baseline value for an emergency pediatrician to encourage the attendance of in-person emergency service. This value was determined through the consensus of specialists in pediatric emergency aiming to be more sensitive than specific. The cut point validation and evaluation of the severity score will be carried out in a future study.
Statistical analysisContinuous variables were described as means and standard deviations or as medians (variation), according to the Shapiro–Wilk test. Categorical variables were described in percentage terms. Means or medians were compared using either Student's t-test or the Mann–Whitney U test, as applicable. Categorical variables were compared using Fisher's exact test.
For all statistical tests, the significance level was set at 5% (p < 0.05). Statistical analyses were performed using SPSS software, version 22 (IBM Corporation, Armonk, NY, USA).
ResultsFrom April to June 2020, 255 teleconsultations were carried out with 140 different patients, 122 (87.1%) of which had some form of chronic disease.
Of the total consultations, 182 were from 99 patients who underwent RT-PCR exam for SARS-Cov-2 at some point or had direct contact with a person known to be positive for COVID-19. The mean age of these patients was 7.1 (± 5.7) years, ranging from 0.3 to 18 years and the female/male ratio was 1,14:1. 87 (88%) of the patients had a chronic disease.
The mean number of teleconsultations for patients tested positive for SARS-Cov-2, or in close contact with a person who received a positive RT-PCR test, was 1.7 (± 1.0) per patient, ranging from 1 to 6. 48 patients were seen through teleconsultation for one session, 32 patients received two teleconsultations, and 21 patients underwent three or more teleconsultations. Of the 182 teleconsultations, only 20 (11%) were spontaneously sought out by the patients, with the remaining being follow-up consultations after in-person consultation or hospitalization.
A higher median teleconsultation severity score was found in the teleconsultations of patients who tested positive or were in direct contact with a person with a confirmed diagnosis of COVID-19 compared to those who tested negative for SARS-Cov-2: 3 (1–7) vs 2 (0–8), p = 0.001.
Of the 182 teleconsultations, 26 (14%) were resolved with a doctor referring the patient to the emergency department for in-person care. Fifteen patients (58%) were referred in the first teleconsultation, five patients (20%) were referred in the second, three patients (11%) were referred in the third, and three patients (11%) in the fourth teleconsultation.
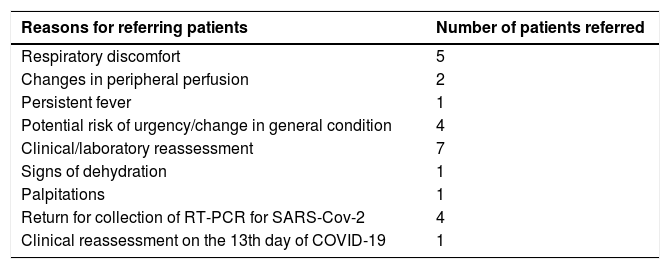
Of the patients referred for in-person consultation in the emergency department, 20 (77%) tested negative for SARS-Cov-2 and six (23%) tested positive or had direct contact with a person with confirmed COVID-19 (p = 0.03). In 14 (54%) of the 26 teleconsultations in which patients were referred to the emergency department, the individuals had a severity score greater than or equal to 5 (p < 0.001). Twelve individuals had a score less than 5 referred due to the physician's opinion or for clinical laboratory reassessment. The reasons for referring patients are shown in Table 1.
Reasons for referring patients for an in-person assessment.
Out of the 20 patients who were referred to the emergency department and tested negative, 14 patients were evaluated and discharged promptly. Although one of the patients did not attend, he was re-evaluated through telemedicine two days later and showed clinical improvement after measures taken by his mother at home. Another four patients (21%) were admitted, three in the pediatric ward and one in PICU. No deaths, adverse events, or delayed diagnosis were recorded.
Of the six patients tested who were positive or in direct contact with a person diagnosed with COVID-19, four referrals were of different patients with one patient being referred twice. Of these five individuals, only two patients (33%) were hospitalized after evaluation, both in the pediatric ward.
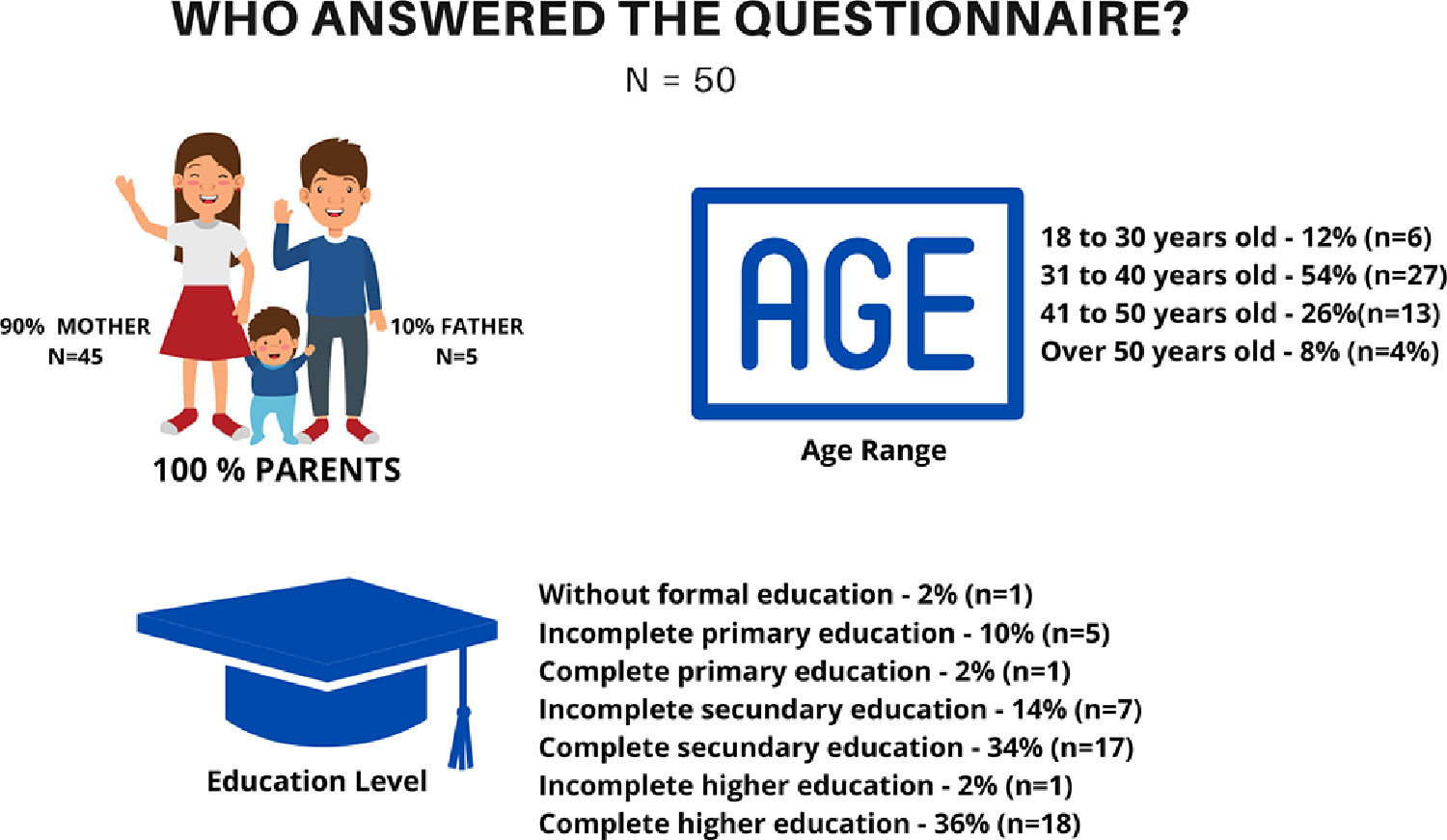
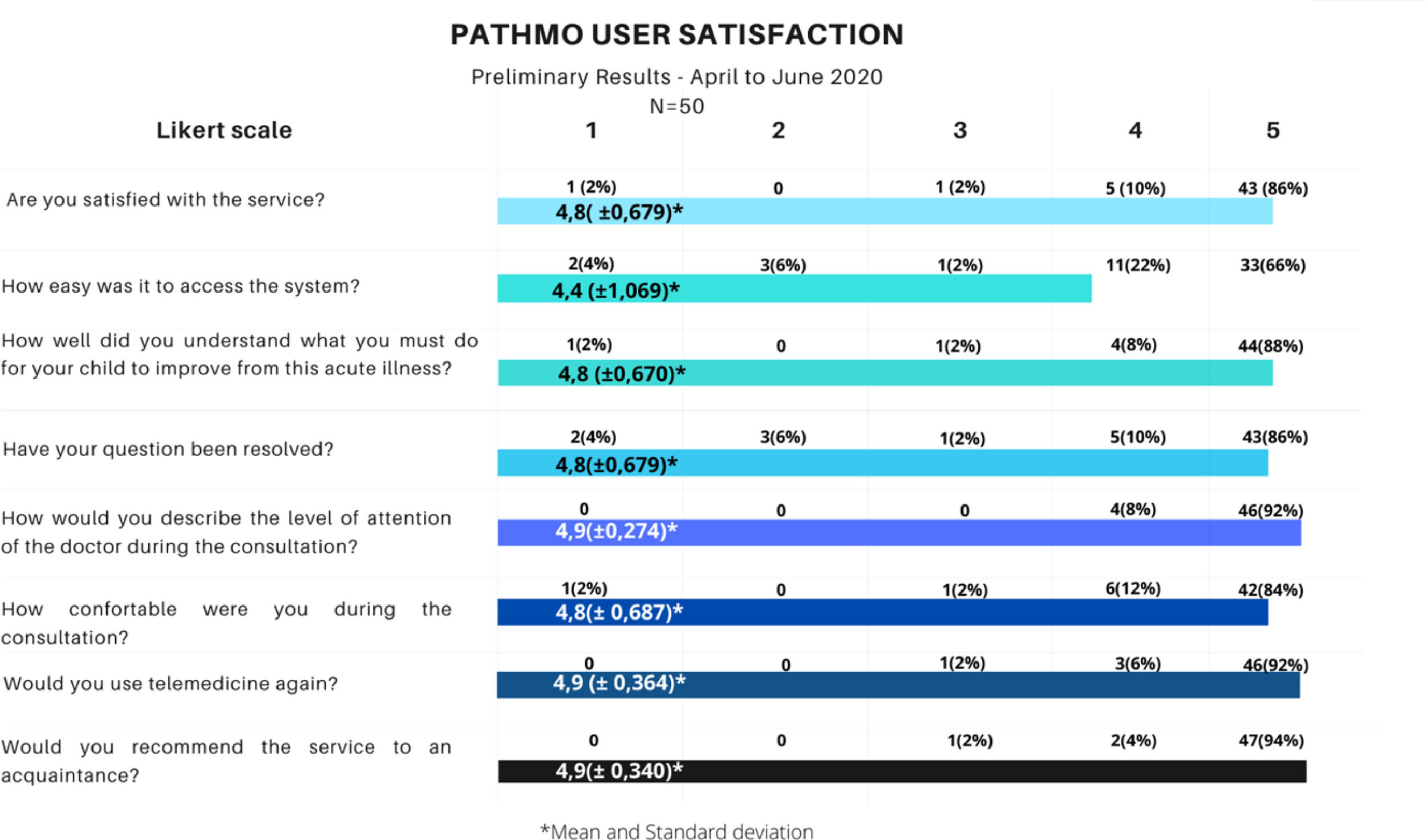
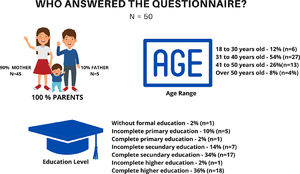
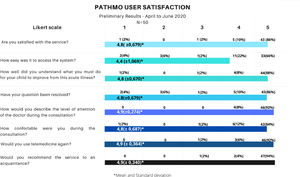
PATHMO satisfactionOf the 255 teleconsultations during April and June 2020, 50 guardians (19.6%) answered the satisfaction questionnaire (Appendix 1). 72% (n = 36) answered that it took less than 30 min to speak to the doctor, with another 16% (n = 8) waiting up to 1 hour for the teleconsultation. The demographic data of those who answered the questionnaire are described in Figure 2. Figure 3 shows the results of the satisfaction questionnaire on a Likert scale.
PATHMO user satisfaction results on a Likert scale – Question 1: 1(Not satisfied) to 5 (Totally satisfied), Question 2: 1 (It was very difficult to access the system) to 5 (It was very easy to access the system), Question 3: 1 (I do not understand what I need to do) to 5 (I definitely understand what I need to do), Question 4: 1 (None of my issues have been resolved) to 5 (All my issues have been resolved), Question 5: 1 (He / She was not attentive) to 5 (He / She was very attentive), Question 6: 1 (Not comfortable) to 5 (Completely comfortable), Question 7: 1 (I would not use telemedicine again) to 5 (I would definitely use telemedicine again), Question 8: 1 (I would not recommend) to 5 (I would definitely recommend).
Although most participants did not have any difficulties, 18% (n = 9) had reported problems with connection and 12% (n = 6) reported difficulty with the use of the application (Google Hangouts).
DiscussionTelemedicine is becoming part of medical services as the result of the growth in technology and communication.3 Although regulation surrounding telemedicine in Brazil is still restricted to the timeframe of the pandemic,8 there is a strong movement from the medical population to extend this regulation.
The implementation of telemedicine has greatly contributed to providing services during the COVID-19 pandemic. In this period, the study's service had 1041 in-person consultations, and about 24% (255 out of 1041) of the total consultations were carried out by video call. This represents a reduction in the circulation of populations at risk while allowing many patients to continue to be seen.
The leave of numerous health professionals due to the COVID-19 pandemic was a recurring problem in several health systems. Thus, the implementation of telemedicine services contributed to a reduction in the spread of the new coronavirus among the medical teams and allowed professionals in high-risk groups to work with greater security while in quarantine.24
In addition to a decrease in exposure and a reduction in the circulation of individuals during the pandemic,24 teleconsultations allowed for the ability to save in regard to patient expenses for the public health system. North American data has indicated that 76% of consultations in the emergency department could be avoided with savings of up to $733 per visit.3,25 Considering the study population as overly complex, this savings may be even greater since transport often requires advanced resources such as ambulance and oxygen transport.
The use of already available software, some of which was free (e.g., Google Hangouts and WhatsApp), and others which were already being used in the hospital (e.g., the electronic medical record where the teleconsultation was recorded), allowed for a fast, efficient, and low-cost implementation of PATMHO. Moreover, the training of the team was facilitated via software that was already part of their daily lives and was increasingly used during the pandemic.
The present study is one of the first to propose a severity score developed specifically for pediatric care through direct doctor-patient teleconsultation. The preliminary assessment of the study's severity score showed that patients were referred for in-person care in teleconsultations in which the score was higher, even with some patients remaining hospitalized. In the current context of COVID-19, the score related to the disease was included in the score, increasing the score rating in these patients.
However, from what was observed within the preliminary results, the resulting score on the question for the presence of COVID-19 does not seem to be associated with the referral of patients as most of the in-person consultations were with patients who were negative for SARS-Cov-2 or did not have direct contact with someone who had been exposed to SARS-Cov-2. The study's score will be validated in terms of the decision-making process in a future study to assess patient safety.
Comparing the present study's results of referrals for in-person care with those obtained by Haimi et al. (2020 evaluated 339 children attended by an Israeli pediatric screening service by a phone call between 2014 and 2017, the referral rate was lower (14% vs 28.3%),26 suggesting that teleconsultation may be more advantageous than consultation by telephone when it comes to assessing the need for referral of in-person emergency consultations.
Teleconsultation service was evaluated by users as practical, fast, and efficient, with a good resolution of questions and an understanding of the recommendations. A high degree of end-user satisfaction was observed in this preliminary phase of the present study. A retrospective cohort study conducted in New York during the pandemic also showed a high degree of patient satisfaction in medical service through the use of video,27 which reinforces the importance of PATMHO now that there is a global concern on exposure to COVID-19. Connection difficulties were the greatest challenge faced by end-users, exposing the need for investment in technology and greater digital inclusion of the Brazilian population.28
The limitations of the study in this preliminary phase include a small population sample and complex health needs. Most of the teleconsultations were a follow-up meeting involving a reassessment. As it is a new service, there was a low investment in advertising, with spontaneous demand being low. However, the aim is for growth in all remote medical services post-pandemic, which most likely will also happen with emergency-related care.
Moreover, the implementation of telemedicine services within medical residency creates a teaching environment, enabling the introduction of telemedicine as part of the medical residency program in pediatrics, pediatric emergencies, or even as part of undergraduate education. Two systematic reviews on telemedicine education and training, one from 201629 and another from 2020,30 demonstrate that the literature on this subject is limited and requires greater exploration.
ConclusionThis study presents an innovative implementation of a telemedicine program in a public and exclusively pediatric tertiary service. The program developed was low cost, generated great satisfaction in guardians, and increased patient safety. In this way, PATMHO may serve as a reference for other public services in Brazil and other developing countries.
The present study's preliminary results are encouraging and demonstrate the potential of the program. Further studies are needed to demonstrate the benefits in populations with different health needs, the impact of telemedicine health services over a longer period of time, and the use of this service outside of the COVID-19 pandemic.